Changes in Health State Utility Values in Japanese Patients with End-Stage Breast Cancer
Abstract
:1. Introduction
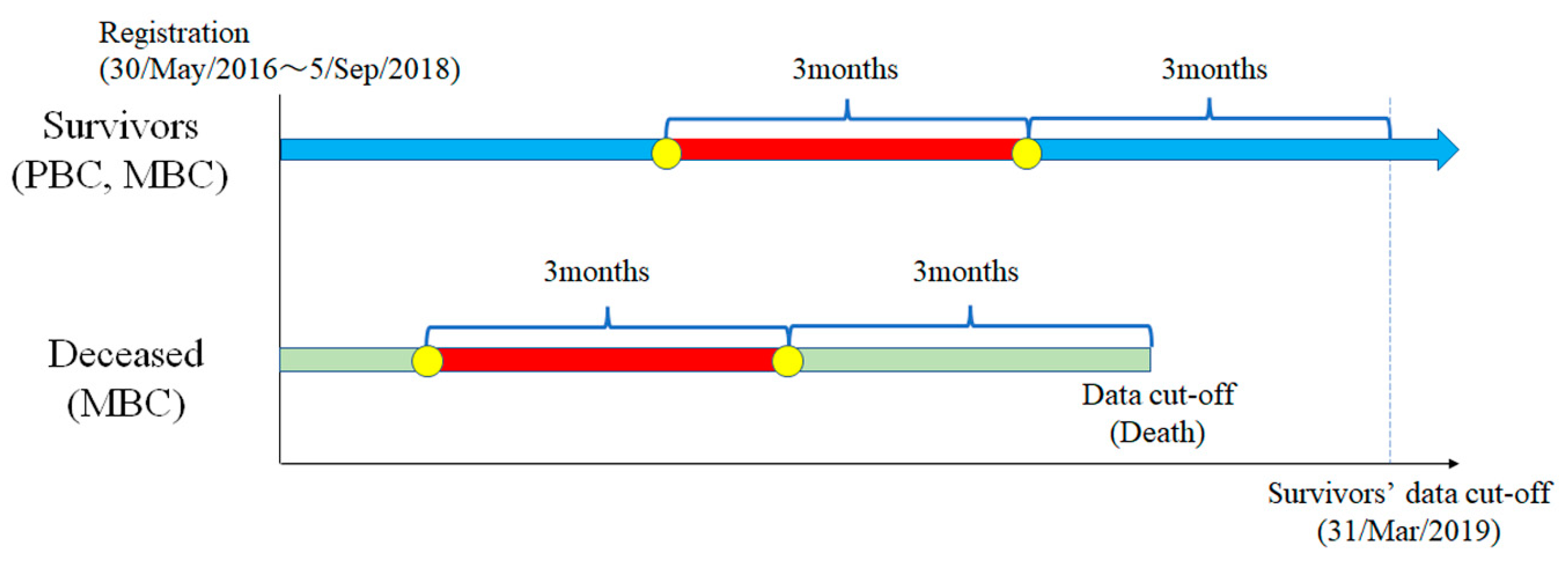
2. Materials and Methods
2.1. A Prospective Cohort Database of HSUVs for Japanese Breast Cancer Patients
2.2. Preference-Based Measurement for Calculating HSUVs
2.3. Transition in HSUVs in Japanese Patients with Breast Cancer
2.4. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Cancer Statistics. Available online: https://ganjoho.jp/reg_stat/statistics/data/dl/index.html#a14 (accessed on 18 March 2021).
- Yashkin, A.P.; Greenup, R.A.; Gorbunova, G.; Akushevich, I.; Oeffinger, K.C.; Hwang, E.S. Outcomes and costs for women after breast cancer: Preparing for improved survivorship of medicare beneficiaries. JCO Oncol. Pract. 2021, 17, e469–e478. [Google Scholar] [CrossRef]
- Tartari, F.; Santoni, M.; Pistelli, M.; Berardi, R. Healthcare cost of HER2-positive and negative breast tumors in the United States (2012–2035). Cancer Treat. Rev. 2017, 60, 12–17. [Google Scholar] [CrossRef]
- Iragorri, N.; de Oliveira, C.; Fitzgerald, N.; Essue, B. The out-of-pocket cost burden of cancer care–A systematic literature review. Curr. Oncol. 2021, 28, 1216–1248. [Google Scholar] [CrossRef]
- Shiroiwa, T.; Fukuda, T.; Ikeda, S.; Takura, T. New decision-making processes for the pricing of health technologies in Japan: The FY 2016/2017 pilot phase for the introduction of economic evaluations. Health Policy 2017, 121, 836–841. [Google Scholar] [CrossRef] [PubMed]
- Sugawara, T. Specific Utilization Method of Medical Economic Evaluation—Procedure and Analysis Method for Calculating Economic Evaluation in HTA; Technical Information Institute: Tokyo, Japan, 2014; pp. 16–22. [Google Scholar]
- Herdman, M.; Gudex, C.; Lloyd, A.; Janssen, M.F.; Kind, P.; Parkin, D.; Bonsel, G.; Badia, X. Development and preliminary testing of the new five-level version of EQ-5D (EQ-5D-5L). Qual. Life Res. 2011, 20, 1727–1736. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shiroiwa, T.; Fukuda, T.; Ikeda, S.; Takura, T.; Moriwaki, K. Development of an official guideline for the economic evaluation of drugs/medical devices in Japan. Value Health 2017, 20, 372–378. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Earle, C.C.; Chapman, R.H.; Baker, C.S.; Bell, C.M.; Stone, P.W.; Sandberg, E.A.; Neumann, P.J. Systematic overview of cost-utility assessments in oncology. J. Clin. Oncol. 2000, 18, 3302–3317. [Google Scholar] [CrossRef]
- Peasgood, T.; Ward, S.E.; Brazier, J. Health-state utility values in breast cancer. Expert Rev. Pharmacoecon. Outcomes Res. 2010, 10, 553–566. [Google Scholar] [CrossRef]
- Shih, V.; Chan, A.; Xie, F.; Ko, Y. Health state utility assessment for breast cancer. Value Health Reg. Issues 2012, 1, 93–97. [Google Scholar] [CrossRef] [Green Version]
- Kuchuk, I.; Bouganim, N.; Beusterien, K.; Grinspan, J.; Vandermeer, L.; Gertler, S.; Dent, S.F.; Song, X.; Segal, R.; Mazzarello, S.; et al. Preference weights for chemotherapy side effects from the perspective of women with breast cancer. Breast Cancer Res. Treat. 2013, 142, 101–107. [Google Scholar] [CrossRef]
- Tachi, T.; Teramachi, H.; Tanaka, K.; Asano, S.; Osawa, T.; Kawashima, A.; Yasuda, M.; Mizui, T.; Nakada, T.; Noguchi, Y.; et al. The impact of outpatient chemotherapy-related adverse events on the quality of life of breast cancer patients. PLoS ONE 2015, 10, e0124169. [Google Scholar] [CrossRef]
- Brown, D.S.; Trogdon, J.G.; Ekwueme, D.U.; Chamiec-Case, L.; Guy Jr, G.P.; Tangka, F.K.; Li, C.; Trivers, K.F.; Rodriguez, J.L. Health state utility impact of breast cancer in U.S. women aged 18-44 years. Am. J. Prev. Med. 2016, 50, 255–261. [Google Scholar] [CrossRef]
- Trogdon, J.G.; Ekwueme, D.U.; Chamiec-Case, L.; Guy, G.P., Jr. Breast cancer in young women: Health state utility impacts by race/ethnicity. Am. J. Prev. Med. 2016, 50, 262–269. [Google Scholar] [CrossRef] [Green Version]
- Paracha, N.; Thuresson, P.O.; Moreno, S.G.; MacGilchrist, K.S. Health state utility values in locally advanced and metastatic breast cancer by treatment line: A systematic review. Expert Rev. Pharmacoecon. Outcomes Res. 2016, 16, 549–559. [Google Scholar] [CrossRef]
- Hao, Y.; Wolfram, V.; Cook, J. A structured review of health utility measures and elicitation in advanced/metastatic breast cancer. Clinicoecon. Outcomes Res. 2016, 8, 293–303. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hagiwara, Y.; Shiroiwa, T.; Shimozuma, K.; Kawahara, T.; Uemura, Y.; Watanabe, T.; Taira, N.; Fukuda, T.; Ohashi, Y.; Mukai, H. Impact of adverse events on health utility and health-related quality of life in patients receiving first-line chemotherapy for metastatic breast cancer: Results from the SELECT BC study. Pharmacoeconomics 2018, 36, 215–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chou, T.C.; Chiang, S.C.; Ko, Y. Health state utilities for metastatic breast cancer in Taiwan. Breast 2020, 51, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Criscitiello, C.; Spurden, D.; Piercy, J.; Rider, A.; Williams, R.; Mitra, D.; Wild, R.; Corsaro, M.; Kurosky, S.K.; Law, E.H. Health-related quality of life among patients with HR+/HER2- early breast cancer. Clin. Ther. 2021, S0149–S2918. [Google Scholar] [CrossRef]
- Pourrahmat, M.M.; Kim, A.; Kansal, A.R.; Hux, M.; Pushkarna, D.; Fazeli, M.S.; Chung, K.C. Health state utility values by cancer stage: A systematic literature review. Eur. J. Health Econ. 2021. [Google Scholar] [CrossRef]
- Haslam, A.; Herrera-Perez, D.; Gill, J.; Prasad, V. Patient experience captured by quality-of-life measurement in oncology clinical trials. JAMA Netw. Open 2020, 3, e200363. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sagara, Y.; Mori, M.; Yamamoto, S.; Eguchi, K.; Iwatani, T.; Naito, Y.; Kogawa, T.; Tanaka, K.; Kotani, H.; Yasojima, H.; et al. Current status of advance care planning and end-of-life communication for patients with advanced and metastatic breast cancer. Oncologist 2021, 26, e686–e693. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Shi, J.F.; Zhu, J.; Huang, H.Y.; Bai, Y.N.; Liu, G.X.; Liao, X.Z.; Mao, A.Y.; Ren, J.S.; Sun, X.J.; et al. Health Economic Evaluation Working Group of the Cancer Screening Program in Urban China. Health-related quality of life and utility scores of patients with breast neoplasms in China: A multicenter cross-sectional survey. Breast 2018, 39, 53–62. [Google Scholar] [CrossRef] [PubMed]
- Hildebrandt, T.; Thiel, F.C.; Fasching, P.A.; Graf, C.; Bani, M.R.; Loehberg, C.R.; Schrauder, M.G.; Jud, S.M.; Hack, C.C.; Beckmann, M.W.; et al. Health utilities in gynecological oncology and mastology in Germany. Anticancer Res. 2014, 34, 829–835. [Google Scholar] [PubMed]
- Chie, W.C.; Huang, C.S.; Chen, J.H.; Chang, K.J. Utility assessment for different clinical phases of breast cancer in Taiwan. J Formos. Med. Assoc. 2000, 99, 677–683. [Google Scholar] [PubMed]




| Variable Patients | (n = 137) | |
|---|---|---|
| Age (years), Mean ± SD (Range) | 56.0 ± 11.16 (32–86) | |
| Histopathological types | n | % |
| Ductal carcinoma in situ | 13 | 9.6 |
| Invasive ductal carcinoma | 102 | 75.0 |
| Invasive lobular carcinoma | 11 | 8.1 |
| Others | 10 | 7.3 |
| Breast cancer subtypes | n | % |
| HR+/HER2– (luminal) | 102 | 74.5 |
| HR–/HER2+ (HER2) | 7 | 5.1 |
| HR+/HER2+ (luminal–HER2) | 18 | 13.1 |
| HR–/HER2− (triple-negative) | 10 | 7.3 |
| Stage | n | % |
| 0 | 13 | 9.5 |
| І | 59 | 43.0 |
| ІІA | 36 | 26.3 |
| ІІB | 17 | 12.4 |
| ІІІA | 6 | 4.4 |
| ІІІB | 3 | 2.2 |
| ІІІC | 3 | 2.2 |
| Variable Patients | (n = 44) | |
|---|---|---|
| Age (years), Mean ± SD (Range) | 57.4 ± 11.6 (29–80) | |
| Breast cancer subtypes | n | % |
| HR+/HER2– (luminal) | 30 | 68.1 |
| HR–/HER2+ (HER2) | 4 | 9.1 |
| HR+/HER2+ (luminal–HER2) | 4 | 9.1 |
| HR–/HER2− (triple-negative) | 5 | 11.1 |
| Unknown | 1 | 2.3 |
| Number of metastatic organs | n | % |
| 1 | 19 | 46.3 |
| 2 | 7 | 17.1 |
| ≥3 | 15 | 36.6 |
| Potentially life-threatening organ metastases (liver, lung, brain) | n | % |
| + | 27 | 61.4 |
| − | 17 | 38.6 |
| Metastatic organs (including duplicates) | n | % |
| Liver | 13 | 29.5 |
| Lung | 17 | 38.6 |
| Brain | 4 | 9.1 |
| Bone | 16 | 36.4 |
| Distant LNs | 17 | 38.6 |
| Breast/skin | 22 | 50.0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Iwatani, T.; Noto, S.; Tsugawa, K. Changes in Health State Utility Values in Japanese Patients with End-Stage Breast Cancer. Curr. Oncol. 2021, 28, 4203-4212. https://doi.org/10.3390/curroncol28050356
Iwatani T, Noto S, Tsugawa K. Changes in Health State Utility Values in Japanese Patients with End-Stage Breast Cancer. Current Oncology. 2021; 28(5):4203-4212. https://doi.org/10.3390/curroncol28050356
Chicago/Turabian StyleIwatani, Tsuguo, Shinichi Noto, and Koichiro Tsugawa. 2021. "Changes in Health State Utility Values in Japanese Patients with End-Stage Breast Cancer" Current Oncology 28, no. 5: 4203-4212. https://doi.org/10.3390/curroncol28050356
APA StyleIwatani, T., Noto, S., & Tsugawa, K. (2021). Changes in Health State Utility Values in Japanese Patients with End-Stage Breast Cancer. Current Oncology, 28(5), 4203-4212. https://doi.org/10.3390/curroncol28050356





