Comparison of Patient-Reported Experience of Patients Receiving Radiotherapy Measured by Two Validated Surveys
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Patient-Reported Experience Measures
2.3. Outcome Definition
2.4. Statistical Analyses
3. Results
3.1. Sample
3.2. Patient Characteristics
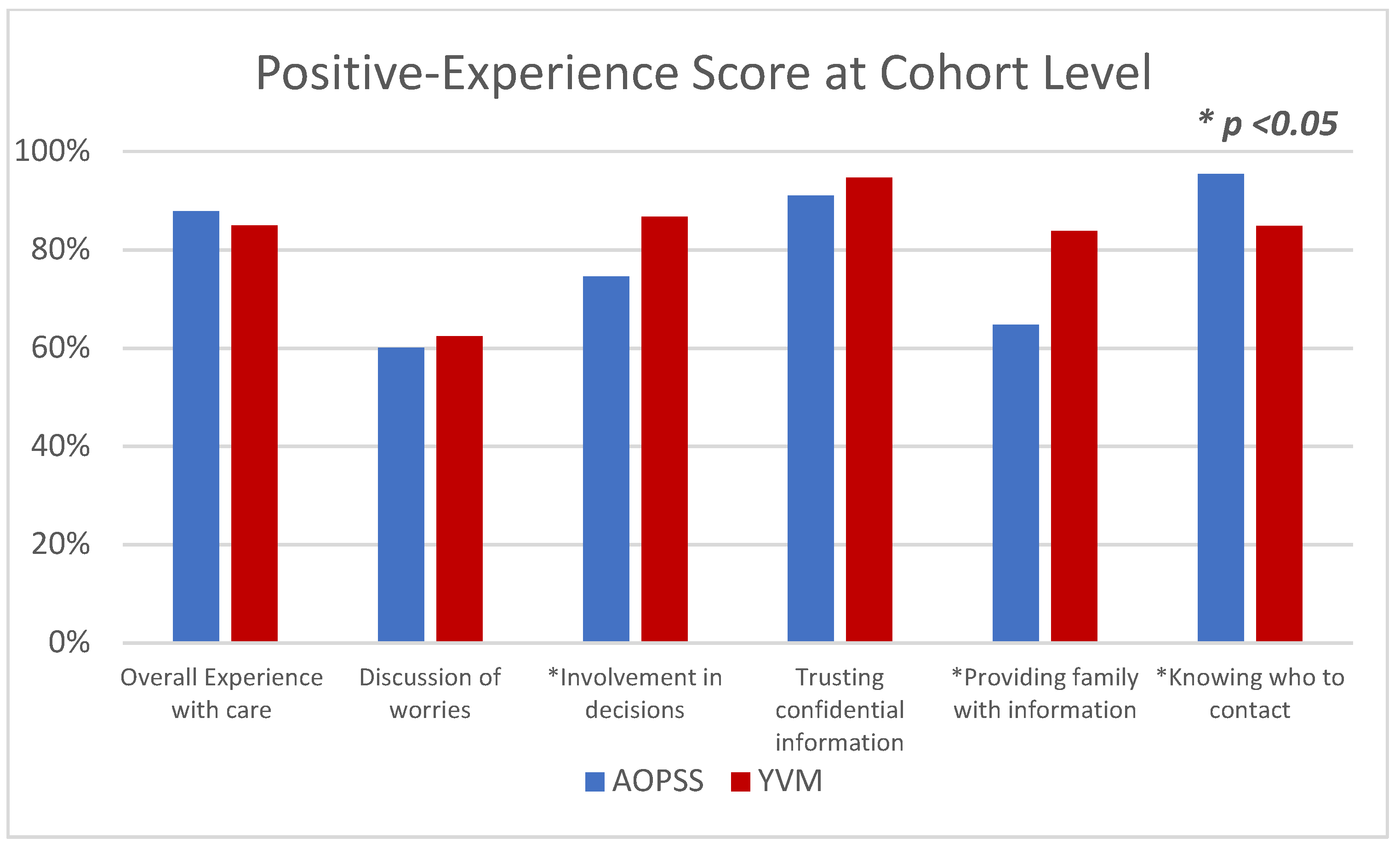
3.3. Positive Experience at the Cohort Level
3.4. Positive Experience at the Tumor Groups Level
3.5. Association between Positive Experience and the Covariates within Each Cohort
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Doyle, C.; Lennox, L.; Bell, D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 2013, 3, e001570. [Google Scholar] [CrossRef] [PubMed]
- Anhang Price, R.; Elliott, M.N.; Zaslavsky, A.M.; Hays, R.D.; Lehrman, W.G.; Rybowski, L.; Edgman-Levitan, S.; Cleary, P.D. Examining the role of patient experience surveys in measuring health care quality. Med. Care Res. Rev. 2014, 71, 522–554. [Google Scholar] [CrossRef]
- Fenton, J.J.; Jerant, A.F.; Bertakis, K.D.; Franks, P. The cost of satisfaction: A national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch. Intern. Med. 2012, 172, 405–411. [Google Scholar] [CrossRef]
- Isaac, T.; Zaslavsky, A.M.; Cleary, P.D.; Landon, B.E. The relationship between patients’ perception of care and measures of hospital quality and safety. Health Serv. Res. 2010, 45, 1024–1040. [Google Scholar] [CrossRef] [PubMed]
- Biondi, E.A.; Hall, M.; Leonard, M.S.; Pirraglia, P.A.; Alverson, B.K. Association between resource utilization and patient satisfaction at a tertiary care medical center. J. Hosp. Med. 2016, 11, 785–791. [Google Scholar] [CrossRef] [PubMed]
- The Beryl Institute. Defining Patient Experience [internet]. Available online: https://www.theberylinstitute.org/page/DefiningPatientExp (accessed on 19 February 2021).
- Coronado, A.C.; Tran, K.; Chadder, J.; Niu, J.; Fung, S.; Louzado, C.; Rahal, R. The experience of patients with cancer during diagnosis and treatment planning: A descriptive study of Canadian survey results. Curr. Oncol. 2017, 24, 332–337. [Google Scholar] [CrossRef]
- Comerford, D.; Shah, R. Ambulatory approach to cancer care. Part 1: The patient experience. Br. J. Nurs. 2018, 27, S4–S12. [Google Scholar] [CrossRef] [PubMed]
- Canadian Partnership against Cancer. The Canadian Strategy for Cancer Control: 2017–2022. Available online: https://www.partnershipagainstcancer.ca/wp-content/uploads/2016/02/canadian-strategy-cancer-control-2017-2022-en.pdf (accessed on 19 February 2021).
- The CAHPS Improvement Guide. Available online: https://www.ahrq.gov/sites/default/files/wysiwyg/cahps/quality-improvement/improvement-guide/2-why-improve/cahps-section-2-why-improve-patient-experience.pdf (accessed on 19 February 2021).
- Organization for Economic Co-operation and Development. Health Care Quality Indicators—Responsiveness and Patient Experiences. 2018. Available online: http://www.oecd.org/els/health-systems/hcqi-responsiveness-and-patient-experiences.htm (accessed on 19 February 2021).
- Kingsley, C.; Patel, S. Patient-reported outcome measures and patient-reported experience measures. BJA Educ. 2017, 17, 137–144. [Google Scholar] [CrossRef]
- National Research Corporation. Development and Validation of the Picker Ambulatory Oncology Survey Instrument in Canada; National Research Corporation: Lincoln, NE, USA, 2003; Available online: https://nrchealth.com/nrc-health-canada/ (accessed on 19 February 2021).
- Your Voice Matters, Patient-Reported Experience Measure. Ontario Health (Cancer Care Ontario). Available online: https://www.cancercareontario.ca/en/cancer-care-ontario/programs/clinical-services/patient-family-engagement-experience/your-voice-matters (accessed on 19 February 2021).
- Gesell, S.B.; Gregory, N. Identifying priority actions for improving patient satisfaction with outpatient cancer care. J. Nurs. Care Qual. 2004, 19, 226–233. [Google Scholar] [CrossRef] [PubMed]
- Rozario, D. How well do we do what we do, and how do we know it? The importance of patient-reported experience measures in assessing our patients’ experience of care. Can. J. Surg. 2019, 62, E7–E9. [Google Scholar] [CrossRef]
- Fradgley, E.A.; Paul, C.L.; Bryant, J.; Oldmeadow, C. Getting right to the point: Identifying Australian outpatients’ priorities and preferences for patient-centred quality improvement in chronic disease care. Int. J. Qual. Health Care. 2016, 28, 470–477. [Google Scholar] [CrossRef]
- Tremblay, D.; Roberge, D.; Berbiche, D. Determinants of patient-reported experience of cancer services responsiveness. BMC Health Serv. Res. 2015, 15, 425. [Google Scholar] [CrossRef] [PubMed]
- Fitch, M.I.; Coronado, A.C.; Schippke, J.C.; Chadder, J.; Green, E. Exploring the perspectives of patients about their care experience: Identifying what patients perceive are important qualities in cancer care. Support. Care Cancer 2020, 28, 2299–2309. [Google Scholar] [CrossRef]
- Loiselle, C.G. Cancer information-seeking preferences linked to distinct patient experiences and differential satisfaction with cancer care. Patient Educ. Couns. 2019, 102, 1187–1193. [Google Scholar] [CrossRef]
- Bridge, E.; Conn, L.G.; Dhanju, S.; Singh, S.; Moody, L. The patient experience of ambulatory cancer treatment: A descriptive study. Curr. Oncol. 2019, 26, e482–e493. [Google Scholar] [CrossRef] [PubMed]
- Wiig, S.; Storm, M.; Aase, K.; Gjestsen, M.T.; Solheim, M.; Harthug, S.; Robert, G.; Fulop, N. Investigating the use of patient involvement and patient experience in quality improvement in Norway: Rhetoric or reality? BMC Health Serv. Res. 2013, 13, 206. [Google Scholar] [CrossRef] [PubMed]
- Patient-Centered Radiation Oncology Service Enhancement (PROSE). Available online: https://www.proseprogram.ca (accessed on 30 March 2021).
- Turner, J.; Kelly, B. Emotional dimensions of chronic disease. West J. Med. 2000, 172, 124–128. [Google Scholar] [CrossRef]
- Manary, M.P.; Boulding, W.; Staelin, R.; Glickman, S.W. The patient experience and health outcomes. N. Engl. J. Med. 2013, 368, 201–203. [Google Scholar] [CrossRef]
- LaVela, S.L.; Gallan, A.S. Evaluation and measurement of patient experience. Patient Exp. J. 2014, 1, 28–36. [Google Scholar] [CrossRef]
- Bjertnaes, O.A. The association between survey timing and patient-reported experiences with hospitals: Results of a national postal survey. BMC Med. Res. Methodol. 2012, 12, 13. [Google Scholar] [CrossRef]
- Brédart, A.; Razavi, D.; Robertson, C.; Brignone, S.; Fonzo, D.; Petit, J.Y.; De Haes, J.C.J.M. Timing of patient satisfaction assessment: Effect on questionnaire acceptability, completeness of data, reliability and variability of scores. Patient Educ. Couns. 2002, 46, 131–136. [Google Scholar] [CrossRef]
- Stevens, M.; Reininga, I.H.; Boss, N.A.; van Horn, J.R. Patient satisfaction at and after discharge. Effect of a time lag. Patient Educ. Couns. 2006, 60, 241–245. [Google Scholar] [CrossRef][Green Version]
- Lemos, P.; Pinto, A.; Morais, G.; Pereira, J.; Loureiro, R.; Teixeira, S.; Nunes, C.S. Patient satisfaction following day surgery. J. Clin. Anesth. 2009, 21, 200–205. [Google Scholar] [CrossRef] [PubMed]
- Taylor, N.G.; Tollafield, D.R.; Rees, S. Does patient satisfaction with foot surgery change over time? Foot (Edinb). 2008, 18, 68–74, Erratum in 2008, 18, 179. [Google Scholar] [CrossRef] [PubMed]
- Bendall-Lyon, D.; Powers, T.L.; Swan, J.E. Time does not heal all wounds. Patients report lower satisfaction levels as time goes by. Mark. Health Serv. 2001, 21, 10–14. [Google Scholar]
- Watson, L.; Qi, S.; Photitai, E.; DeIure, A. A Cross-Sectional Analysis of Ambulatory Oncology Experience by Treatment Intent. Curr. Oncol. 2020, 28, 98–106. [Google Scholar] [CrossRef] [PubMed]

| Items | AOPSS | YVM |
|---|---|---|
| Data collection | Retrospective | Real time |
| Location where the PREM was completed | Home | Hospital |
| PREM type | Paper | Electronic |
| Assessment of experience over a period of | within six months | within the last outpatient visit (recorded in real time) |
| Healthcare services assessed | Multiple services that the patient might have interacted with including radiotherapy | One service (radiotherapy) |
| Number of questions in the PREM | 97 questions | 28 main questions with some having sub-questions |
| Items | AOPSS | YVM |
|---|---|---|
| OEDW | Overall, how would you rate your quality of care in the past six months? If you had any worries or concerns before beginning your treatment, did your care provider discuss them with you? | On a scale of excellent to poor, how would you rate the following…? Your overall experience with your last visit? Please think of one of the providers you met with today and identified in Question 13. On a scale of excellent to poor, how would you rate this doctor/healthcare provider on the following…? Discussed your emotional worries and concerns? |
| ID | Were you involved in decisions about your care as much as you wanted? | Please think of one of the providers you met with today and identified in Question 13. On a scale of excellent to poor, how would you rate this doctor/healthcare provider on the following…? Involved you in decisions about your care in the way you wanted? |
| TC | Did you feel you could trust your care providers with confidential information? | On a scale of excellent to poor, how would you rate the following….? Your overall confidence that the people in the clinic treat your health information with privacy/confidentiality? |
| PI KC | Did your care providers give your family or someone close to you all the information they needed to support you in your care and recovery? Did you know whom to talk to when you had any questions or concerns? | On a scale of excellent to poor, how would you rate the following….? Your overall confidence that the clinic provided your family/caregiver with the information they wanted about your care? On a scale of excellent to poor, how would you rate the following….? Your overall confidence that the clinic ensured that you know who to contact if you have any questions or concerns after your most recent visit? |
| Items | Surveyed Cohorts | ||
|---|---|---|---|
| AOPSS (N = 220) | YVM (N = 200) | p | |
| Age groups <50 51–70 ≥71 | 31 (14%) 114 (52%) 75 (34%) | 41 (21%) 104 (52%) 51 (26%) | 0.080 |
| Sex Female Male | 128 (58%) 92 (42%) | 103 (52%) 97 (49%) | 0.169 |
| Education levels Up to high school graduate College, trade, or technical school University degree and/or more | 81 (37%) 64 (29%) 62 (28%) | 62 (31%) 54 (27%) 66 (33%) | 0.387 |
| Tumor groups Breast Genitourinary Gastrointestinal Lung Other | 72 (33%) 38 (17%) 25 (11%) 26 (12%) 59 (27%) | 28 (14%) 27 (14%) 37 (19%) 27 (14%) 81 (41%) | <0.001 |
| Items | Overall Experience with Care | Discussion of Worries | Involvement in Decisions | Trusting Providers with Confidential Information | Providing Family with Information | Knowing Who to Contact | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Reference Level | AOPSS OR (95% CI) | YVM OR (95% CI) | AOPSS OR (95% CI) | YVM OR (95% CI) | AOPSS OR (95% CI) | YVM OR (95% CI) | AOPSS OR (95% CI) | YVM OR (95% CI) | AOPSS OR (95% CI) | YVM OR (95% CI) | AOPSS OR (95% CI) | YVM OR (95% CI) | |
| Age group | |||||||||||||
| <50 | ≥71 | 0.5 (0.1–2.2) | 0.6 (0.2–2.7) | 1.6 (0.6–4.3) | 0.3 (0.1–1.2) | 0.5 (0.2–1.4) | 0.4 (0.1–2.4) | 0.2 (0.03–1.2) | 0.5 (0.05–4.6) | 0.8 (0.3–2.1) | 0.5 (0.1–2.2) | NA | 0.37 |
| 51–70 | 0.9 (0.3–2.6) | 0.7 (0.2–2.2) | 1.7 (0.8–3.6) | 0.7 (0.2–2) | 0.9 (0.4–1.9) | 0.4 (0.1–1.6) | 0.4 (0.1–1.6) | 0.4 (0.7–2.3) | 0.7 (0.3–1.5) | 0.7 (0.2–2.4) | 2 (0.1–35) | 0.38 | |
| Sex | |||||||||||||
| Female | Male | 1.4 (0.5–4.3) | 0.97 (0.3–2.8) | 2.3 (0.3–6.4) | 1.1 (0.5–2.7) | 0.8 (0.3–2.1) | 0.6 (0.2–1.9) | 0.3 (0.03–1.9) | 1.1 (0.2–5.1) | 0.7 (0.3–1.7) | 0.7 (0.2–1.9) | NA | 0.5 (0.2–1.6) |
| Education level | |||||||||||||
| College | Up to high school | 2 (0.6–6.9) | 2.5 (0.8–8.2) | 2.4 (1.04–5.3) | 3.2 (1.1–9.1) | 1.97 (0.9–4.5) | 2 (0.5–7.5) | 5.6 (1.1–28.4) | 1.2 (0.2–6.5) | 1.6 (0.7–3.5) | 2 (0.6–7.1) | NA | 1.6 (0.4–6.8) |
| University or more | 1.1 (0.4–3.4) | 2.96 (0.9–9.7) | 0.99 (0.4–2.2) | 2.3 (0.7–6.7) | 1.8 (0.8–4.2) | 1.8 (0.5–6.2) | 3.1 (0.9–11.2) | 1.8 (0.4–9.5) | 0.7 (0.3–1.5) | 2.5 (0.7–8.6) | NA | 0.7 (0.2–2.4) | |
| Tumor group | |||||||||||||
| Breast | Lung | 4.98 (0.7–38) | 3.0 (0.6–16.1) | 0.6 (0.1–2.3) | 4.3 (0.9–19.5) | 3.3 (0.9–11.8) | 6.7 (1.04–43) | NA | 2.1 (0.2–17.1) | 0.98 (0.3–3.3) | 5.9 (0.9–37.6) | NA | 5.6 (1.01–31) |
| GI | 1.4 (0.2–8.1) | 11 (1.2–103) | 0.7 (0.2–2.9) | 1.5 (0.4–5.9) | 0.6 (0.2–2) | 14.2 (1.5–136) | NA | 2.8 (0.4–19.9) | 0.2 (0.1–1.5) | 6.8 (1.1–41) | NA | 6.2 (1.2–31.5) | |
| GU | 1.99 (0.3–12.2) | 2.1 (0.4–12) | 1.6 (0.3–5) | 1.5 (0.3–8) | 0.9 (0.2–3.1) | 3.2 (0.5–21.9) | NA | 4.4 (0.3–59.9) | 0.94 (0.2–3.7) | 3 (0.5–21) | NA | 7.03 (0.6–77.6) | |
| Other | 0.6 (0.1–2.6) | 1.4 (0.4–5.1) | 0.4 (0.1–1.4) | 2.4 (0.7–8.8) | 1.2 (0.4–3.7) | 2.2 (0.6–8.2) | NA | 4 (0.6–26) | 0.7 (0.2–2.2) | 1.8 (0.5–6.6) | 5.4 | 3.4 (0.9–13.1) | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Al-Rashdan, A.; Watson, L.; Yannitsos, D.; Qi, S.; Grendarova, P.; Barbera, L. Comparison of Patient-Reported Experience of Patients Receiving Radiotherapy Measured by Two Validated Surveys. Curr. Oncol. 2021, 28, 2180-2189. https://doi.org/10.3390/curroncol28030202
Al-Rashdan A, Watson L, Yannitsos D, Qi S, Grendarova P, Barbera L. Comparison of Patient-Reported Experience of Patients Receiving Radiotherapy Measured by Two Validated Surveys. Current Oncology. 2021; 28(3):2180-2189. https://doi.org/10.3390/curroncol28030202
Chicago/Turabian StyleAl-Rashdan, Abdulla, Linda Watson, Demetra Yannitsos, Siwei Qi, Petra Grendarova, and Lisa Barbera. 2021. "Comparison of Patient-Reported Experience of Patients Receiving Radiotherapy Measured by Two Validated Surveys" Current Oncology 28, no. 3: 2180-2189. https://doi.org/10.3390/curroncol28030202
APA StyleAl-Rashdan, A., Watson, L., Yannitsos, D., Qi, S., Grendarova, P., & Barbera, L. (2021). Comparison of Patient-Reported Experience of Patients Receiving Radiotherapy Measured by Two Validated Surveys. Current Oncology, 28(3), 2180-2189. https://doi.org/10.3390/curroncol28030202





