Out-of-Pocket Costs and Perceived Financial Burden Associated with Prostate Cancer Treatment in a Quebec Remote Area: A Cross-Sectional Study
Abstract
1. Introduction
2. Methods
2.1. Study Setting and Sample
2.2. Questionnaire and Variables
2.3. Statistical Analysis
3. Results
3.1. Out-of-Pocket Costs
3.2. Absences from Work
3.3. Perceived Financial Burden and Associated Factors
4. Discussion
4.1. Out-of-Pocket Costs
4.2. Absence from Work
4.3. Perceived Financial Burden and Associated Factors
4.4. Implications
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ferlay, J.; Ervik, M.; Lam, F.; Colombet, M.; Mery, L.; Piñeros, M.; Znaor, A.; Soerjomataram, I.; International Agency for Research on Cancer. Global Cancer Observatory: Cancer Today. 2018. Available online: https://gco.iarc.fr/today (accessed on 4 May 2020).
- Canadian Cancer Statistics. A 2018 Special Report on Cancer Incidence by Stage; Gouvernement du Canada: Toronto, ON, Canada, 2018. Available online: https://www.cancer.ca/~/media/cancer.ca/CW/cancer%20information/cancer%20101/Canadian%20cancer%20statistics/Canadian-Cancer-Statistics-2018-FR.pdf?la=fr-CA (accessed on 12 October 2019).
- Schmidt, S.; The EMPRO Group; Garin, O.; Pardo, Y.; Valderas, J.M.; Alonso, J.; Rebollo, P.; Rajmil, L.; Garcia-Forero, C.; Ferrer, M. Assessing quality of life in patients with prostate cancer: A systematic and standardized comparison of available instruments. Qual. Life Res. 2014, 23, 2169–2181. [Google Scholar] [CrossRef]
- Namiki, S.; Arai, Y. Health-related quality of life in men with localized prostatae cancer. Int. J. Urol. 2010, 17, 125–138. [Google Scholar] [CrossRef] [PubMed]
- Sanyal, C.; Aprikian, A.; Chevalier, S.; Curry, G.; Dragomir, A. Direct cost for initial mangement of prostate cancer: A systematic review. Curr. Oncol. 2013, 20, 522–531. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Fenner, V.; Iselin, C. Management of prostate cancer in the elderly men. Revue Médicale Suisse 2014, 10, 2311–2315. [Google Scholar] [PubMed]
- Cardinal, L.; Langlois, M.; Gagné, D.; Tourigny, A.; Direction de santé publique et Institut national de santé publique du Québec. Perspectives pour un vieillissement en santé: Proposition d’un modèle conceptuel: Agence de la santé et des services sociaux de la Capitale-Nationale. 2008. Available online: https://www.inspq.qc.ca/pdf/publications/860_PerspectiveVieillissementSante.pdf (accessed on 14 July 2017).
- Tarricone, R. Cost-of-illness analysis: What room in health economics? Health Policy 2006, 77, 51–63. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. Canada’s Health Care System. 2016. Available online: https://www.canada.ca/fr/sante-canada/services/systeme-soins-sante-du-canada.html (accessed on 13 August 2019).
- Régie de L’assurance Maladie. Obtain Information on Covered Services. 2019. Available online: https://www.ramq.gouv.qc.ca/fr/citoyens/assurance-maladie/informer-services-couverts (accessed on 17 August 2019).
- Hurley, J. Health Economics, 1st ed.; McGraw-Hill Ryerson: Whitby, ON, Canada, 2010. [Google Scholar]
- De Oliveira, C.; Bremner, K.E.; Ni, A.; Alibhai, S.M.H.; Laporte, A.; Krahn, M.D. Patient time and out-of-pocket costs for long-term prostate cancer survivors in Ontario, Canada. J. Cancer Surviv. 2013, 8, 9–20. [Google Scholar] [CrossRef]
- Gordon, L.G.; Walker, S.; Mervin, M.; Lowe, A.; Smith, D.; Gardiner, R.; Chambers, S. Financial toxicity: A potential side effect of prostate cancer treatment among Australian men. Eur. J. Cancer Care 2015, 26, e12392. [Google Scholar] [CrossRef]
- Jayadevappa, R.; Schwartz, J.S.; Chhatre, S.; Gallo, J.; Wein, A.J.; Malkowicz, S.B. The burden of out-of-pocket and indirect costs of prostate cancer. Prostate 2010, 70, 1255–1264. [Google Scholar] [CrossRef]
- Zheng, Z.; Yabroff, K.R.; Guy, G.P.; Han, X.; Li, C.; Banegas, M.P.; Ekwueme, D.U.; Jemal, A. Annual Medical Expenditure and Productivity Loss Among Colorectal, Female Breast, and Prostate Cancer Survivors in the United States. J. Natl. Cancer Inst. 2015, 108, 382. [Google Scholar] [CrossRef]
- Jung, O.S.; Guzzo, T.; Lee, D.; Mehler, M.; Christodouleas, J.; Deville, C.; Hollis, G.; Shah, A.; Vapiwala, N.; Wein, A.; et al. Out-of-Pocket Expenses and Treatment Choice for Men With Prostate Cancer. Urology 2012, 80, 1252–1257. [Google Scholar] [CrossRef]
- Longo, C.; Bereza, B.G. A comparative analysis of monthly out-of-pocket costs for patients with breast cancer as compared with other common cancers in Ontario, Canada. Curr. Oncol. 2011, 18, e1–e8. [Google Scholar] [CrossRef] [PubMed]
- Longo, C.; Deber, R.; Fitch, M.; Williams, A.; D’Souza, D. An examination of cancer patients’monthly out-of-pocket costs in Ontario, Canada. Eur. J. Cancer Care 2007, 16, 500–507. [Google Scholar] [CrossRef] [PubMed]
- Longo, C.; Fitch, M.I.; Deber, R.; Williams, A.P. Financial and family burden associated with cancer treatment in Ontario, Canada. Support. Care Cancer 2006, 14, 1077–1085. [Google Scholar] [CrossRef] [PubMed]
- Housser, E.; Mathews, M.; LeMessurier, J.; Young, S.; Hawboldt, J.; West, R. Responses by breast and prostate cancer patients to out-of-pocket costs in Newfoundland and Labrador. Curr. Oncol. 2013, 20, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Sethukavalan, P.; Cheung, P.; Tang, C.I.; Quon, H.; Morton, G.; Nam, R.; Loblaw, D.A. Patient costs associated with external beam radiotherapy treatment for localized prostate cancer: The benefits of hypofractionated over conventionally fractionated radiotherapy. Can. J. Urol. 2012, 19, 6165–6169. [Google Scholar] [PubMed]
- Sharp, L.; Timmons, A. The Financial Impact of a Cancer Diagnosis; National Cancer Registry Ireland: Cork, Ireland, 2010.
- Marti, J.; Hall, P.S.; Hamilton, P.; Hulme, C.; Jones, H.; Velikova, G.; Ashley, L.; Wright, P. The economic burden of cancer in the UK: A study of survivors treated with curative intent. Psycho-Oncology 2015, 25, 77–83. [Google Scholar] [CrossRef]
- Smith-Palmer, J.; Takizawa, C.; Valentine, W. Literature review of the burden of prostate cancer in Germany, France, the United Kingdom and Canada. BMC Urol. 2019, 19, 1–16. [Google Scholar] [CrossRef]
- Jayadevappa, R.; Chhatre, S.; Wein, A.J.; Malkowicz, S.B. Predictors of patient reported outcomes and cost of care in younger men with newly diagnosed prostate cancer. Prostate 2009, 69, 1067–1076. [Google Scholar] [CrossRef]
- Institut de la statistique du Québec. Panorama des Régions du Québec. Édition 2018: Gouvernement du Québec; Institut de la statistique du Québec: Abitibi-Témiscamingue, QC, Canada, 2018.
- Centre Intégré de Santé et de Services Sociaux de l’Abitibi-Témiscamingue. Portrait de Santé de la Population. Région Abitibi-Témiscamingue; Centre Intégré de Santé et de Services Sociaux de l’Abitibi-Témiscamingue, Gouvernement du Québec: Abitibi-Témiscamingue, QC, Canada, 2018.
- Institut de la statistique du Québec. Bulletin Statistique Régional; Institut de la statistique du Québec, Gouvernement du Québec: Abitibi-Témiscamingue, QC, Canada, 2019. Available online: http://www.stat.gouv.qc.ca/statistiques/profils/bulletins/2019/08-Abitibi-Temiscamingue.pdf (accessed on 12 June 2019).
- Government of Canada. Reasonable Per-Kilometer Allowance. 2019. Available online: https://www.canada.ca/en/revenue-agency/services/tax/businesses/topics/payroll/benefits-allowances/automobile/automobile-motor-vehicle-allowances/automobile-allowance-rates.html (accessed on 20 April 2019).
- Maruish, M. User’s Manual for the SF-12v2 Health Survey, 3rd ed.; Quality Metric Incorporated: Lincoln, NE, USA, 2012. [Google Scholar]
- Sangha, O.; Stucki, G.; Liang, M.H.; Fossel, A.H.; Katz, J.N. The self-administered comorbidity questionnaire: A new method to assess comorbidity for clinical and health services research. Arthritis Rheum. 2003, 49, 156–163. [Google Scholar] [CrossRef]
- du Plessis, V.; Beshiri, R.; Bollman, R.D. Definitions of rural. Rural and Small Town Canada Analysis Bulletin. 2001, 13, 1–17. [Google Scholar]
- Krahn, M.D.; Zagorski, B.; Laporte, A.; Alibhai, S.M.; Bremner, K.E.; Tomlinson, G.; Warde, P.; Naglie, G. Healthcare costs asssociated with prostate cancer: Estimates from a population-based study. BJU Int. 2010, 105, 338–346. [Google Scholar] [CrossRef] [PubMed]
- Government of Canada. Canada’s Health Care System. 2018. Available online: https://www.canada.ca/en/health-canada/services/health-care-system/reports-publications/health-care-system/canada.html#a1 (accessed on 14 September 2019).
- Taylor, K.L.; Luta, G.; Miller, A.B.; Church, T.R.; Kelly, S.; Muenz, L.R.; Davis, K.M.; Dawson, D.L.; Edmond, S.N.; Reding, D.; et al. Long-Term Disease-Specific Functioning Among Prostate Cancer Survivors and Noncancer Controls in the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial. J. Clin. Oncol. 2012, 30, 2768–2775. [Google Scholar] [CrossRef] [PubMed]
- Riley, G.F.; Potosky, A.L.; Lubitz, J.D.; Kessler, L.G. Medicare Payments from Diagnosis to Death for Elderly Cancer Patients by Stage at Diagnosis. Med. Care 1995, 33, 828–841. [Google Scholar] [CrossRef] [PubMed]
- Azhar, H.; Allam, Z.; Varghese, G.; Engels, D.; John, S. Minimizing the perceived financial burden due to cancer. South. Method. Univ. Data Sci. Rev. 2018, 1, 1–19. [Google Scholar]
- Shih, Y.-C.T.; Chien, C.-R. A review of cost communication in oncology: Patient attitude, provider acceptance, and outcome assessment. Cancer 2017, 123, 928–939. [Google Scholar] [CrossRef]
- Zaidi, A.A.; Ansari, T.Z.; Khan, A. The financial burden of cancer: Estimates from patients undergoing cancer care in a tertiary care hospital. Int. J. Equity Health 2012, 11, 60. [Google Scholar] [CrossRef]
- Rogers, S.N.; Harvey-Woodworth, C.; Hare, J.; Leong, P.; Lowe, D. Patients’ perception of the financial impact of head and neck cancer and the relationship to health related quality of life. Br. J. Oral Maxillofac. Surg. 2012, 50, 410–416. [Google Scholar] [CrossRef]
- Rootman, I.; Gordon-El-Bihbety, D. Vision d’une Culture de la Santé au Canada. Rapport du Groupe D’experts sur la Littératie en Matière de Santé; Association Canadienne de Santé Publique: Ottawa, ON, Canada, 2008; Available online: https://www.cpha.ca/sites/default/files/assets/portals/h-l/report_f.pdf (accessed on 18 August 2019).
- Laxmi, V.; Maheshwary, N. Identification of Factors Influencing Financial Literacy: A Theoretical Review. Int. J. Res. Manag. Econ. Commer. 2018, 8, 89–94. [Google Scholar]
- McDougall, J.A.; Banegas, M.P.; Wiggins, C.L.; Chiu, V.K.; Rajput, A.; Kinney, A.Y. Rural Disparities in Treatment-Related Financial Hardship and Adherence to Surveillance Colonoscopy in Diverse Colorectal Cancer Survivors. Am. Assoc. Cancer Res. J. 2018. Available online: https://cebp.aacrjournals.org/content/cebp/27/11/1275.full.pdf (accessed on 18 March 2018). [CrossRef]
- Shankaran, V.; Ramsey, S. Addressing the financial burden of cancer treatment: From copay to can’t pay. JAMA Oncol. 2015, 1, 273–274. [Google Scholar] [CrossRef]
- Bhandari, A.; Wagner, T. Self-Reported Utilization of Health Care Services: Improving Measurement and Accuracy. Med. Care Res. Rev. 2006, 63, 217–235. [Google Scholar] [CrossRef] [PubMed]
- Lensberg, B.R.; Drummond, M.F.; Danchenko, N.; Despiégel, N.; François, C. Challenges in measuring and valuing productivity costs, and their relevance in mood disorders. Clin. Outcomes Res. CEOR 2013, 5, 565–573. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | n = 171 a |
|---|---|
| Age (years)—Mean ± SD | 68.73 ± 7.28 |
| Min | 47 |
| Max | 87 |
| Race/Ethnicity—n (%) | |
| White | 171 (100) |
| Country of birth—n (%) | |
| Canada | 169 (98.8) |
| Other | 2 (1.2) |
| Professional status—n (%) | |
| Full-time job | 28 (16.3) |
| Part-time job | 14 (8.2) |
| Retired | 125 (73.1) |
| Not working | 2 (1.2) |
| Welfare | 2 (1.2) |
| Relationship status—n (%) | |
| In a relationship | 143 (83.6) |
| Single | 28 (16.4) |
| Annual family income (CAD$)—n (%) | |
| Less than $20,000 | 21 (12.3) |
| Between $20,000 and $39,999 | 67 (39.2) |
| Between $40,000 and $59,999 | 39 (22.8) |
| Between $60,000 and $79,999 | 20 (11.7) |
| Between $80,000 and $99,999 | 13 (7.6) |
| $100,000 and over | 11 (6.4) |
| Completed education—n (%) | |
| Elementary school | 32 (18.7) |
| High school | 66 (38.6) |
| Professional studies | 24 (14) |
| College | 25 (14.6) |
| University | 24 (14.1) |
| Drug insurance—n (%) | |
| Régie de l’assurance maladie du Québec | 123 (71.9) |
| Private insurance | 48 (28.1) |
| Region of residence b—n (%) | |
| Urban | 98 (57.3) |
| Rural | 73 (42.7) |
| PSA (ng/mL)—Mean ± SD | 12.04 ± 36.54 |
| Min | 1 |
| Max | 448 |
| Gleason score—n (%) | |
| ≤6 | 56 (32.8) |
| 7 | 90 (52.6) |
| >7 | 25 (14.6) |
| Tumor stage—n (%) | |
| ≤T2a | 130 (76.5) |
| T2b | 5 (2.9) |
| T2c | 35 (20.6) |
| Missed | 1 (0.6) |
| Comorbidity—Mean ± SD | 2.57 ± 1.50 |
| Min | 1 |
| Max | 9 |
| Time elapsed since first treatment—n (%) | |
| 0–1 year | 44 (25.7) |
| 2–3 years | 53 (31.0) |
| 4–5 years | 29 (17.0) |
| 6, 7, 8 and 9 years | 27 (15.8) |
| 10 years and over | 18 (10.5) |
| First treatment received after diagnosis—n (%) | |
| Radical prostatectomy | 44 (26.2) |
| Radiotherapy | 96 (57.1) |
| Active surveillance | 23 (13.7) |
| Hormonotherapy | 4 (2.3) |
| Others | 1 (0.7) |
| More than one treatment—n (%) | |
| Yes | 58 (34.5) |
| No | 110 (65.5) |
| Subtotal Costs for Hospital, Drugs, Vitamins, Supplements, Alternative and Complementary Therapies, etc. | Subtotal Travel Costs | Subtotal Parking Costs | Subtotal Accommodation Costs | Total Costs | |
|---|---|---|---|---|---|
| Overall | |||||
| 3-months out-of-pocket costs for all participants ($) (n = 171) | |||||
| Mean ± SD | 136.82 ± 328.80 | 344.19 ± 808.53 | 5.90 ± 18.00 | 29.29 ± 185.95 | 516.19 ± 1029.71 |
| Median (range) | 15 (0–2300) | 88 (0–5500) | 0 (0–132) | 0 (0–2200) | 139 (0–6148) |
| 3-months out-of-pocket costs for participants with non-null costs ($) (n = 142) | |||||
| Mean ± SD | 164.76 ± 354.54 | 414.48 ± 871.11 | 7.1 ± 19.54 | 35.27 ± 203.66 | 621.61 ± 1101.09 |
| Median (range) | 39.5 (0–2300) | 115.5 (0–5500) | 1.13 (0–132) | 0 (0–2200) | 226.66 (5.3–6148) |
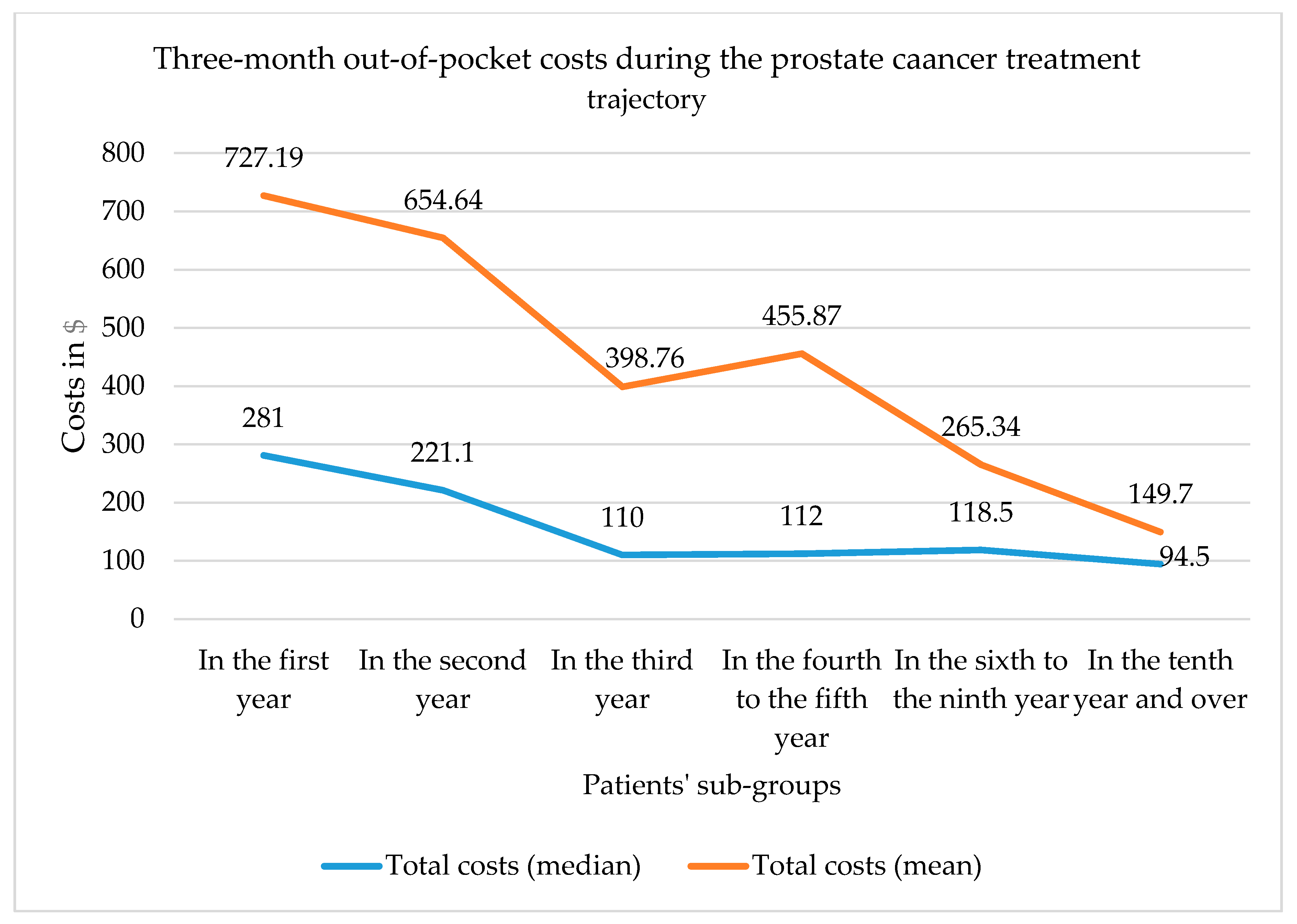
| By time since first treatment | |||||
| 3-months out-of-pocket costs for patients who are in the first year or less since first treatment ($) (n = 44) | |||||
| Mean ± SD | 182.15 ± 376.69 | 472.33 ± 968.68 | 4.75 | 67.95 ± 337.36 | 727.19 ± 1237.80 |
| Median (range) | 31 (0–1900) | 137.5 (0–5500) | 0 (0–90) | 0 (0–2200) | 281 (0–5790) |
| 3-months out-of-pocket costs for patients who are in the second year since first treatment ($) (n = 22) | |||||
| Mean ± SD | 106.40 ± 318.53 | 500.05 ± 946.71 | 11.81 ± 31.23 | 36.36 ± 121.67 | 654.64 ± 1090.12 |
| Median (range) | 12.5 (0–1500) | 117.70 (0–4070) | 1 (0–132) | 0 (0–500) | 221.10 (0–4110) |
| 3-months out-of-pocket costs for patients who are in the third year or more since first treatment ($) (n = 105) | |||||
| Mean ± SD | 124.19 ± 310.36 | 257.82 ± 692.83 | 5.13 ± 15.56 | 11.6 ± 74.25 | 398.76 ± 907.15 |
| Median (range) | 12 (0–2300) | 33 (0–4510) | 0 (0–125) | 0 (0–700) | 110 (0–6148) |
| Factors | None or Slight Burden (n = 133) | Manageable, Difficult to Manage or Unmanageable Significant Burden (n = 38) | Univariate Logistic Regression p-Value | Crude OR (95%CI) | Adjusted OR (95%CI) f |
|---|---|---|---|---|---|
| Age—Mean ± SD | 69.13 ± 7.03 | 67.32 ± 8.02 | 0.18 | 0.97 (0.92–1.02) | |
| Annual family income—n (%) a Less than $39,999 (reference) Between $40,000 and $79,999 $80,000 and over | 63 (47.4) 51 (38.3) 19 (14.3) | 25 (65.8) 8 (21.1) 5 (13.2) | 0.04 e 0.46 | 0.40 (0.16–0.95) 0.66 (0.22–1.97) | 0.15 (0.03–0.69) 0.09 (0.07–1.30) |
| Completed education—n (%) a Elementary and high school (reference) Professional studies and college University | 72 (54.1) 38 (28.6) 23 (17.3) | 26 (68.4) 11 (28.9) 1 (2.6) | 0.59 0.04 e | 0.8 (0.36–1.80) 0.12 (0.02–0.94) | 0.75 (0.22–2.53) 0.03 (0.00–0.79) |
| Employment status—n (%) b Retired or not working (reference) Full-time or part-time job | 102 (76.7) 31 (23.3) | 27 (71.1) 11 (28.9) | 0.48 | 1.34 (0.60–3.01) | |
| Relationship—n (%) In a relationship (reference) Single | 112 (84.2) 21 (15.8) | 31 (81.6) 7 (18.4) | 0.70 | 1.20 (0.47–3.09) | |
| Region of residence—n (%) Urban (reference) Rural | 77 (57.9) 56 (42.1) | 21 (55.3) 17 (44.7) | 0.77 | 1.11 (0.54–2.30) | |
| Drug insurance—n (%) Régie de l’assurance maladie du Québec (reference) Private insurance (employer- provided insurance or personally purchased insurance) | 101 (75.9) 32 (24.1) | 22 (57.9) 16 (42.1) | 0.03 e | 2.30 (1.08–4.89) | 5.23 (1.13–24.17) |
| Additional insurance—n (%) No (reference) Yes | 95 (71.4) 38 (28.6) | 27 (71.1) 11 (28.9) | 0.96 | 1.02 (0.46–2.26) | |
| APS at diagnosis—Mean ± SD | 13.05 ± 41.28 | 8.51 ± 6.08 | 0.56 | 0.99 (0.96–1.02) | |
| Gleason score at diagnosis—Mean ± SD c | 6.77 ± 0.70 | 7.11 ± 0.76 | 0.01 e | 1.88 (1.14–3.10) | 1.13 (0.53–2.40) |
| Clinical tumor stage at diagnosis—n (%) d ≤ T2a (reference) T2b-T2c | 100 (75.2) 33 (24.8) | 30 (81.1) 7 (18.9) | 0.46 | 0.71 (0.28–1.76) | |
| Time elapsed since treatment—Mean ± SD | 4.44 ± 3.99 | 2.92 ± 2.28 | 0.03 e | 0.87 (0.77–0.99) | 0.97 (0.82–1.15) |
| Number of treatments received—Mean ± SD | 1.35 ± 0.58 | 1.66 ± 0.75 | 0.01 e | 2.01 (1.18–3.43) | 2.02 (0.80–5.11) |
| Out-of-pocket costs—Mean ± SD | 249.20 ± 410 | 1450.65 ± 1765.81 | 0.00 e | 1 (1–1) | 1.001 (1.001–1.002) |
| Physical health-related quality of life—Mean ± SD | 48.42 ± 9.31 | 42.14 ± 11.55 | 0.00 e | 0.95 (0.91–0.98) | 0.95 (0.913–0.997) |
| Mental health-related quality of life—Mean ± SD | 47.91 ± 8.51 | 41.90 ± 10.30 | 0.00 e | 0.93 (0.90–0.97) | 0.947 (0.895– 1.002) |
| Treatment in the region vs. outside the region—n (%) In the region Outside the region (reference) | 47 (36.2) 83 (63.8) | 6 (16.2) 31 (83.8) | 0.03 e | 2.93 (1.14–7.52) | 0.87 (0.22–3.41) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Haouly, A.; Lacasse, A.; El-Rami, H.; Liandier, F.; Dragomir, A. Out-of-Pocket Costs and Perceived Financial Burden Associated with Prostate Cancer Treatment in a Quebec Remote Area: A Cross-Sectional Study. Curr. Oncol. 2021, 28, 26-39. https://doi.org/10.3390/curroncol28010005
El-Haouly A, Lacasse A, El-Rami H, Liandier F, Dragomir A. Out-of-Pocket Costs and Perceived Financial Burden Associated with Prostate Cancer Treatment in a Quebec Remote Area: A Cross-Sectional Study. Current Oncology. 2021; 28(1):26-39. https://doi.org/10.3390/curroncol28010005
Chicago/Turabian StyleEl-Haouly, Abir, Anais Lacasse, Hares El-Rami, Frederic Liandier, and Alice Dragomir. 2021. "Out-of-Pocket Costs and Perceived Financial Burden Associated with Prostate Cancer Treatment in a Quebec Remote Area: A Cross-Sectional Study" Current Oncology 28, no. 1: 26-39. https://doi.org/10.3390/curroncol28010005
APA StyleEl-Haouly, A., Lacasse, A., El-Rami, H., Liandier, F., & Dragomir, A. (2021). Out-of-Pocket Costs and Perceived Financial Burden Associated with Prostate Cancer Treatment in a Quebec Remote Area: A Cross-Sectional Study. Current Oncology, 28(1), 26-39. https://doi.org/10.3390/curroncol28010005






