The Bone Lid Technique in Oral and Maxillofacial Surgery: A Scoping Review
Abstract
:1. Introduction
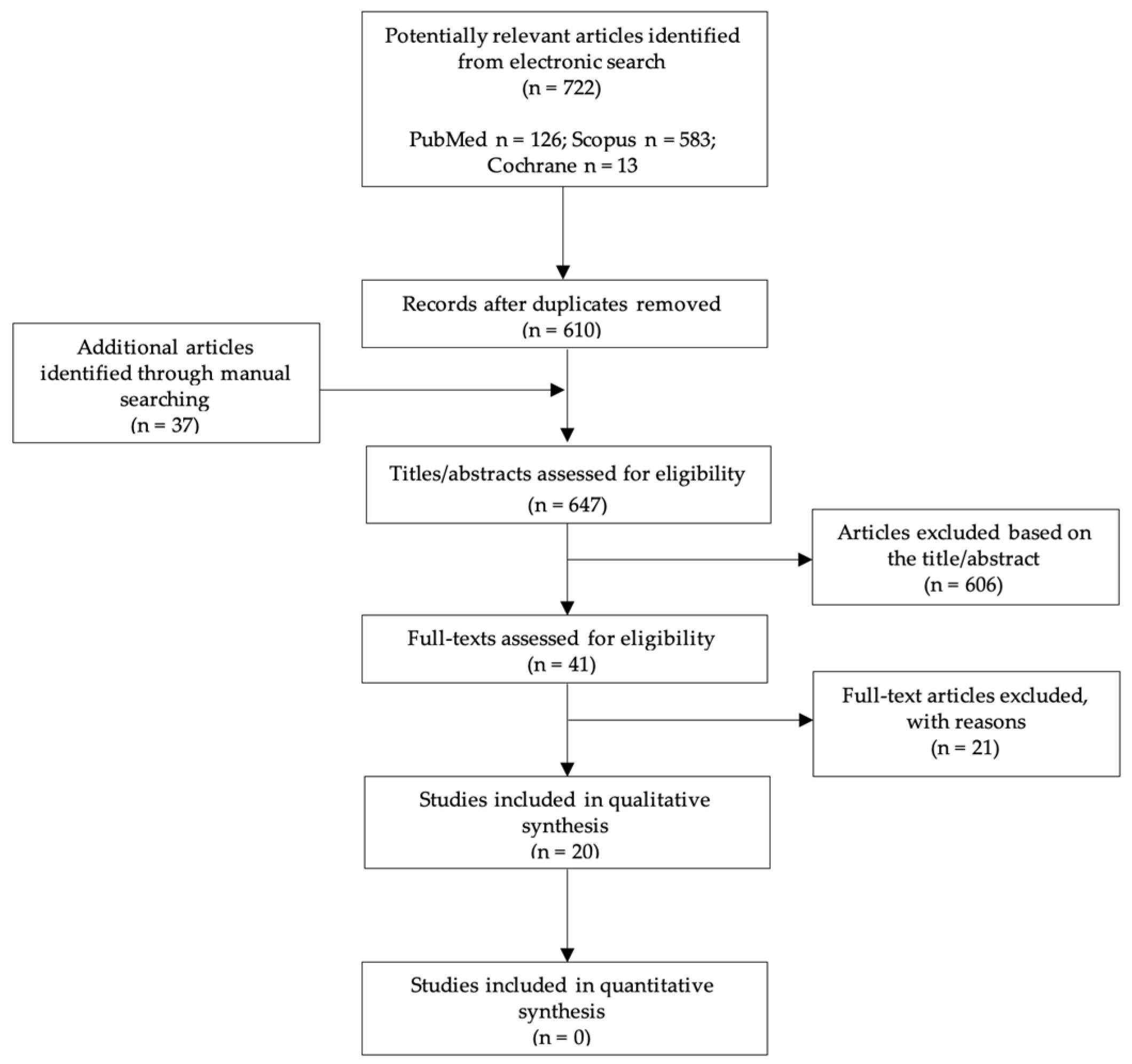
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Selection of the Studies
2.4. Data Charting
2.5. Synthesis of Results
3. Results
4. Discussion
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Khoury, F.; Hensher, R. The bony lid approach for the apical root resection of lower molars. Int. J. Oral Maxillofac. Surg. 1987, 16, 166–170. [Google Scholar] [CrossRef]
- Pappalardo, S.; Guarnieri, R. Randomized clinical study comparing piezosurgery and conventional rotatory surgery in mandibular cyst enucleation. J. Craniomaxillofac. Surg. 2014, 42, e80–e85. [Google Scholar] [CrossRef] [PubMed]
- Oh, S.; Park, J.-H.; Paeng, J.-Y.; Kim, C.-S.; Hong, J. Comparison of surgical approach and outcome for the treatment of cystic lesion on lower jaw. J. Korean Assoc. Oral Maxillofac. Surg. 2012, 38, 276–283. [Google Scholar] [CrossRef] [Green Version]
- Sivolella, S.; Brunello, G.; Fistarol, F.; Stellini, E.; Bacci, C. The bone lid technique in oral surgery: A case series study. Int. J. Oral Maxillofac. Surg. 2017, 46, 1490–1496. [Google Scholar] [CrossRef]
- Savitha, K.; Cariappa, K.M. An effective extraoral approach to the mandible. A technical note. Int. J. Oral Maxillofac. Surg. 1998, 27, 61–62. [Google Scholar] [CrossRef]
- Rattan, V.; Sethi, A. Arteriovenous malformation of the mandible: Successful management by buccal window approach. Br. J. Oral Maxillofac. Surg. 2010, 48, e31–e33. [Google Scholar] [CrossRef]
- Degerliyurt, K.; Akar, V.; Denizci, S.; Yucel, E. Bone lid technique with piezosurgery to preserve inferior alveolar nerve. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2009, 108, e1–e5. [Google Scholar] [CrossRef]
- Sivolella, S.; Brunello, G.; Berengo, M.; De Biagi, M.; Bacci, C. Rehabilitation with Implants after Bone Lid Surgery in the Posterior Mandible. J. Oral Maxillofac. Surg. 2015, 73, 1485–1492. [Google Scholar] [CrossRef]
- Khoury, F. The bony lid approach in pre-implant and implant surgery: A prospective study. Eur. J. Oral Implantol. 2013, 6, 375–384. [Google Scholar]
- Jung, S.R.; Bashutski, J.D.; Linebaugh, M.L. Application of modified bony lid technique to remove or replace compromised implants: Case series. Implant Dent. 2013, 22, 206–211. [Google Scholar] [CrossRef]
- Kwon, Y.D.; Pae, A. Piezoelectric Trapezoidal Osteotomy for the Retrieval of a Displaced Dental Implant in the Osteoporotic Mandibular Body. Implant Dent. 2016, 25, 703–706. [Google Scholar] [CrossRef] [PubMed]
- Atef, M.; Mounir, M. Computer-Guided Inferior Alveolar Nerve Lateralization with Simultaneous Implant Placement: A Preliminary Report. J. Oral Implantol. 2018, 44, 192–197. [Google Scholar] [CrossRef] [PubMed]
- Bacci, C.; Sivolella, S.; Brunello, G.; Stellini, E. Maxillary sinus bone lid with pedicled bone flap for foreign body removal: The piezoelectric device. Br. J. Oral Maxillofac. Surg. 2014, 52, 987–989. [Google Scholar] [CrossRef] [PubMed]
- Biglioli, F.; Chiapasco, M. An easy access to retrieve dental implants displaced into the maxillary sinus: The bony window technique. Clin. Oral Implants Res. 2014, 25, 1344–1351. [Google Scholar] [CrossRef]
- Sohn, D.S.; Heo, J.U.; Kwak, D.H.; Kim, D.E.; Kim, J.M.; Moon, J.W.; Lee, J.H.; Park, I.S. Bone regeneration in the maxillary sinus using an autologous fibrin-rich block with concentrated growth factors alone. Implant Dent. 2011, 20, 389–395. [Google Scholar] [CrossRef] [Green Version]
- Chiapasco, M.; Felisati, G.; Maccari, A.; Borloni, R.; Gatti, F.; Di Leo, F. The management of complications following displacement of oral implants in the paranasal sinuses: A multicenter clinical report and proposed treatment protocols. Int. J. Oral Maxillofac. Surg. 2009, 38, 1273–1278. [Google Scholar] [CrossRef]
- Naros, A.; Peters, J.P.; Biegner, T.; Weise, H.; Krimmel, M.; Reinert, S. Fungus Ball of the Maxillary Sinus-Modern Treatment by Osteoplastic Approach and Functional Endoscopic Sinus Surgery. J. Oral Maxillofac. Surg. 2019, 77, 546–554. [Google Scholar] [CrossRef]
- Göçmen, G.; Varol, A.; Selçuk, B.; Göker, K. Extraoral Extraction of an Impacted Molar Using Bone Lid Technique. Marmara Dent. J. 2013, 1, 42–43. [Google Scholar] [CrossRef] [Green Version]
- Lazaridis, N.; Tilaveridis, I.; Venetis, G.; Lazaridou, M. Maxillary sinus osteoplasty with vascularized pedicled bone flap. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 828–832. [Google Scholar] [CrossRef]
- Balleri, P.; Veltri, M.; Nuti, N.; Ferrari, M. Implant placement in combination with sinus membrane elevation without biomaterials: A 1-year study on 15 patients. Clin. Implant Dent. Relat. Res. 2012, 14, 682–689. [Google Scholar] [CrossRef]
- Bayram, B.; Alaaddinoglu, E. Implant-box mandible: Dislocation of an implant into the mandible. J. Oral Maxillofac. Surg. 2011, 69, 498–501. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.M.; Sohn, D.S.; Heo, J.U.; Moon, J.W.; Lee, J.H.; Park, I.S. Benefit of the replaceable bony window in lateral maxillary sinus augmentation: Clinical and histologic study. Implant Dent. 2014, 23, 277–282. [Google Scholar] [CrossRef] [PubMed]
- Chiapasco, M.; Flora, A.; Serioli, L.; Zaniboni, M. The removal of a deeply impacted lower third molar by means of the bone lid technique with piezoelectric instruments. Ital. J. Dent. Med. 2017, 2, 13–17. [Google Scholar]
- Sukegawa, S.; Kanno, T.; Matsumoto, K.; Sukegawa-Takahashi, Y.; Masui, M.; Furuki, Y. Complications of a poly-L-lactic acid and polyglycolic acid osteosynthesis device for internal fixation in maxillofacial surgery. Odontology 2018, 106, 360–368. [Google Scholar] [CrossRef]
- Katauczek, F.; Nkenke, E.; Wagner, F.; Seemann, R. A modified bone lid for osteoplastic surgery of the maxillary sinus. Int. J. Oral Maxillofac. Surg. 2015, 44, 889–891. [Google Scholar] [CrossRef]
- Hu, Y.K.; Yang, C.; Xu, G.Z.; Xie, Q.Y. Digital design of functional surgery for odontogenic cyst intruding into maxillary sinus. Braz. J. Otorhinolaryngol. 2018, 84, 212–219. [Google Scholar] [CrossRef]
- Sivolella, S.; Brunello, G.; Fincato, A.; De Stavola, L. Computer-guided bone lid osteotomy with piezosurgery. Ann. Stomatol. 2018, 9, 84–90. [Google Scholar]
- Sukegawa, S.; Kanno, T.; Shibata, A.; Matsumoto, K.; Sukegawa-Takahashi, Y.; Sakaida, K.; Furuki, Y. Intraoperative navigation-assisted accurate bone lid surgery to remove a mandibular lesion: A case report. Oral Maxillofac. Surg. Cases 2017, 3, 15–19. [Google Scholar] [CrossRef]
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef] [Green Version]
- Shuster, J.J. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. In The Cochrane Collaboration; Higgins, J.P.T., Green, S., Eds.; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2011. [Google Scholar]
- Sterne, J.A.; Hernán, M.A.; Reeves, B.C.; Savović, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [Green Version]
- Aliyev, T.; Efeoglu, B.F.; Rizaj, X.; Sahin, O. Removal of the residual root and implant therapy simultaneously via bone lid approach. Niger. J. Clin. Pract. 2019, 22, 739–741. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, A.; Badiali, G.; Piersanti, L.; Marchetti, C. Computer-assisted piezoelectric surgery: A navigated approach toward performance of craniomaxillofacial osteotomies. J. Craniofac. Surg. 2015, 26, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Bovi, M.; Manni, A.; Mavriqi, L.; Bianco, G.; Celletti, R. The use of piezosurgery to mobilize the mandibular alveolar nerve followed immediately by implant insertion: A case series evaluating neurosensory disturbance. Int. J. Periodontics Restor. Dent. 2010, 30, 73–81. [Google Scholar]
- Choi, H.; Cho, G.J.; Jung, K.H.; Jeon, J.Y.; Lim, S.W.; Park, C.J.; Hwang, K.G. The dual-port endoscope-assisted cyst enucleation on the maxillofacial region. Maxillofac. Plast. Reconstr. Surg. 2021, 43, 40. [Google Scholar] [CrossRef]
- Hamdoon, Z.; Mahmood, N.; Talaat, W.; Sattar, A.A.; Naeim, K.; Qais, A.; Kheder, W.; Jerjes, W. Evaluation of different surgical approaches to remove dental implants from the maxillary sinus. Sci. Rep. 2021, 11, 4440. [Google Scholar] [CrossRef]
- Lee, S.M.; Yu, Y.H.; Wang, Y.; Kim, E.; Kim, S. The Application of “Bone Window” Technique in Endodontic Microsurgery. J. Endod. 2020, 46, 872–880. [Google Scholar] [CrossRef]
- Liu, Z.; Huang, D.; Li, K.; Li, H.; Liu, L. Precise locating and cutting of the bone lid with a digital template during the treatment of large mandibular cysts: A case series study. J. Craniomaxillofac. Surg. 2021, 49, 358–361. [Google Scholar] [CrossRef] [PubMed]
- Nordera, P.; Spanio di Spilimbergo, S.; Stenico, A.; Fornezza, U.; Volpin, L.; Padula, E. The cutting-edge technique for safe osteotomies in craniofacial surgery: The piezosurgery bone scalpel. Plast. Reconstr. Surg. 2007, 120, 1989–1995. [Google Scholar] [CrossRef] [PubMed]
- Saibene, A.M.; Collurà, F.; Pipolo, C.; Bulfamante, A.M.; Lozza, P.; Maccari, A.; Arnone, F.; Ghelma, F.; Allevi, F.; Biglioli, F.; et al. Odontogenic rhinosinusitis and sinonasal complications of dental disease or treatment: Prospective validation of a classification and treatment protocol. Eur. Arch. Otorhinolaryngol. 2019, 276, 401–406. [Google Scholar] [CrossRef] [Green Version]
- Scolozzi, P.; Martinez, A.; Lombardi, T.; Jaques, B. Lateral antrotomy as a surgical approach for maxillary sinus: A modified technique with free bone flap repositioning and fixation with a titanium plate. J. Oral Maxillofac. Surg. 2009, 67, 689–692. [Google Scholar] [CrossRef]
- Seo, M.-H.; Lee, J.-Y.; Frimpong, P.; Eo, M.-Y.; Kim, S.-M. Modified Endoscopic-Assisted Approach for Removal of Ectopic Third Molar in the Maxillary Sinus. Appl. Sci. 2021, 11, 8446. [Google Scholar] [CrossRef]
- Wang, Y.J.; He, Y.Y.; Zhao, S.F.; Bacci, C.; Sivolella, S.; Brunello, G.; Stellini, E. Maxillary sinus bone lid with pedicled bone flap for foreign body removal: The piezoelectric device. Br. J. Oral Maxillofac. Surg. 2015, 53, 404–405. [Google Scholar] [CrossRef] [PubMed]
- Yura, S.; Kato, T.; Ooi, K.; Izumiyama, Y. Access to the maxillary sinus using a bone flap with sinus mucosal and mucoperiosteal pedicles. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e8–e12. [Google Scholar] [CrossRef]
- Sohn, D.S.; Jung, H.S.; Kim, K.H.; Song, K.J.; An, H.W.; Min, K.H. Removal of displaced foreign body from the maxillary sinus using replaceable bony windows and saline irrigation, followed by suctioning of the foreign body. Implant Dent. 2011, 20, 112–117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sukegawa, S.; Yamamoto, N.; Matsuyama, T.; Takabatake, K.; Kawai, H.; Nagatsuka, H.; Furuki, Y. Factors of successful treatment using the bone lid technique in maxillofacial surgery: A pilot study. J. Hard Tissue Biol. 2021, 30, 193–198. [Google Scholar] [CrossRef]
- Ahmed, M.; Salah, M.K.; Khairy, N. Computer-Aided Design/Computer-Aided Manufacturing Cutting Guides for Odontectomy of Deeply Impacted Mandibular Third Molars. Open Access Maced. J. Med. Sci. 2018, 6, 2395–2401. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kablan, F.; Yaffe, V.; El-Naaj, I.A. The Buccal Lid Approach for Removal of Impacted Mandibular Molars—When, How and Why? Open J. Stomatol. 2017, 7, 81. [Google Scholar] [CrossRef] [Green Version]
- Hu, Y.K.; Yang, C.; Zhou Xu, G.; Wang, Y.; Abdelrehem, A. Retrieval of root fragment in maxillary sinus via anterolateral wall of the sinus to preserve alveolar bone. J. Craniofac. Surg. 2015, 26, e81–e84. [Google Scholar] [CrossRef]
- Xu, G.Z.; Yang, C.; Fan, X.D.; Hu, Y.K.; Yu, C.Q. Functional surgery for the treatment of dentigerous cyst in the maxillary sinus. J. Craniofac. Surg. 2015, 26, e84–e86. [Google Scholar] [CrossRef]
- Kurokawa, H.; Takeda, S.; Yamashita, Y.; Nakamura, T.; Takahashi, T. Evaluation of a modified method for maxillary sinus surgery—Reimplantation of the anterior bony wall of the maxillary sinus. Asian J. Oral Maxillofac. Surg. 2002, 14, 144–147. [Google Scholar] [CrossRef]
- Choung, P.H.; Choung, Y.H. Vascularized bone flap for access to the maxillary sinus. J. Oral Maxillofac. Surg. 1997, 55, 832–835. [Google Scholar] [CrossRef]
- Choi, B.H.; Yoo, J.H.; Sung, K.J. Radiographic comparison of osseous healing after maxillary sinusotomy performed with and without a periosteal pedicle. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 1996, 82, 375–378. [Google Scholar] [CrossRef]
- Widmark, G.; Ekholm, S.; Borrman, H.; Grangård, U.; Holmberg, K. The use of a bone lid to close the anterior wall defect after surgery in the maxillary sinus. Swed. Dent. J. 1992, 16, 173–182. [Google Scholar] [PubMed]
- Lasaridis, N.; Zouloumis, L.; Antoniadis, K. Bony lid approach for apicoectomy of mandibular molars. Aust. Dent. J. 1991, 36, 366–368. [Google Scholar] [CrossRef]
- Lindorf, H.H. Osteoplastic surgery of the sinus maxillaris--the “bone lid”-method. J. Maxillofac. Surg. 1984, 12, 271–276. [Google Scholar] [CrossRef]
- Lindorf, H. Knochendeckelverschluss nach oraler Kieferhoehleneroffnung. Dtsch. Zhanaertl. Z. 1974, 29, 587–590. [Google Scholar]
- Lindorf, H. Tierexperimentelle Untersuchungen zur osteo plastischen Kieferhöhlenoperation (Knochendeckelmethode). Dtsch. Z. Mund Kiefer Gesichtschir. 1983, 7, 378–383. [Google Scholar]
- Lieblich, S.E. Endodontic surgery. Dent. Clin. N. Am. 2012, 56, 121–132. [Google Scholar] [CrossRef]
- Setzer, F.C.; Shah, S.B.; Kohli, M.R.; Karabucak, B.; Kim, S. Outcome of endodontic surgery: A meta-analysis of the literature--part 1: Comparison of traditional root-end surgery and endodontic microsurgery. J. Endod. 2010, 36, 1757–1765. [Google Scholar] [CrossRef]
- Hu, Y.K.; Xie, Q.Y.; Yang, C.; Xu, G.Z. Computer-designed surgical guide template compared with free-hand operation for mesiodens extraction in premaxilla using “trapdoor” method. Medicine 2017, 96, e7310. [Google Scholar] [CrossRef]
- Stajčić, Z.; Stojčev Stajčić, L.J.; Kalanović, M.; Đinić, A.; Divekar, N.; Rodić, M. Removal of dental implants: Review of five different techniques. Int. J. Oral Maxillofac. Surg. 2016, 45, 641–648. [Google Scholar] [CrossRef] [PubMed]
- Khoury, F.; Antoun, H.; Missika, P. Bone Augmentation in Oral Implantology; Quintessence Publishing: Hanover Park, IL, USA, 2007. [Google Scholar]
- Lee, S.C.; Jeong, C.H.; Im, H.Y.; Kim, S.Y.; Ryu, J.Y.; Yeom, H.Y.; Kim, H.M. Displacement of dental implants into the focal osteoporotic bone marrow defect: A report of three cases. J. Korean Assoc. Oral Maxillofac. Surg. 2013, 39, 94–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nogami, S.; Yamauchi, K.; Tanuma, Y.; Odashima, K.; Matsui, A.; Tanaka, K.; Takahashi, T. Removal of dental implant displaced into maxillary sinus by combination of endoscopically assisted and bone repositioning techniques: A case report. J. Med. Case Rep. 2016, 10, 1. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Biglioli, F.; Goisis, M. Access to the maxillary sinus using a bone flap on a mucosal pedicle: Preliminary report. J. Craniomaxillofac. Surg. 2002, 30, 255–259. [Google Scholar] [CrossRef] [PubMed]
- Tilaveridis, I.; Lazaridou, M.; Dimitrakopoulos, I.; Lazaridis, N.; Charis, C. Displacement of three dental implants into the maxillary sinus in two patients. Report of two cases. Oral Maxillofac. Surg. 2012, 16, 311–314. [Google Scholar] [CrossRef] [PubMed]
- Tsodoulos, S.; Karabouta, I.; Voulgaropoulou, M.; Georgiou, C. Atraumatic removal of an asymptomatic migrated dental implant into the maxillary sinus: A case report. J. Oral Implantol. 2012, 38, 189–193. [Google Scholar] [CrossRef]
- Vercellotti, T.; De Paoli, S.; Nevins, M. The piezoelectric bony window osteotomy and sinus membrane elevation: Introduction of a new technique for simplification of the sinus augmentation procedure. Int. J. Periodontics Restor. Dent. 2001, 21, 561–567. [Google Scholar]
| Database | Search Strategy |
|---|---|
| PubMed | ((“bone lid” [All Fields] OR “bony lid” [All Fields]) OR “bony window” [All Fields]) AND ((((((((((((((((((((((((((((“methods” [MeSH Subheading] OR “methods” [All Fields]) OR “techniques” [All Fields]) OR “methods”[MeSH Terms]) OR “technique” [All Fields]) OR “technique s” [All Fields]) OR (“piezosurgery” [MeSH Terms] OR “piezosurgery” [All Fields])) OR “microsaw” [All Fields]) OR “micro-saw” [All Fields]) OR “bone defect*” [All Fields]) OR “oral surgery” [All Fields]) OR ((((“maxilla”[MeSH Terms] OR “maxilla” [All Fields]) OR “maxillae” [All Fields]) OR “maxillas”[All Fields]))) OR (((“mandible” [MeSH Terms] OR “mandible” [All Fields]) OR “mandibles”[All Fields]) OR “mandible s” [All Fields])) OR “maxillary sinus” [All Fields]) OR (((“apicoectomy”[MeSH Terms] OR “apicoectomy” [All Fields]) OR “apicectomies” [All Fields]) OR “apicectomy” [All Fields])) OR “apical surgery” [All Fields]) OR “endodontic surgery” [All Fields]) OR “root-end surgery” [All Fields]) OR “implant*” [All Fields]) OR “impacted teeth” [All Fields]) OR “impacted tooth” [All Fields]) OR “impacted molar*” [All Fields]) OR “third molar*” [All Fields]) OR “inferior alveolar nerve*” [All Fields]) OR “cyst*” [All Fields]) OR “cystic lesion*” [All Fields]) OR “computer-guided” [All Fields]) OR “osteoplastic procedure*” [All Fields]) OR “sinus surgeries” [All Fields]) Filter: English |
| Scopus | (“bone lid” OR “bony lid” OR “bony window”) AND (technique OR piezosurgery OR microsaw OR micro-saw OR “bone defect” OR “bone defects” OR “oral surgery” OR maxilla OR mandible OR “maxillary sinus” OR apicectomy OR “apical surgery” OR “endodontic surgery” OR “root-end surgery” OR implant OR implants OR “impacted teeth” OR “impacted tooth” OR “impacted molar” OR “impacted molars” OR “third molar” OR “third molars” OR “inferior alveolar nerve” OR “inferior alveolar nerves” OR cyst OR cysts OR “cystic lesion” OR “cystic lesions” OR “computer-guided” OR “osteoplastic procedure” OR “osteoplastic procedures” OR “sinus surgeries”) AND (LIMIT-TO (LANGUAGE, “English”)) |
| Cochrane Central Register of Controlled Trials (CENTRAL) | (“bone lid” OR “bony lid” OR “bony window”) AND (technique OR piezosurgery OR microsaw OR micro-saw OR “bone defect” OR “bone defects” OR “oral surgery” OR maxilla OR mandible OR “maxillary sinus” OR apicectomy OR “apical surgery” OR “endodontic surgery” OR “root-end surgery” OR implant OR implants OR “impacted teeth” OR “impacted tooth” OR “impacted molar” OR “impacted molars” OR “third molar” OR “third molars” OR “inferior alveolar nerve” OR “inferior alveolar nerves” OR cyst OR cysts OR “cystic lesion” OR “cystic lesions” OR “computer-guided” OR “osteoplastic procedure” OR “osteoplastic procedures” OR “sinus surgeries”) in Title Abstract Keyword—in Trials |
| Main Reasons for Exclusion | No. | References |
|---|---|---|
| Bone lids not repositioned | 6 | Choi et al., 2021 [35]; Hamdoon et al., 2021 [36]; Saibene et al. 2019 [40]; Bianchi et al., 2015 [33]; Bovi et al., 2010 [34]; Nordera et al., 2007 [39] |
| Technical note | 3 | Katauczek et al., 2015 [25]; Bacci et al., 2014 [13]; Yura et al., 2010 [44] |
| Case report or case series with n < 10 bone lids | 12 | Liu et al., 2021 [38]; Seo et al., 2021 [42]; Lee et al., 2020 [37]; Aliyev et al., 2019 [32]; Sukegawa et al., 2018 [24]; Chiapasco et al., 2017 [23]; Sivolella et al., 2015 [8]; Wang et al., 2015 [43]; Sohn et al., 2011 [45]; Degerliyurt et al., 2009 [7]; Scolozzi et al., 2009 [41]; Chiapasco et al., 2009 [16] |
| Ref. | Study Design | Clinical Indication | Total No. of Pts. | Total No. of Bone Lid Pts. | Gender (M/F) * | Mean Age (Range), yr * | Jaw (Max /Mand) | No. of Cases (Bone Lid) | Mean Follow-Up (Range) | Bone-Cutting Instruments | Bone Lid Fixation |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sukegawa et al., 2021 [46] | Retrospective cohort study | Radicular cyst; follicular cyst; benign tumor | 30 | 30 | 19/11 | 36.7 (SD 19.6; range 12–77) | Max (11)/mand (16) § | 30 | Max: > 1 yr; mand > 6 mths | Piezosurgery | Resorbable plates (PLLA, PLLA/PGA, u-HA/PLLA) |
| Naros et al., 2019 [17] | Case series | Treatment of maxillary sinus fungus ball | 22 | 21 | 12/10 | 58.3 (SD 14.7) | Max | 21 | 12.9 mths | Thin cutting wheel; piezosurgery | Suture |
| Ahmed et al., 2018 [47] | Prospective cohort study | Impacted mandibular third molar removal | 18 | 18 | 7/11 | 24.5 (20–29) | Mand | 18 | 6 mths | Disc microsaw (inferior cut) + reciprocating saw | None |
| Hu et al., 2018 [26] | Case-control study | Odontogenic maxillary sinus cyst removal | 45 | 22 | 27/18 | 43.26 (17–68) | Max | 22 | 3 mths | Piezosurgery | Miniplates |
| Kablan et al., 2017 [48] | Case series | Impacted mandibular third molar removal | 9 | 7 | 5/4 (bone lid 3/4) | Total 30.7 (12–75); bone lid 20.3 (12–27) | Mand | 10 (+2 not repositioned) | >1 yr | Small round bur (superior osteotomy) + disc microsaw | None (2); microplates (8) |
| Sivolella et al., 2017 [4] | Case series | Cyst/keratocystic odontogenic tumor enucleation; impacted teeth extraction (with or without associated cysts); apicectomy | 21 | 21 | 15/6 | 40.5 (18–72) | Mand | 21 | 2.3 yrs (1–6 yrs) | Piezosurgery | Miniplates |
| Hu et al., 2015 [49] | Case series | Displaced root fragment removal from sinus | 21 | 10 | 9/12 | 43.4 (22–60) | Max | 10 | (3 mths–2.5 yrs) | Piezosurgery | Microplates |
| Xu et al., 2015 [50] | Case series | Dentigerous cyst removal | 20 | 20 | 11/9 | 35 (17–68) | Max | 20 | 14 mths (6–24 mths) | Piezosurgery | Microplate |
| Biglioli and Chiapasco, 2014 [14] | Case series | Displaced implant removal from sinus | 36 | 36 | 19/17 | 50.8 (28–72) | Max | 36 | (4–6 mths) | Piezosurgery or reciprocating saw; diamond bur (for upper horizontal osteotomy) | Resorbable suture |
| Pappalardo and Guarnieri, 2014 [2] | Randomized prospective study | Mandibular cyst enucleation | 80 | 40 | 35/45 (bone lid 21/19) | Piezo group 43.2 (21–67); control group 41.4 (20–66) | Mand | 40 | 1 wk | Piezosurgery | None |
| Jung et al., 2013 [10] | Case series | Compromised implant removal/replacement | 10 | 10 | 9/1 | 61.5 (47–89) | Max (4)/mand (6) | 10 | _ | Disc microsaw; shank drill (in some cases in addition to microsaw) | None; microplate (1 case) |
| Khoury, 2013 [9] | Prospective cohort study | Implant explantation; fractured teeth/roots removal; impacted tooth extraction; nerve decompression/lateralization; displaced implant/foreign body removal from sinus | 200 | 200 | 62/138 | 55.3 (19–74) | Max/mand | 200 | ≥4 years (192 cases) | Disc microsaw | None; suture (sinus); micro-screws |
| Oh et al., 2012 [3] | Case-control study (Retrospective) | Mandibular cyst removal | 60 | 34 | 22/38 | 38.5 | Mand | 34 | 13.7 mths (6–24 mths) | _ | Microplates (14); wire (7); resorbable sutures (6); mix (2); none (5) |
| Kurokawa et al., 2002 [51] | Case series | Treatment of odontogenic maxillary sinusitis | 53 | 53 | 32/21 | 44.5 (20–73) | Max | 53 | 2 yrs | Diamond disk | Resorbable suture (45); microplates (8) |
| Choung and Choung, 1997 [52] | Case series | Treatment of maxillary sinusitis; oroantral fistula closure; cyst enucleation; treatment of osteomyelitis; removal of impacted tooth in the sinus | 24 | 24 | 17/7 | 37 (16–66) | Max | 25 | >48 mths | Oscillating saw (round blades); bur (6 cases) | Resorbable suture (20); none (5) |
| Choi et al., 1996 [53] | Randomized prospective study | Displaced tooth removal from sinus; treatment of chronic sinusitis with oroantral communication | 20 | 20 | 8/12 | 46 (25–60) | Max | 20 | 3 mths | Fissure bur and chisel | Resorbable suture |
| Widmark et al., 1992 [54] | Case series | Treatment of maxillary sinusitis; cyst enucleation; displaced tooth removal from sinus; treatment of cases of pain in healthy sinus | 12 | 12 | 6/6 | 45 (26–80) | Max | 13 | 2 (1–4 yrs) | Small drills and osteotome | Resorbable suture |
| Lasaridis et al., 1991 [55] | Case series | Apicectomy of mandibular molars | 21 | 21 | _ | _ | Mand | 24 | At least 6 mths | Round and fine fissure burs | None |
| Khoury and Hensher, 1987 [1] | Case series | Apicectomy of mandibular molars | 75 | 75 | _ | _ | Mand | 75 | 3–6 mths | Round bur and chisel | None; resorbable suture |
| Lindorf, 1984 [56] | Case series | Rhinogenous cause; dentogenous cause; accident; treatment of tumors | 61 | 61 | _ | _ | Max | 70 | 6 mths | Small circular saw | None; resorbable suture; fibrin-based adhesive |
| Application | References | No. of Cases (Bone Lid) | Post-Op Assessment Methods | Main Findings |
|---|---|---|---|---|
| Root-end surgery | Lasaridis et al., 1991 [55] | 24 |
| Healing in resected roots: complete in 19 teeth, uncertain in 4 teeth (16.7%). Complications: unsatisfactory healing in 1 tooth (4.2%); transient paresthesia in 4 cases (resolved within 2 months). |
| Khoury and Hensher, 1987 [1] | 75 |
| Good healing after 3 months in all cases except one, and in the majority complete healing within 6 months. Complications: infection and removal of bone lid in a patient who did not take antibiotics (1 case); in some patients (number not specified) transient postoperative paresthesia resolved within 1 month. | |
| Access to mandibular lesions and impacted teeth | Sukegawa et al., 2021 [46] | 16 |
| Overall, 30 cases; i.e., 16 in the mandible, 11 in the maxilla, and 3 unclear localization (see “other indications”). Bone healing in 27 cases and bone lid necrosis in 3. No significant differences between patients with bone healing and bone lid necrosis as regards age, sex, anatomical variables (jaw, side, cortical bone thickness), lesion size, pathological diagnosis, and osteosynthesis material. Significant differences in smoking (p = 0.005), alcohol intake (p = 0.003), and in the distance of the lesion from the alveolar bone crest (p = 0.037); i.e., in cases of necrosis, the lesions were closer to the alveolar bone crest. Complications: 3 bone lid necrosis (out of 30 total cases): all in the mandible, all in male patients and in presence of smoking habit and alcohol consumption, and all in cases of follicular cyst removal. Average lesion size in cases of necrosis: mesiodistal diameter 13.57 mm (SD 1.03) and buccolingual diameter 11.96 mm (SD 2.15). |
| Ahmed et al., 2018 [47] | 18 |
| Good intraoperative fit of the 3D-printed cutting guide in all patients. Average operative time: 25 min. Pts. showed normal parameters of pain, facial swelling, and maximal mouth opening. Uneventful primary wound healing in all pts.; no signs of infection, flap dehiscence, or bone exposure. Immediate post-op CBCTs showed proper repositioning of the bony segment; 6 months post-op CBCTs showed adequate cortication of the buccal plate of bone and normal bone healing of the sockets in all cases. Complications: Transient lower lip paresthesia in 3 pts., probably owing to pressure during root removal (recovery achieved within 3 months). | |
| Kablan et al., 2017 [48] | 10 |
| Uneventful healing in all cases, but three; in 1 case the bone lid was not repositioned and used for anterior augmentation allowing implant placement in the recipient site. Complications: infection and second surgery for bilateral bone lid removal (in 2 cases in the same pt., in which the bone lids were not fixated); transient hypoesthesia completely resolved after 2 months (in 2 pts.) | |
| Sivolella et al., 2017 [4] | 21 |
| Clinical follow-up 2 weeks post-op: soft tissues healed by primary intention, normal color, no inflammation, no signs of necrosis/suppuration/bone lid exposure. Miniplates were removed in 8 cases (2 for pt. discomfort, 3 for fistula, 3 for prosthetic reasons). Complete radiographic bone defect filling in 18 cases; radiographic integration of the bone lid in 20 cases (in the case of bone necrosis: revision surgery and removal of the necrotic lid); pre-/1 y post CT (11 cases): 93.8% mean reduction in volume of the radiolucent areas; no cyst recurrence. Complications: immediate complications: bleeding/edema (1); ecchymosis (1); IAN paresthesia (3: regressed spontaneously in 2 cases after 2 and 4 months; 1 permanent)—late complications: trismus (1); broken screws during miniplates removal (3); discomfort due to miniplates (2); fistula (2); IAN hypoesthesia (1); bone lid necrosis (1); persistent radiolucent lesion (2). | |
| Pappalardo and Guarnieri, 2014 [2] | 40 |
| Piezosurgery group (bone lid) presented lower pain symptoms, minor swelling, and less recovery time compared to the conventional rotatory-group, and no lesions of mandible nerve. Complications: none in piezosurgery/bone lid group; 2 pts. in conventional group presented with paresthesia 1 week post-op. | |
| Oh et al., 2012 [3] | 34 |
| Correlation between bony healing, determined through panoramic radiographs, and surgical approach (bone lid or not repositioned) was not significant after 6, 12, and 24 months post-op (p <0.05). Complications: none in control group. In bone lid group, 12 pts. with complications: continuous discomfort disappeared after wire removal (2); dysgeusia disappeared after plate removal (1); infection and incision, drainage of abscess, and sequestrectomy (4); recurrent aspects observed and re-surgery performed (3); curettage since bone grafting failed (1); abnormality of bone lid location and removal (1). | |
| Implant explantation | Jung et al., 2013 [10] | 10 |
| Successful implant removal and bone lid repositioning in all cases; in 3 cases, successful immediate implant placement. Complications: none. |
| Khoury, 2013 [9] | 146 |
| Good bone healing in all cases but 3. Complications: in 3 pts., in which implants affected by peri-implantitis were explanted, resorption of the bone lid occurred (3 months post-op: in 1 pt. resorption >30%; in 2 pts. resorption >50%). | |
| Access to the maxillary sinus | Naros et al., 2019 [17] | 21 |
| Complete removal of the fungus ball in all cases. Complications: recurrence after 3 years in 1 case (treated with revision surgery) and insufficient sinus ventilation in 2 cases (treated with revision infundibulotomy). |
| Hu et al., 2018 [26] | 22 |
| Surgeries completed in 20 min. Perfect intra-operative anesthetic effect; small amount of intra-operative blood loss (except in 2 cases); complete removal of all lesions with sinus mucosa preservation; easy repositioning of bone lid, with the use of iodoform gauze due to excessive exudation in 2 cases; durations of pain and swelling (all cases without infraorbital involvement) 2–7 days (mean 3.62 days) and 5–14 days (mean 6.47 days) respectively; no bone resorption and no change in maxillary contour; only 2 cases had mild sinus mucosal thickening. Complications: in 2 cases, intraoperative impulsive bleeding (due to damage of the posterior superior alveolar artery); nasal bleeding (1–3 days) in 8 cases; post-op infection in 1 case (clinical symptoms disappeared after removing miniplate and bone lid and draining for 3 month); in 2 cases, mild sinus mucosal thickening. | |
| Hu et al., 2015 [49] | 10 |
| Surgical procedure was completed within 20 min. All patients healed without oroantral communications. Duration of pain was 3 to 14 days, and swelling was 2 days to 3 months. No pt. developed facial paresthesia or asymmetry. CT scans showed no lesions in the maxillary sinus and the morphology of alveolar bone was normal with little loss of height and width. Complications: 1 pt. experienced discharge and fullness after surgery (settled within 2 months). | |
| Xu et al., 2015 [50] | 20 |
| No need for further treatment except in one case; post-op pain and swelling mild or moderate (none severe); no facial paresthesia; no nasal obstruction; no hemorrhage; no recurrence. Post-op CT: sinus extrusion deformation improved to different degrees and cured chronic maxillary sinusitis. Complications: microplate removal and radical maxillary sinusotomy owing to infection (1 case). | |
| Biglioli and Chiapasco, 2014 [14] | 36 |
| Displaced implants retrieved in all cases; surgical procedure <30 min; uneventful post-op recovery; in all pts. with pain before surgery, complete regression of symptoms; CT (4–6 months post-op): correct stabilization of bone lid, no significant bone lid resorption, and no gap between bone lid margins and surrounding bone; and in the 3 pts. presenting preoperatively with hypertrophic sinus mucosa, 1 complete regression, and in 2, some residual thickening, but with no signs and symptoms of sinusitis. In 12 pts., sinus grafting 12–18 months after bone lid in the same areas and 17 implants placed in the grafted areas 6–9 months later (implant survival rate 100%, and no complications). Complications: none. | |
| Kurokawa et al., 2002 [51] | 53 |
| No sensory impairment of skin and mucosa supplied by the infra-orbital nerve 2 years after surgery (in 4 pts., temporary loss of sensitivity). No loss of dental sensitivity 2 years after surgery (in 2 pts., temporary loss). Radiologically: reimplanted bone remained intact and no scar tissue invaded the maxillary sinus. The drainage window constructed in the lower nasal cavity remained patent. Complications: inflammatory complications in 2 pts. (1 pt. treated without the removal of the reimplanted bone, in 1 pt., removal of the reimplanted bone); 1 case of recurrent sinusitis (successfully treated with Caldwell-Luc method); temporary loss of sensitivity (skin, mucosa) in 4 cases; transient loss of dental sensitivity in 2 cases. | |
| Choung and Choung, 1997 [52] | 25 |
| Exact bone lid repositioning; adequate vascularity of the bone lid; no neurosensory disturbances; normal tooth sensitivity. Complications: facial pain disappeared within 1 month after surgery (1 case). | |
| Choi et al., 1996 [53] | 20 |
| Group A: bone lid as a free bone graft (10 cases); Group B: osteoperiosteal pedicled bone lid (10 cases). Bone lid consolidation: observed in all Group B cases, partial loss of bone lid in 2 cases of Group A. Bone density: significant differences in bone density between the 2 groups (p < 0.05), mean bone reduction 55% in group A, while no reduction in group B; no significant difference in bone density between pts. with and without chronic maxillary sinusitis. Complications: partial loss of bone lid in 2 cases of Group A. | |
| Widmark et al., 1992 [54] | 13 |
| Surgical procedure uneventful in 10 cases out of 12 (in 2 cases, bone lid fragmentation); normal tooth sensitivity; bone lid integration and healthy sinus in most cases. Complications: bone lid fragmentation during surgery (2 cases). Infraorbital nerve injury: 10 days post-op hypoesthesia (8 cases) and paresthesia (1 case)—3 months post-op hypoesthesia (5 cases)—1-year post-op hypoesthesia (3 cases). Radiographic findings (CT): 3 months post-op mild dislocation of the bone lid (1 case) and suspicious of fracture (1 case); 1 year after surgery in 2 cases almost complete opacification of the sinus; in 1 (out of 4) long-term follow-up, pt. had thickened sinus mucosa. | |
| Lindorf, 1984 [56] | 70 |
| A total of 96% of the cases of chronic or sub-acute sinusitis were cured by the first surgical treatment; no loss of dental sensitivity; 3 out of 6 pts with residual problems were cured by appropriate medications. Complications: 3 pts. with residual problems were surgically treated again (1 case of new formation of hemangiomatous fibroma + 2 cases of polypoid sinusitis). | |
| Other indications | Sukegawa et al., 2021 [46] | 14 |
| Access to alveolar bone lesions: 11 in the maxilla and 3 unclear locations. For details, see above. Complications: all in the mandible, none in the maxilla. |
| Khoury, 2013 [9] | 47 |
| Fractured tooth/root and foreign body removal (29 cases) + impacted tooth extraction (14 cases) + inferior alveolar nerve decompression—lateralization (4 cases) Uneventful healing after all procedures. Complications: none. |
| References | D1 | D2 | D3 | D4 | D5 | D6 | D7 | Overall |
|---|---|---|---|---|---|---|---|---|
| Pappalardo & Guarnieri, 2014 [2] | Moderate | Low | Moderate | Low | Low | Low | Moderate | Moderate |
| Choi et al., 1996 [53] | Low | Low | Moderate | Moderate | Low | Low | Moderate | Moderate |
| References | Selection of Participants | Sample Size § | Follow-Up §§ | Drop-Outs §§§ | Measurement of Outcome | Selection of Reported Result | Overall |
|---|---|---|---|---|---|---|---|
| Sukegawa et al., 2021 [46] | Low | Moderate | Moderate | Low | Low | Low | Moderate |
| Naros et al., 2019 [17] | Low | Moderate | Moderate | Low | Low | Low | Moderate |
| Ahmed et al., 2018 [47] | Low | Moderate | Low | Low | Low | Low | Low |
| Hu et al., 2018 [26] | Low | Moderate | High | Low | Low | Low | High |
| Kablan et al., 2017 [48] | Low | High | High | Low | Low | Low | High |
| Sivolella et al., 2017 [4] | Low | Moderate | Moderate | Low | Low | Low | Moderate |
| Hu et al., 2015 [49] | Low | Moderate | Moderate | Low | Low | Low | Moderate |
| Xu et al., 2015 [50] | Low | Moderate | Moderate | Low | Low | Low | Moderate |
| Biglioli and Chiapasco, 2014 [14] | Low | Moderate | Moderate | Moderate | Low | Low | Moderate |
| Jung et al., 2013 [10] | Low | Moderate | Low | Low | Low | Low | Low |
| Khoury, 2013 [9] | Low | Low | Low | Low | Low | Low | Low |
| Oh et al., 2012 [3] | Low | Moderate | Moderate | Low | Low | Low | Moderate |
| Kurokawa et al., 2002 [51] | Low | Low | Moderate | High | Low | Low | High |
| Choung and Choung, 1997 [52] | Low | Moderate | High | Moderate | Low | Low | High |
| Widmark et al., 1992 [54] | Low | Moderate | High | Low | Low | Low | High |
| Lasaridis et al., 1991 [55] | Low | Moderate | Moderate | Low | Low | Low | Moderate |
| Khoury and Hensher, 1987 [1] | Low | High | Moderate | Low | Low | Low | High |
| Lindorf, 1984 [56] | Low | Low | Moderate | Low | Low | Low | Low |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sivolella, S.; Brunello, G.; Panda, S.; Schiavon, L.; Khoury, F.; Del Fabbro, M. The Bone Lid Technique in Oral and Maxillofacial Surgery: A Scoping Review. J. Clin. Med. 2022, 11, 3667. https://doi.org/10.3390/jcm11133667
Sivolella S, Brunello G, Panda S, Schiavon L, Khoury F, Del Fabbro M. The Bone Lid Technique in Oral and Maxillofacial Surgery: A Scoping Review. Journal of Clinical Medicine. 2022; 11(13):3667. https://doi.org/10.3390/jcm11133667
Chicago/Turabian StyleSivolella, Stefano, Giulia Brunello, Sourav Panda, Lucia Schiavon, Fouad Khoury, and Massimo Del Fabbro. 2022. "The Bone Lid Technique in Oral and Maxillofacial Surgery: A Scoping Review" Journal of Clinical Medicine 11, no. 13: 3667. https://doi.org/10.3390/jcm11133667






