New Safety Aspects in Corneal Donation—Studies on SARS-CoV-2-Positive Corneal Donors
Abstract
:1. Introduction
2. Materials and Methods
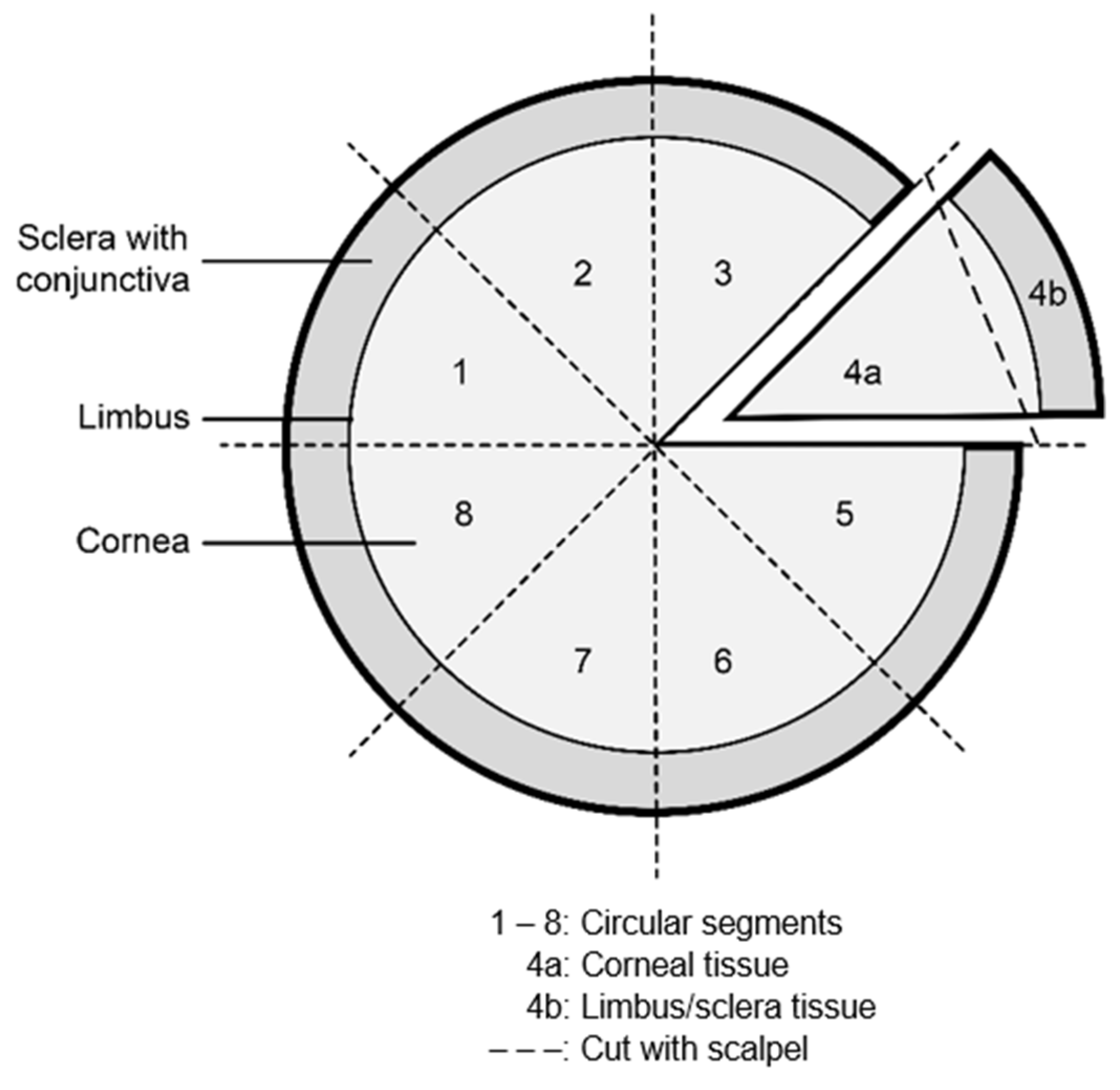
2.1. Human Sample Preparation and Cultivation
2.2. Test Kits Used for SARS-CoV-2 Detection
2.3. Subgenomic RNA Analysis
2.4. Immunohistochemistry
3. Results
3.1. Case History
3.2. SARS-CoV-2 Detection in Corneal Tissue and Related Culture Medium Using qRT–PCR
3.3. Subgenomic RNA Analysis
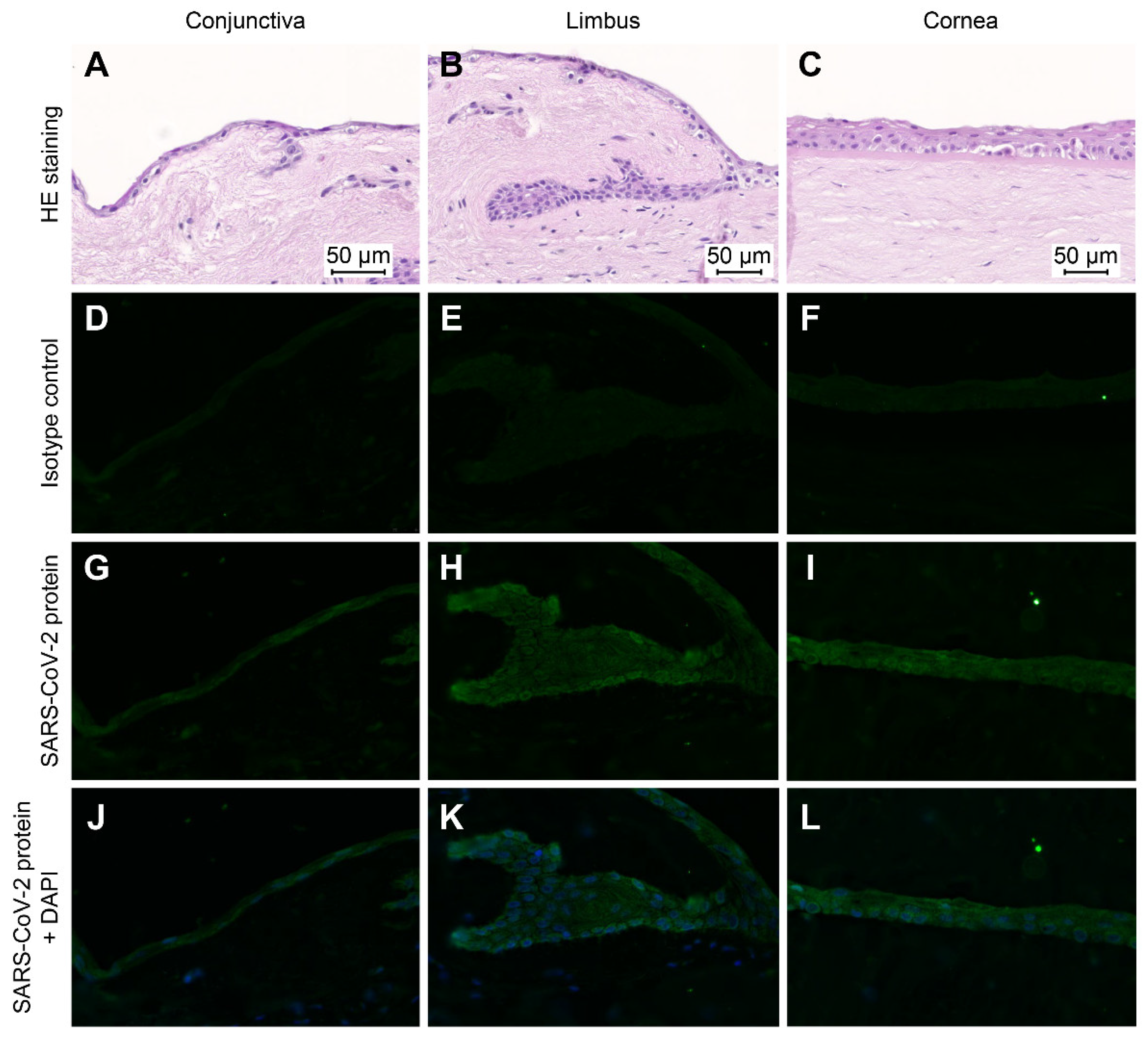
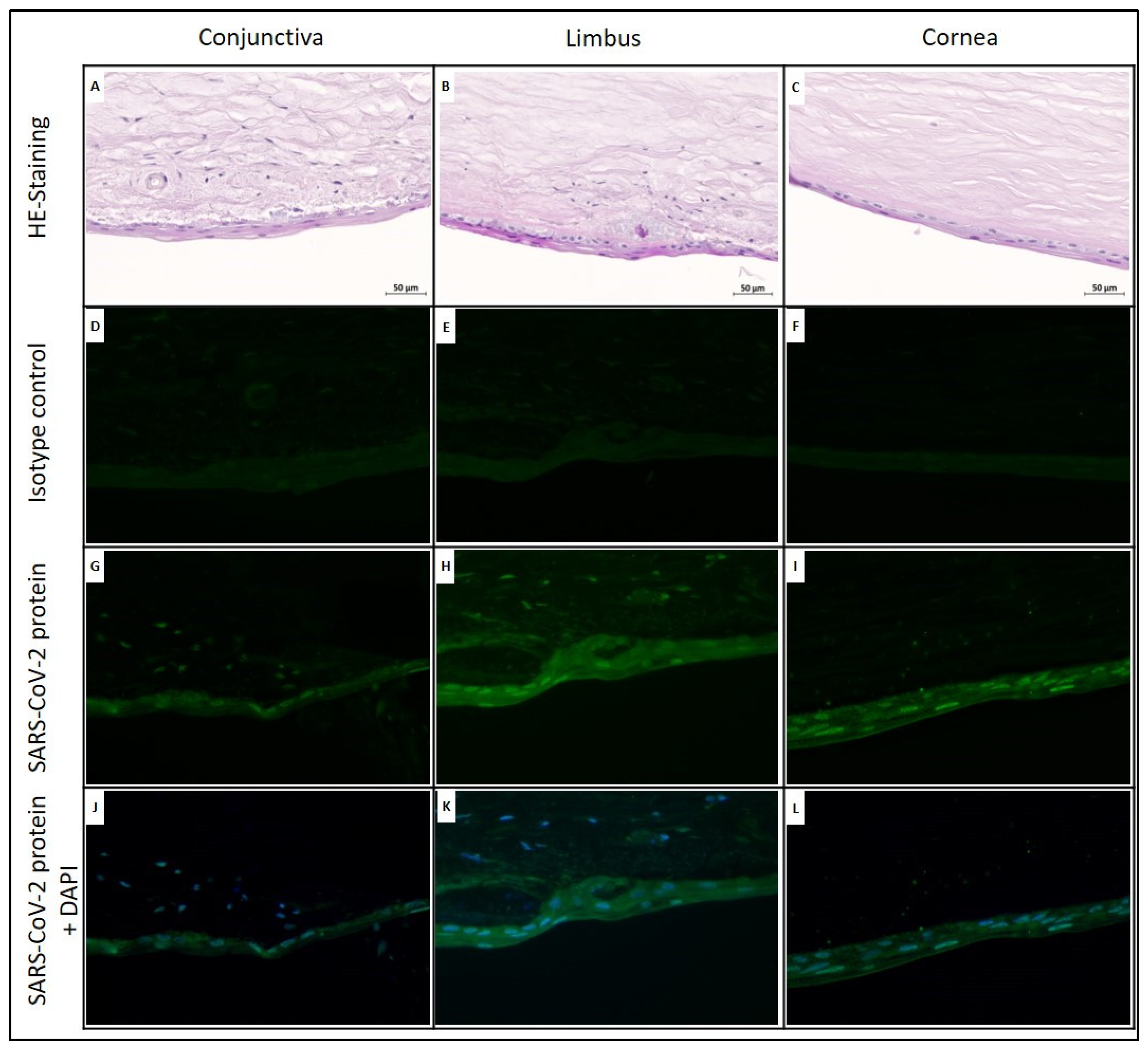
3.4. Immunohistochemical Staining for SARS-CoV-2
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bullard, J.; Dust, K.; Funk, D.; Strong, J.E.; Alexander, D.; Garnett, L.; Boodman, C.; Bello, A.; Hedley, A.; Schiffman, Z.; et al. Predicting infectious severe acute respiratory syndrome coronavirus 2 from diagnostic samples. Clin. Infect. Dis. 2020, 71, 2663–2666. [Google Scholar] [CrossRef] [PubMed]
- Casagrande, M.; Fitzek, A.; Spitzer, M.S.; Puschel, K.; Glatzel, M.; Krasemann, S.; Norz, D.; Lutgehetmann, M.; Pfefferle, S.; Schultheiss, M. Presence of SARS-CoV-2 RNA in the cornea of viremic patients with COVID-19. JAMA Ophthalmol. 2021, 139, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Azzolini, C.; Donati, S.; Premi, E.; Baj, A.; Siracusa, C.; Genoni, A.; Grossi, P.A.; Azzi, L.; Sessa, F.; Dentali, F.; et al. SARS-CoV-2 on Ocular Surfaces in a Cohort of Patients with COVID-19 from the Lombardy Region, Italy. JAMA Ophthalmol. 2021, 139, 956–963. [Google Scholar] [CrossRef] [PubMed]
- Bayyoud, T.; Iftner, T.; Bartz-Schmidt, K.U.; Rohrbach, J.M.; Ueffing, M.; Schindler, M.; Thaler, S. First results of investigations of SARS-CoV-2 RNA in human corneal tissue. Ophthalmologe 2021, 118, 78–80. [Google Scholar] [CrossRef] [PubMed]
- Miner, J.J.; Platt, D.J.; Ghaznavi, C.M.; Chandra, P.; Santeford, A.; Menos, A.M.; Dong, Z.; Wang, E.R.; Qian, W.; Karozichian, E.S.; et al. HSV-1 and zika virus but not SARS-CoV-2 replicate in the human cornea and are restricted by corneal type III interferon. Cell Rep. 2020, 33, 108339. [Google Scholar] [CrossRef]
- Wolfel, R.; Corman, V.M.; Guggemos, W.; Seilmaier, M.; Zange, S.; Muller, M.A.; Niemeyer, D.; Jones, T.C.; Vollmar, P.; Rothe, C.; et al. Virological assessment of hospitalized patients with COVID-2019. Nature 2020, 581, 465–469. [Google Scholar] [CrossRef] [Green Version]
- Vogels, C.B.F.; Brito, A.F.; Wyllie, A.L.; Fauver, J.R.; Ott, I.M.; Kalinich, C.C.; Petrone, M.E.; Casanovas-Massana, A.; Catherine Muenker, M.; Moore, A.J.; et al. Analytical sensitivity and efficiency comparisons of SARS-CoV-2 RT-qPCR primer-probe sets. Nat. Microbiol. 2020, 5, 1299–1305. [Google Scholar] [CrossRef]
- Pfefferle, S.; Huang, J.; Norz, D.; Indenbirken, D.; Lutgehetmann, M.; Oestereich, L.; Gunther, T.; Grundhoff, A.; Aepfelbacher, M.; Fischer, N. Complete genome sequence of a SARS-CoV-2 strain isolated in Northern Germany. Microbiol. Resour. Announc. 2020, 9, e00520-20. [Google Scholar] [CrossRef]
- Salz, A.K.; Acharya, M.; Hofmann, N.; Wittmershaus, I.; Sangwan, V.; Borgel, M.; Mathur, U. Risk of SARS-CoV-2 virus transmission from donor corneal tissue: A review. Indian J. Ophthalmol. 2021, 69, 1592–1597. [Google Scholar] [CrossRef]
- Levine, H.; Sepulveda-Beltran, P.A.; Altamirano, D.S.; Sabater, A.L.; Dubovy, S.R.; Flynn, H.W.; Amescua, G. Risk and Impact of Severe Acute Respiratory Syndrome Coronavirus 2 Infection on Corneal Transplantation: A Case-Control Study. Cornea 2022, 41, 224–231. [Google Scholar] [CrossRef]
- Wille, D.; Heinzelmann, J.; Hofmann, N.; Borgel, M.; Kehlen, A.; Muller, A.; Viestenz, A. Case report-a cornea donor with a positive SARS-CoV-2 finding. Ophthalmologe 2020, 118, 710–713. [Google Scholar] [CrossRef] [PubMed]
- Trigaux, C.; Salla, S.; Schroeter, J.; Tourtas, T.; Thomasen, H.; Maier, P.; Hellwinkel, O.J.C.; Wittmershaus, I.; Merz, P.R.; Seitz, B.; et al. SARS-CoV-2: Impact on, risk assessment and countermeasures in german eye banks. Curr. Eye Res. 2021, 46, 666–671. [Google Scholar] [CrossRef] [PubMed]
- Thaler, S.; Schindler, M.; Iftner, T.; Bartz-Schmidt, K.U.; Bayyoud, T. Importance of corneal organ culture in donors with possible SARS-CoV-2 infections. Ophthalmologe 2020, 117, 622–625. [Google Scholar] [CrossRef]
- Hoffmann, M.; Kleine-Weber, H.; Schroeder, S.; Kruger, N.; Herrler, T.; Erichsen, S.; Schiergens, T.S.; Herrler, G.; Wu, N.H.; Nitsche, A.; et al. SARS-CoV-2 Cell Entry Depends on ACE2 and TMPRSS2 and Is Blocked by a Clinically Proven Protease Inhibitor. Cell 2020, 181, 271–280. [Google Scholar] [CrossRef]
- Lange, C.; Wolf, J.; Auw-Haedrich, C.; Schlecht, A.; Boneva, S.; Lapp, T.; Agostini, H.; Martin, G.; Reinhard, T.; Schlunck, G. What is the significance of the conjunctiva as a potential transmission route for SARS-CoV-2 infections? Ophthalmologe 2021, 118, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Zhou, L.; Xu, Z.; Castiglione, G.M.; Soiberman, U.S.; Eberhart, C.G.; Duh, E.J. ACE2 and TMPRSS2 are expressed on the human ocular surface, suggesting susceptibility to SARS-CoV-2 infection. Ocul. Surf. 2020, 18, 537–544. [Google Scholar] [CrossRef] [PubMed]
- Collin, J.; Queen, R.; Zerti, D.; Dorgau, B.; Georgiou, M.; Djidrovski, I.; Hussain, R.; Coxhead, J.M.; Joseph, A.; Rooney, P.; et al. Co-expression of SARS-CoV-2 entry genes in the superficial adult human conjunctival, limbal and corneal epithelium suggests an additional route of entry via the ocular surface. Ocul. Surf. 2021, 19, 190–200. [Google Scholar] [CrossRef]
- Roehrich, H.; Yuan, C.; Hou, J.H. Immunohistochemical Study of SARS-CoV-2 Viral Entry Factors in the Cornea and Ocular Surface. Cornea 2020, 39, 1556–1562. [Google Scholar] [CrossRef]
- Sungnak, W.; Huang, N.; Becavin, C.; Berg, M.; Queen, R.; Litvinukova, M.; Talavera-Lopez, C.; Maatz, H.; Reichart, D.; Sampaziotis, F.; et al. SARS-CoV-2 entry factors are highly expressed in nasal epithelial cells together with innate immune genes. Nat. Med. 2020, 26, 681–687. [Google Scholar] [CrossRef] [Green Version]
- Alexandersen, S.; Chamings, A.; Bhatta, T.R. SARS-CoV-2 genomic and subgenomic RNAs in diagnostic samples are not an indicator of active replication. Nat. Commun. 2020, 11, 6059. [Google Scholar] [CrossRef]
- Wong, C.H.; Ngan, C.Y.; Goldfeder, R.L.; Idol, J.; Kuhlberg, C.; Maurya, R.; Kelly, K.; Omerza, G.; Renzette, N.; De Abreu, F.; et al. Subgenomic RNAs as molecular indicators of asymptomatic SARS-CoV-2 infection. bioRxiv 2021. [Google Scholar] [CrossRef]
- Verma, R.; Kim, E.; Martinez-Colon, G.J.; Jagannathan, P.; Rustagi, A.; Parsonnet, J.; Bonilla, H.; Khosla, C.; Holubar, M.; Subramanian, A.; et al. SARS-CoV-2 Subgenomic RNA Kinetics in Longitudinal Clinical Samples. Open Forum Infect. Dis. 2021, 8, ofab310. [Google Scholar] [CrossRef] [PubMed]
- Raaben, M.; Posthuma, C.C.; Verheije, M.H.; Te Lintelo, E.G.; Kikkert, M.; Drijfhout, J.W.; Snijder, E.J.; Rottier, P.J.; de Haan, C.A. The ubiquitin-proteasome system plays an important role during various stages of the coronavirus infection cycle. J. Virol. 2010, 84, 7869–7879. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, H.Y.; Tu, J.L.; Cao, C.L.; Yang, T.; Gao, L.C. Proteasome activator PA28 gamma-dependent degradation of coronavirus disease (COVID-19) nucleocapsid protein. Biochem. Biophys. Res. Commun. 2020, 529, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Moriishi, K.; Okabayashi, T.; Nakai, K.; Moriya, K.; Koike, K.; Murata, S.; Chiba, T.; Tanaka, K.; Suzuki, R.; Suzuki, T.; et al. Proteasome activator PA28 gamma-dependent nuclear retention and degradation of hepatitis C virus core protein. J. Virol. 2003, 77, 10237–10249. [Google Scholar] [CrossRef] [Green Version]
- Ko, N.L.; Taylor, J.M.; Bellon, M.; Bai, X.T.; Shevtsov, S.P.; Dundr, M.; Nicot, C. PA28 gamma is a novel corepressor of HTLV-1 replication and controls viral latency. Blood 2013, 121, 791–800. [Google Scholar] [CrossRef]
- Yan, Y.; Diao, B.; Liu, Y.; Zhang, W.; Wang, G.; Chen, X. Severe acute respiratory syndrome coronavirus 2 nucleocapsid protein in the ocular tissues of a patient previously infected with coronavirus disease 2019. JAMA Ophthalmol. 2020, 138, 1201–1204. [Google Scholar] [CrossRef]
- Chen, X.H.; Yu, H.M.; Mei, T.; Chen, B.; Chen, L.W.; Li, S.L.; Zhang, X.; Sun, X.F. SARS-CoV-2 on the ocular surface: Is it truly a novel transmission route? Br. J. Ophthalmol. 2021, 105, 1190–1195. [Google Scholar] [CrossRef]
- Qu, J.Y.; Xie, H.T.; Zhang, M.C. Evidence of SARS-CoV-2 transmission through the ocular route. Clin. Ophthalmol. 2021, 15, 687–696. [Google Scholar] [CrossRef]
- Armstrong, L.; Collin, J.; Mostafa, I.; Queen, R.; Figueiredo, F.C.; Lako, M. In the eye of the storm: SARS-CoV-2 infection and replication at the ocular surface? Stem Cells Transl. Med. 2021, 10, 976–986. [Google Scholar] [CrossRef]
| Characteristics | Case 1 | Case 2 | Case 3 | Case 4 |
|---|---|---|---|---|
| Age of death in years | 62 | 67 | 55 | 72 |
| Sex | Male | Male | Female | Female |
| Prior nonophthalmic history | Severe mesenteric ischemia, pronounced generalized arteriosclerosis, therapy-resistant Crohn’s disease | Peripheral arterial occlusive disease with forefoot infection; death because of multimorbidity with decompensated heart failure and acute renal failure | Obesity, severe heart disease, diabetes and COPD | Stroke, arterial thrombus, arterial hypertension, diabetes mellitus and peripheral arterial occlusive disease |
| SARS-CoV-2 vaccination | No | No | No | No |
| SARS-CoV-2 symptoms | No | No | No | No |
| Premortem lateral flow test | Negative | Negative | Negative | Negative |
| Latest premortem qRT–PCR test | 6 weeks before death (positive, CT > 30) | 3 weeks before death (negative) | 4 days before death (negative) | - |
| Premortem serum antibody test for SARS-CoV-2 | Negative for antibodies (IgA, IgG) | Negative for antibodies (IgG, IgG II) | Negative for antibodies (IgG, IgG II) | Negative for antibodies (IgG, IgG II) |
| Postmortem conjunctival and nasopharyngeal swab test (qRT–PCR) for SARS-CoV-2 | Positive (CT value of 20.7 (S and N gene, Anchor)) | Positive (CT values of 21.7 (S and N gene, Anchor), 20.4 (E gene, Cepheid), 22.7 (N2 gene, Cepheid)) | Positive (CT value of 16.2 (S and N gene, Anchor)) | Positive (CT value of 39.2 (N and RdRP gene, Abbott)) |
| Strain | Unknown | B.1.177 | Unknown | Unknown |
| Time of detection (days after death) | 4 | 7 | 1 | 4 |
| Sampling | Case 1 | Case 2 | Case 3 | Case 4 | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample CS/CM | CT Value | Sample CS/CM | CT Value | Sample CS/CM | CT Value | Sample CS/CM | CT Value | ||||
| Cornea Graft: L | Cornea Graft: R | Cornea Graft: L | Cornea Graft: R | Cornea Graft: L | Cornea Graft: R | Cornea Graft: L | |||||
| 2 d | CS | 32.8 | 35.0 | ||||||||
| CM (o) b | 30.6 | 32.2 | |||||||||
| 5 d | CS a | neg | |||||||||
| CM (o) b | 38.0 | ||||||||||
| 7 d | CS | neg | CS | 34.3 | 34.3 | CS | 33.7 | 35.0 | CS | neg | neg |
| CM (o) b | 39.8 | CM (n) b | neg | neg | Li/Scl | 31.6 | 33.4 | CM (o) b | neg | neg | |
| CM (n) b | neg | Cornea | neg | neg | |||||||
| CM (o) b | 31.3 | 33.7 | |||||||||
| 14 d | CS | neg | CS | 36.3 | 32.4 | CS | 32.4 | 33.4 | |||
| CM (o) b | neg | CM (n) b | neg | neg | Li/Scl | 35.9 | 34.1 | ||||
| CM (n) b | neg | Cornea | 37.2 | neg | |||||||
| CM (o) b | 31.3 | 31.3 | |||||||||
| CM (n) b | 36.0 | neg | |||||||||
| 21 d | CS | 35.9 | neg | CS | 33.9 | 36.5 | |||||
| Li/Scl | 35.4 | 33.1 | Li/Scl | 33.2 | 37.8 | ||||||
| Cornea | 39.1 | neg | Cornea | neg | neg | ||||||
| CM (o) b | 31.5 | 34.2 | |||||||||
| CM (n) b | neg | neg | |||||||||
| 28 d | 1/8 CS | neg | 35.1 | 1/12 CS | 34.5 | 37.3 | |||||
| Li/Scl | 35.2 | neg | Li/Scl | 34.5 | 39.2 | ||||||
| Cornea | 37.5 | neg | Cornea | neg | neg | ||||||
| CM (o) b | 32.3 | 34.5 | |||||||||
| CM (n) b | neg | neg | |||||||||
| 32 d | 1/8 CS fixed | - | - | 1/12 CS fixed | - | - | |||||
| Sampling | Sample | Detection a (CT Value) | N1 (CT Value) | sg N1 (CT Value) | Delta CT | |
|---|---|---|---|---|---|---|
| 7 d | R | 1/8 CS | 34.3 | 31.9 | 35.3 | −3.4 |
| L | 1/8 CS | 34.3 | 32.3 | 36.4 | −4.1 | |
| 21 d | L | 1/8 CS | - | - | - | - |
| Li/Scl | 33.1 | 31.6 | 35.6 | −4.0 | ||
| Cornea | - | - | - | - | ||
| R | 1/8 CS | 35.9 | 34.8 | - | - | |
| Li/Scl | 35.4 | 34.3 | 35.8 | - | ||
| Cornea | 39.1 | - | - | - | ||
| Cell culture supernatant (ctrl) | 20.5 | 25.5 | −5.2 | |||
| Sampling | Sample | Detection a (CT Value) | N1 (CT Value) | sg N1 (CT Value) | Delta CT | |
|---|---|---|---|---|---|---|
| 7 d | L | 1/12 CS | 35.0 | 32.4 | 36.3 | −3.9 |
| Li/Scl | 33.4 | 31.2 | 34.3 | −3.1 | ||
| Cornea | - | - | - | - | ||
| R | 1/12 CS | 33.7 | 31.2 | 36.3 | −5.1 | |
| Li/Scl | 31.6 | 29.3 | 34.8 | −5.5 | ||
| Cornea | - | 37.2 | - | - | ||
| 14 d | L | 1/12 CS | 33.4 | 33.2 | 37.4 | −4.2 |
| Li/Scl | 34.1 | 32.9 | - | - | ||
| Cornea | - | - | - | - | ||
| CM (o) | 31.3 | 31.9 | - | - | ||
| CM (n) | - | - | - | - | ||
| R | 1/12 CS | 32.4 | 32.2 | 36.5 | −4.3 | |
| Li/Scl | 35.9 b | |||||
| Cornea | 37.2 | 36.1 | 37.4 | n.d. c | ||
| CM (o) | 31.3 | 29.2 | 33.8 | −4.6 | ||
| CM (n) | 36.0 | - | - | - | ||
| 21 d | L | 1/12 CS | 36.5 | 32.9 | - | - |
| Li/Scl | 37.8 | 34.3 | - | - | ||
| Cornea | - | - | - | - | ||
| R | 1/12 CS | 33.9 | 29.6 | 35.6 | −6 | |
| Li/Scl | 33.2 | 29.9 | 36.4 | −6.5 | ||
| Cornea | - | 36.8 | - | - | ||
| Cell culture supernatant (ctrl) | 20.5 | 25.7 | −5.2 | |||
| Cultivation Time (d) | Ocular Tissue | IHC Staining of SARS-CoV-2 Protein | |
|---|---|---|---|
| Cornea: R | Cornea: L | ||
| 7 | Conjunctiva | + | ++ |
| Limbus | ++ | + | |
| Cornea | ++ | + | |
| 32 | Conjunctiva | + | +++ |
| Limbus | +++ | + | |
| Cornea | ++ | + | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wille, D.; Heinzelmann, J.; Kehlen, A.; Lütgehetmann, M.; Nörz, D.S.; Siebolts, U.; Mueller, A.; Karrasch, M.; Hofmann, N.; Viestenz, A.; et al. New Safety Aspects in Corneal Donation—Studies on SARS-CoV-2-Positive Corneal Donors. J. Clin. Med. 2022, 11, 3312. https://doi.org/10.3390/jcm11123312
Wille D, Heinzelmann J, Kehlen A, Lütgehetmann M, Nörz DS, Siebolts U, Mueller A, Karrasch M, Hofmann N, Viestenz A, et al. New Safety Aspects in Corneal Donation—Studies on SARS-CoV-2-Positive Corneal Donors. Journal of Clinical Medicine. 2022; 11(12):3312. https://doi.org/10.3390/jcm11123312
Chicago/Turabian StyleWille, Diana, Joana Heinzelmann, Astrid Kehlen, Marc Lütgehetmann, Dominik S. Nörz, Udo Siebolts, Anke Mueller, Matthias Karrasch, Nicola Hofmann, Anja Viestenz, and et al. 2022. "New Safety Aspects in Corneal Donation—Studies on SARS-CoV-2-Positive Corneal Donors" Journal of Clinical Medicine 11, no. 12: 3312. https://doi.org/10.3390/jcm11123312
APA StyleWille, D., Heinzelmann, J., Kehlen, A., Lütgehetmann, M., Nörz, D. S., Siebolts, U., Mueller, A., Karrasch, M., Hofmann, N., Viestenz, A., Börgel, M., Kuhn, F., & Viestenz, A. (2022). New Safety Aspects in Corneal Donation—Studies on SARS-CoV-2-Positive Corneal Donors. Journal of Clinical Medicine, 11(12), 3312. https://doi.org/10.3390/jcm11123312







