Introduction
We report the case of a patient with a history of mitral valve replacement and a giant left atrium with acute transmural anterior myocardial infarction and concomitant acute occlusion of the right superficial femoral artery.
We emphasise the crucial role of twodimensional transthoracic (TTE) and transoesophageal echocardiography (TEE) in defining anatomical and functional aspects. Antithrombotic drug prevention as well as surgical strategies are also briefly discussed.
Description
A 72-year-old women with a history of mitral valve replacement (Carbo Medics™, 31 mm, F) because of severe mitral stenosis seven years before, presented at the emergency department with acute dyspnoea following typical acute chest pain occurring 36 hours before admission. She also complained of acute occurring claudication (Rutherford 3) since two days. Medical history was uneventful apart from the rheumatic heart disease: there were no cardiovascular risk factors, no previous history of claudication, and coronary angiography performed before valve replacement was normal.
On physical examination the patient presented with acute dyspnea at rest, tachyarrhythmia (120–140 beats/min). Arterial blood pressure was 140/80 mm Hg. At cardiac auscultation loud opening and closing mitral clicks, and a grade 2 systolic murmur was heard, unchanged when compared to the findings reported at the preceding ambulatory examinations. Arterial pulses of the posterior tibial and dorsalis pedis arteries of the right leg were absent.
Electrocardiogram revealed atrial fibrillation (130–140 beats/min), and 0,04 second Q waves and negative T waves in the precordial V1 to V4 leads, which were not present in the preceding ECG-recordings. Chest X-ray showed enlarged left atrium, and evidence of moderate pulmonary vein congestion. Troponin I was 9,77 ng/ml (<0.10 ng/ml), creatinine kinase 1416 IU/l (0–160 IU/l) and INR was 2.5 (mean INR values during the preceding 12 months were 3.1; maximum and minimal INR values were 4.1 and 2.8 respectively).
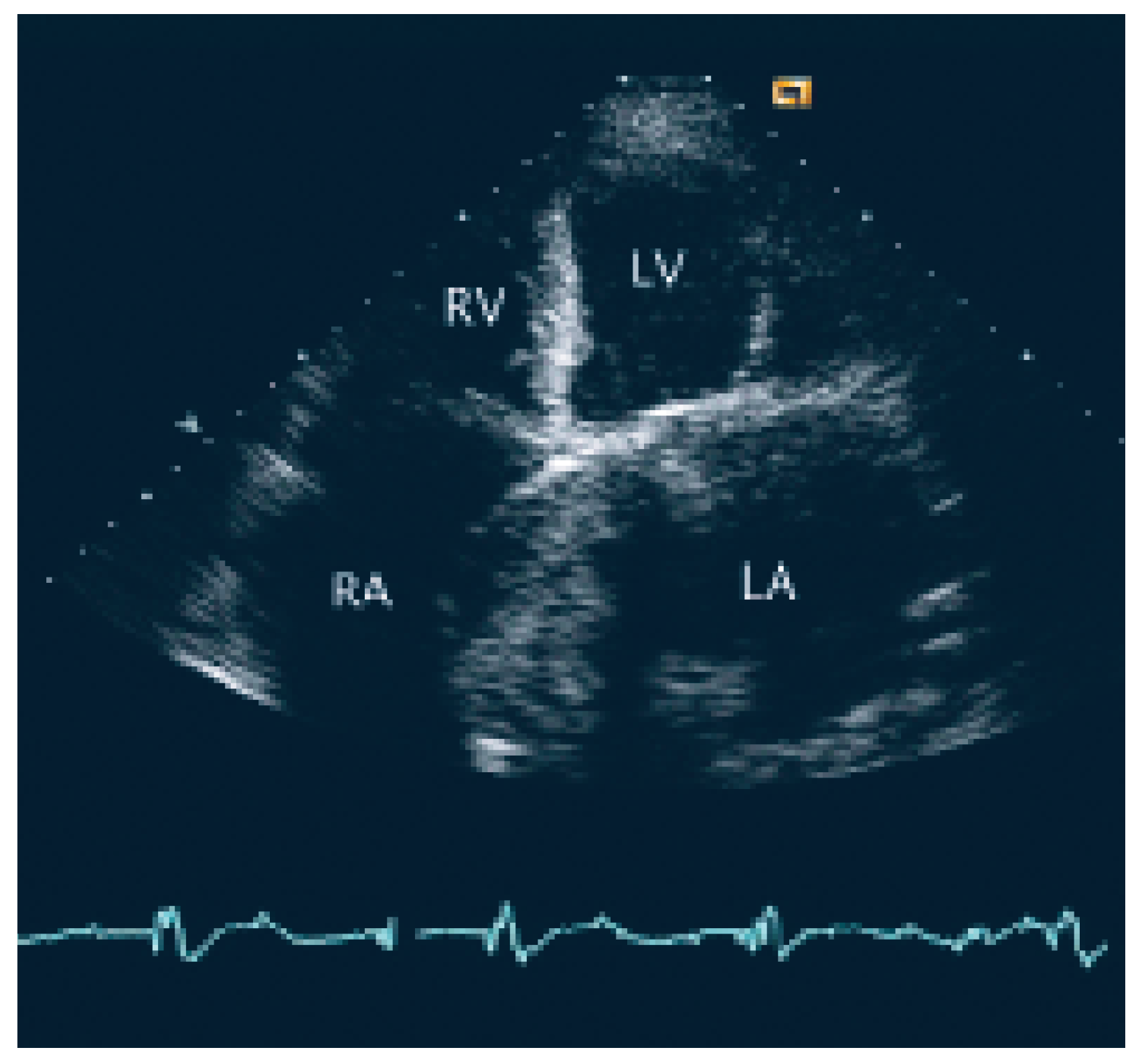
The patient was transferred to the intermediary care unit with the clinical diagnosis of subacute transmural anterior myocardial infarction. TTE showed a giant left atrium (9 cm × 12 cm × 9 cm; 509 cm3) and a large aneurysm of the atrial septum with compression of the right atrium (
Figure 1) also as an apical scar, compatible with subacute myocardial infarction (
Figure 1).
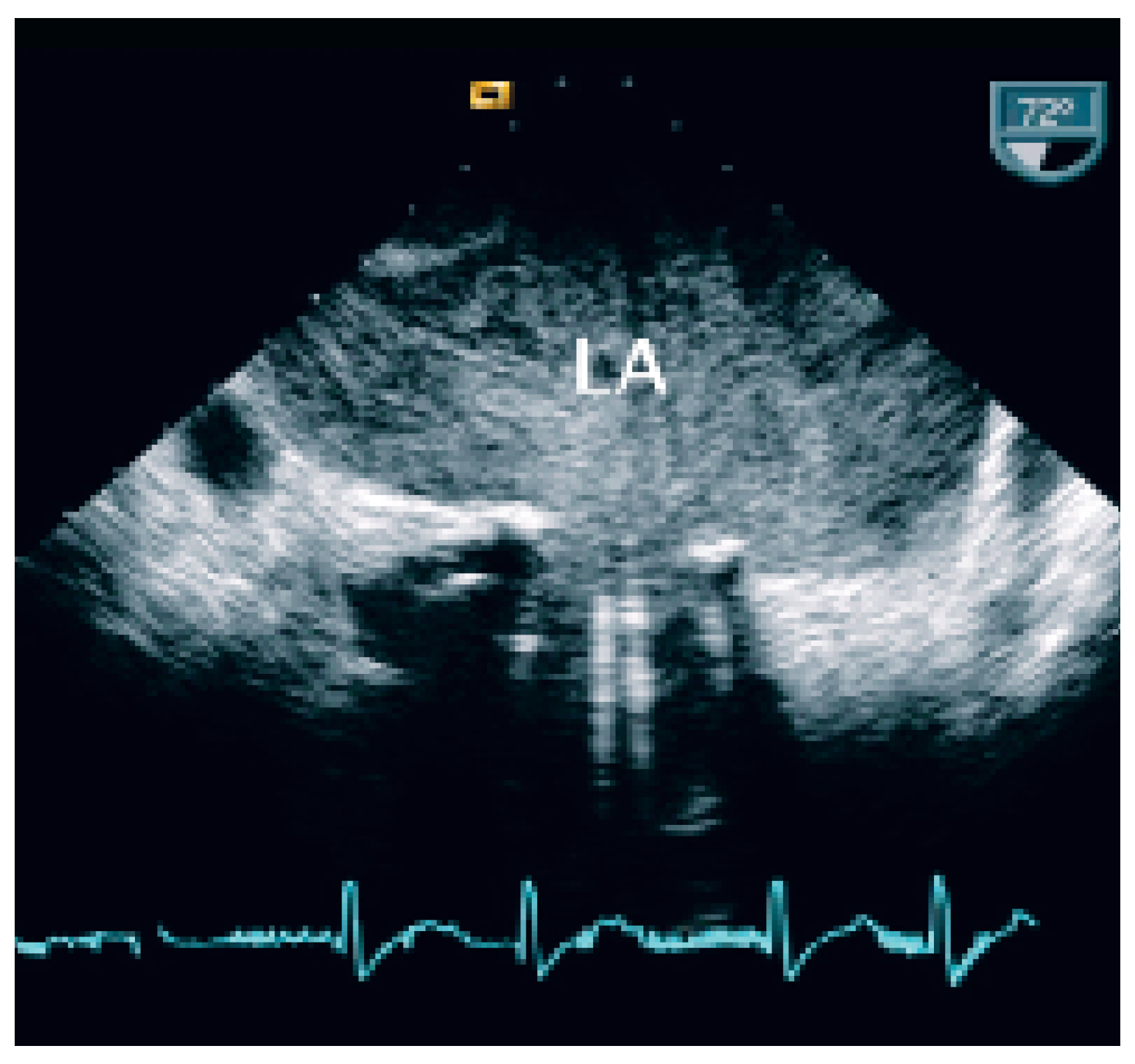
At TEE severe spontaneous echocontrast in the left atrium (
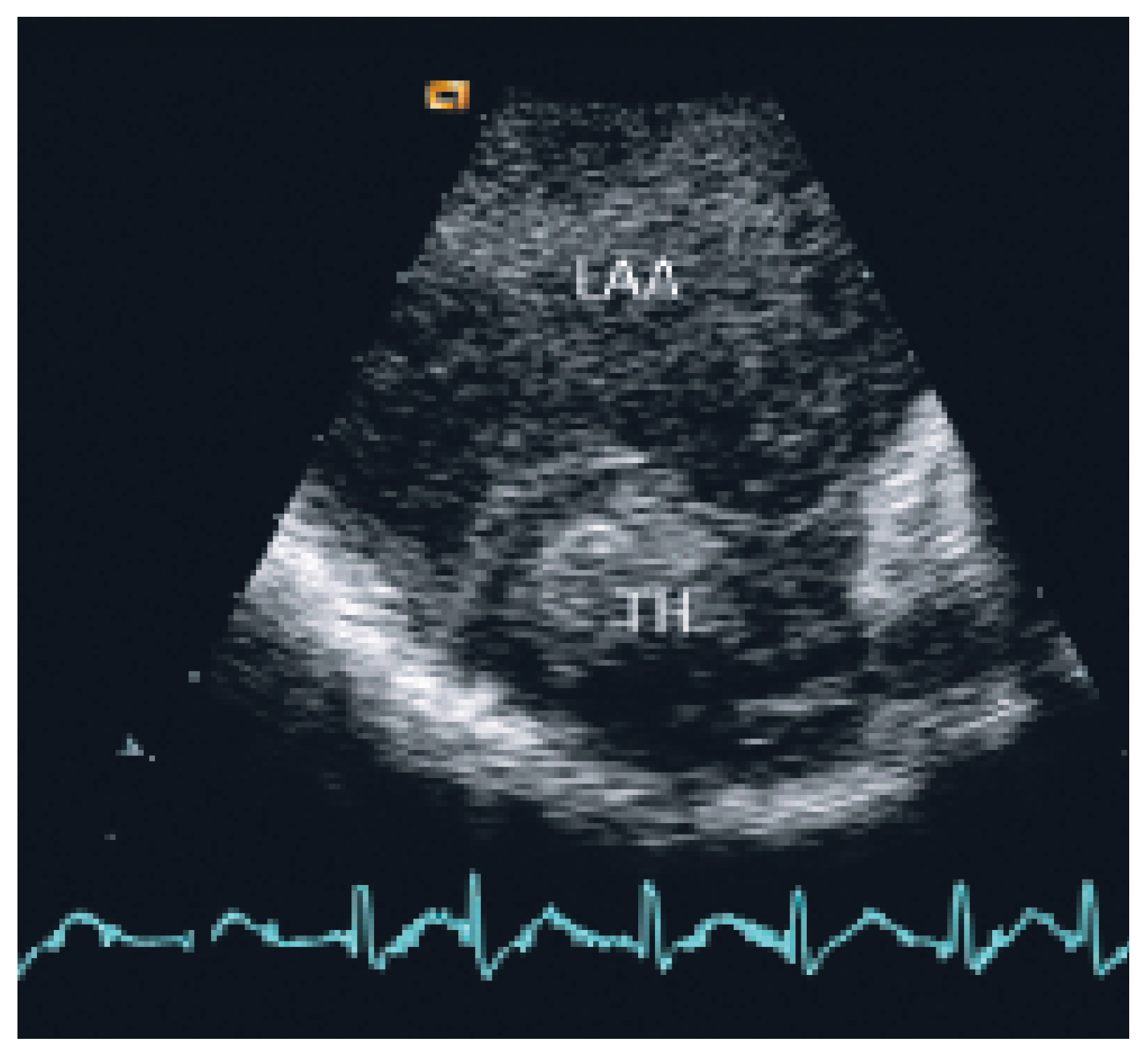
Figure 2) and a thrombus (2.7 cm × 3.5 cm) in the left atrial appendix were present (
Figure 3). There was no evidence of impairment of the beleaflet mechanical valve (mean transvalvular gradient 4 mm Hg). Anklebrachial pressure index was abnormal (0.5), and duplex ultrasounds showed acute thromboembolic occlusion of right superficial femoral artery.
The patient was treated with atenolol (50 mg/d) and enalapril (10 mg/d) and endovenous nonfractionated heparin until a stable INR threshold of at least 3.5 was obtained, plus clopidogrel 75 mg/day.
Hospital and post-discharge follow-up of 12 months were uneventful with no further cardiac symptoms and with spontaneous recovery of claudicatio. No further embolic or haemorrhagic complication occurred under oral anticoagulation and clopidogrel.
Given the absence of risk factors, previous normal coronary angiography, the suboptimal INR values and the concomitant episode of acute limb ischaemia, we hypothesised that the patient suffered acute myocardial infarction following arterial embolisation from the giant left atrium in the left anterior descending artery and in the superficial femoral artery.
Discussion
As cited in Hurst’s memories [
1] “… giant left atrium is defined as one that touches the right lateral side of the chest wall. The condition is caused by rheumatic mitral valve disease and atrial fibrillation is always present …”. This case illustrates the pivotal role of echocardiography in defining and quantifying this pathology and the associated thromboembolic risk. TTE and particularly TEE allowed to assess the magnitude of the giant left atrium (
Figure 1), the presence of spontaneous contrast and intracardiac thrombus (
Figure 2 and 3), the presence of normal functioning of the mechanical valve prosthesis, and the occurrence of a new apical dyskinesia compatible with the diagnosis of acute myocardial infarction [
2].
Our patient with a giant left atrium, and a history of mitral valve disease with mechanical valve replacement seven years earlier associated with left atrial fibrillation was at highest risk of thromboembolic complications. The clinical picture of acute myocardial infarction and concomitant peripheral arterial occlusion in this patient without risk factors for atherosclerosis and with normal previous coronary angiography was compatible with multiple cardiac emboli from the giant left atrium into the LAD and in the superficial femoral artery. Our patient had a mean INR value in the previous twelve months before of 3.1. For mechanical prostheses in the mitral position, the INR should be maintained between 2.5 and 3.5 [
3,
4]. According to the ACC/AHA guidelines for the management of patients with valvular heart disease the addition of aspirin (80 to 100 mg/d) to warfarin should be strongly considered unless there is a contraindication to the use of aspirin (ie bleeding or aspirin intolerance) [
5]. This combination seems to be particularly appropriate in patients who have had an embolus while on warfarin therapy [
5] as it was the case in our patient. Oral direct thrombin inhibitors are safe and effective in patients with atrial fibrillation, and may be an alternative strategy in the future for similar cases, although there is no data available at the moment, using these drugs in patients with prosthetic heart valves [
6].
Although giant left atrium is not necessarily associated with atrial embolism, according to a recent publication [
7] our case had several aggravating factors favoring thromboembolism (atrial fibrillation, mechanical valve in mitral position).
Surgical reduction of giant left atrium also has been previously proposed by several authors using different techniques [
6,
8,
9]. However, surgical repair is usually performed in concomitance with mitral valve surgery. In our patient with normal functioning mitral valve prosthesis, surgical reduction of the giant left atrium should have been better performed at the time of elective mitral valve replacement seven years before. This option should be reconsidered in our patient in case of further cardiac embolisation in spite of the more aggressive antithrombotic treatment, which included warfarin with an INR target value of 3.5 to 4.0 associated with clopidogrel 75 mg/day.