A Wide Complex Tachycardia in a 31-Year-Old Male
Abstract
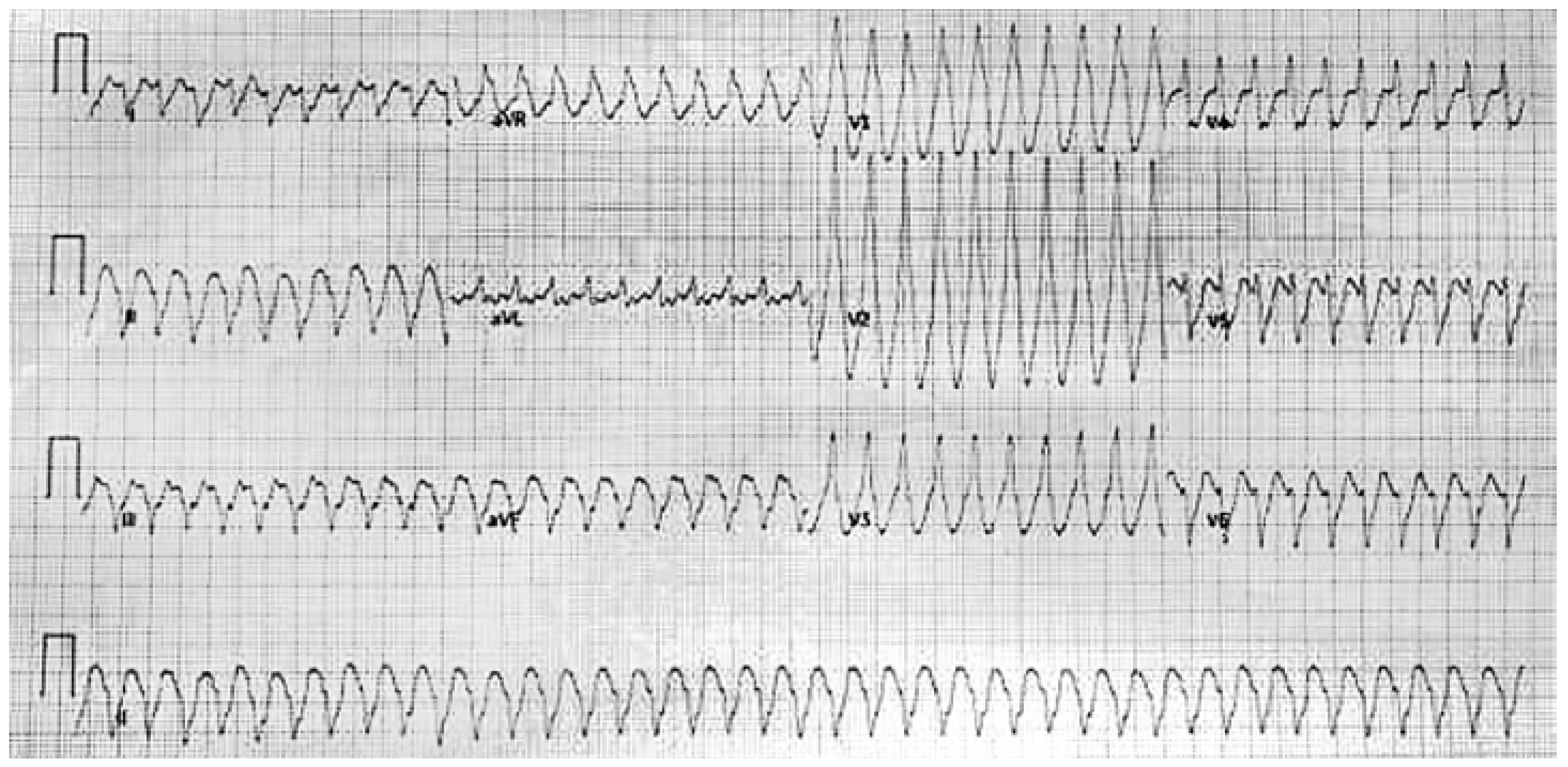
Case Presentation
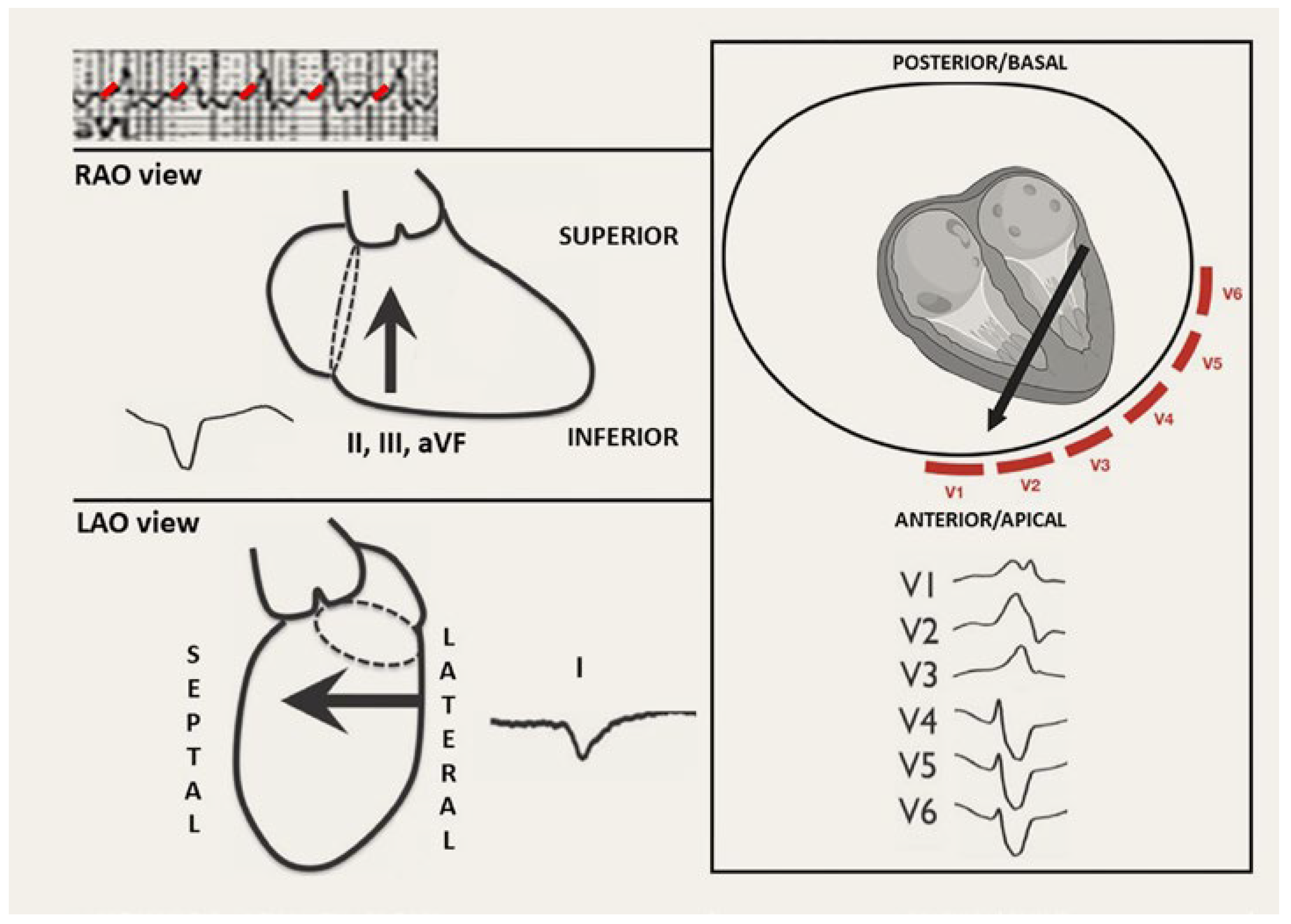
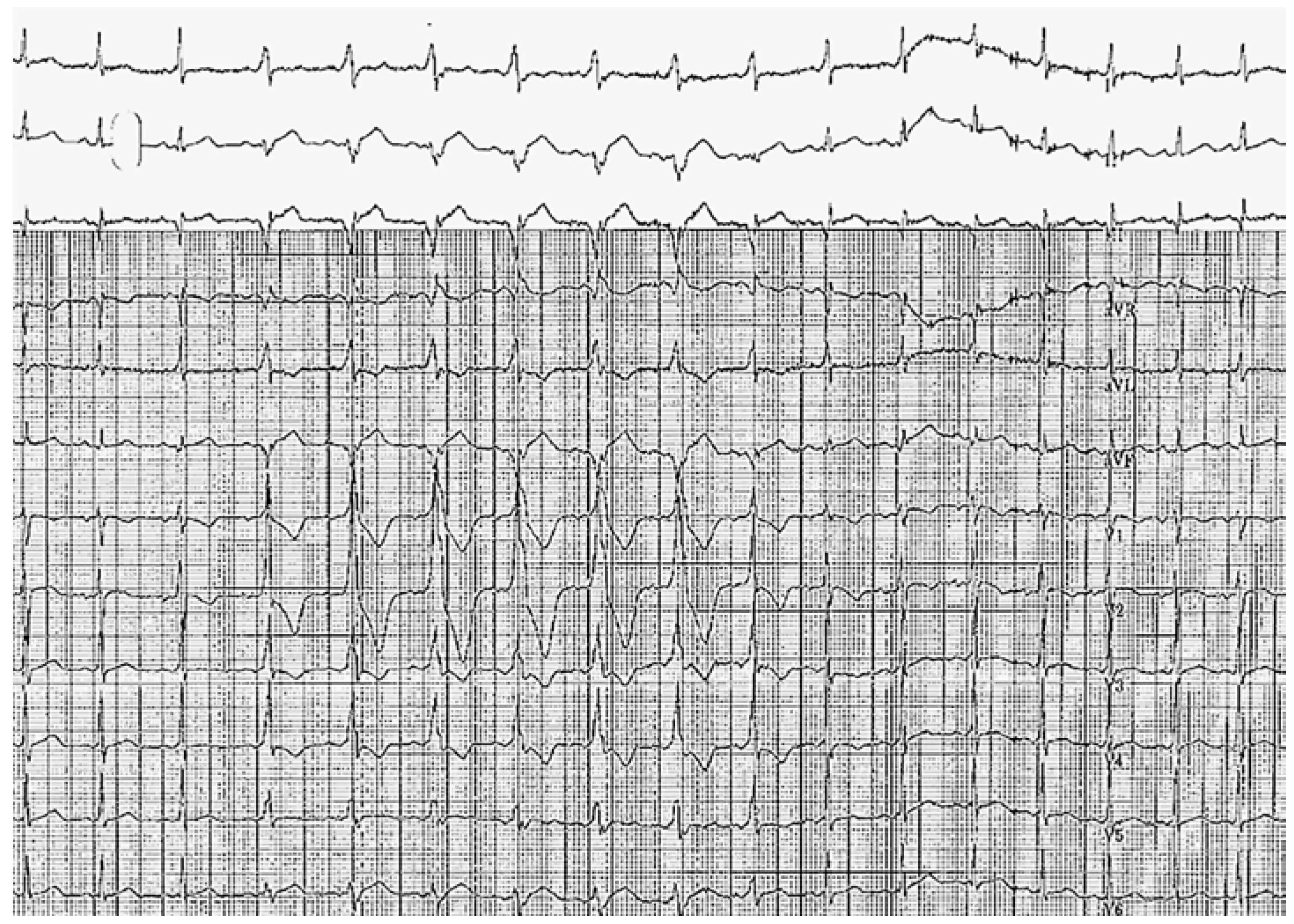
Discussion
Solution
Author Contributions
Informed Consent Statement
Acknowledgments
Conflicts of Interest
References
- Brugada, J.; Katritsis, D.G.; Arbelo, E.; Arribas, F.; Bax, J.J.; Blomström-Lundqvist, C.; ESC Scientific Document Group; et al. 2019 ESC Guidelines for the management of patients with supraventricular tachycardia—The Task Force for the management of patients with supraventricular tachycardia of the European Society of Cardiology (ESC). Eur. Heart J. 2020, 41, 655–720. [Google Scholar] [CrossRef] [PubMed]
- Silverman, A.J.; Machado, C.; Baga, J.J.; Meissner, M.D.; Lehmann, M.H.; Steinman, R.T. Adenosine-induced atrial fibrillation. Am. J. Emerg. Med. 1996, 14, 300–301. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, T.; Nagai, T.; Inoue, K.; Ikeda, S.; Yamaguchi, O. Adenosine triphosphate-induced life-threatening arrhythmia. J. Cardiol. Cases 2023, 28, 150–152. [Google Scholar] [CrossRef] [PubMed]
- Cosío, F.G.; Anderson, R.H.; Becker, A.; Borggrefe, M.; Campbell, R.W.; Gaita, F.; et al. Living anatomy of the atrioventricular junctions. A guide to electrophysiological mapping. A Consensus Statement from the Cardiac Nomenclature Study Group, Working Group of Arrythmias, European Society of Cardiology, and the Task Force on Cardiac Nomenclature from NASPE. North American Society of Pacing and Electrophysiology. Eur. Heart J. 1999, 20, 1068–1075. [Google Scholar] [PubMed]

© 2024 by the author. Attribution - Non-Commercial - NoDerivatives 4.0
Share and Cite
Vivekanantham, H.; Amit, G. A Wide Complex Tachycardia in a 31-Year-Old Male. Cardiovasc. Med. 2024, 27, 94. https://doi.org/10.4414/cvm.2024.1412183678
Vivekanantham H, Amit G. A Wide Complex Tachycardia in a 31-Year-Old Male. Cardiovascular Medicine. 2024; 27(3):94. https://doi.org/10.4414/cvm.2024.1412183678
Chicago/Turabian StyleVivekanantham, Hari, and Guy Amit. 2024. "A Wide Complex Tachycardia in a 31-Year-Old Male" Cardiovascular Medicine 27, no. 3: 94. https://doi.org/10.4414/cvm.2024.1412183678
APA StyleVivekanantham, H., & Amit, G. (2024). A Wide Complex Tachycardia in a 31-Year-Old Male. Cardiovascular Medicine, 27(3), 94. https://doi.org/10.4414/cvm.2024.1412183678



