Sex Differences in Type 2 Diabetes
Abstract
Introduction
Epidemiology
Obesity
Metabolic syndrome (MetS)
Sex-specific risk of gestational diabetes
Glucose homoeostasis
Hormones
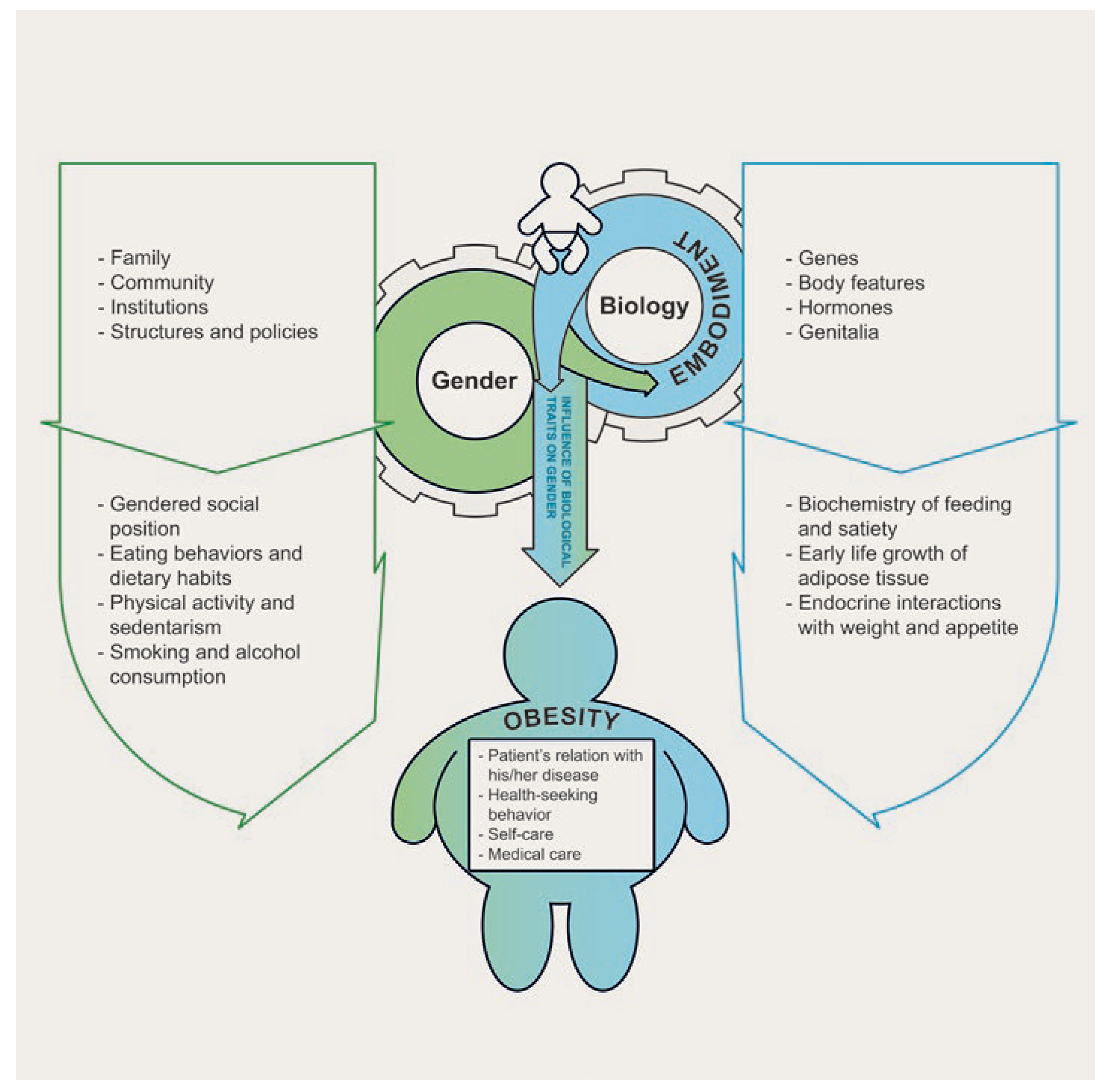
- Both sex, the biological differences between women and men, and gender, the sociologically constructed differences based on membership in one of the two sex categories, influence the prevalence of noncommunicable diseases such as obesity and type 2 diabetes (T2D).
- Many modifiable T2D risk factors are behavioural and greatly, but not only, influenced by gender-related determinants.
- There are differences in the prevalence of obesity and T2D between women and men that change during the lifespan.
- Pregnancy and menopause have a special impact with (abdominal) obesity and T2D increasing after the menopause.
- The link between obesity and T2D seems to be stronger in women than in men.
- Various hormones, such as sex hormones, but also cortisol, growth hormone and other hormones can impact glycaemic levels and body fat and their concentrations and effect on metabolic parameters can differ by sex.
Conclusion
Disclosure statement
References
- International Diabetes Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Kautzky-Willer, A.; Harreiter, J.; Pacini, G. Sex and Gender Differences in Risk, Pathophysiology and Complications of Type 2 Diabetes Mellitus. Endocr Rev. 2016, 37, 278–316. [Google Scholar] [CrossRef]
- Krieger, N. Genders, sexes, and health: what are the connections – and why does it matter? Int J Epidemiol. 2003, 32, 652–657. [Google Scholar] [CrossRef]
- Zhang, H.; Ni, J.; Yu, C.; Wu, Y.; Li, J.; Liu, J.; et al. Sex-Based Differences in Diabetes Prevalence and Risk Factors: A Population-Based Cross-Sectional Study Among Low-Income Adults in China. Front Endocrinol (Lausanne). 2019, 10, 658. [Google Scholar] [CrossRef]
- Choi, Y.J.; Kim, H.C.; Kim, H.M.; Park, S.W.; Kim, J.; Kim, D.J. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998–2005. Diabetes Care. 2009, 32, 2016–2020. [Google Scholar] [CrossRef]
- Boehme, M.W.; Buechele, G.; Frankenhauser-Mannuss, J.; Mueller, J.; Lump, D.; Boehm, B.O.; et al. Prevalence, incidence and concomitant co-morbidities of type 2 diabetes mellitus in South Western Germany – a retrospective cohort and case control study in claims data of a large statutory health insurance. BMC Public Health. 2015, 15, 855. [Google Scholar] [CrossRef]
- Lilja, M.; Eliasson, M.; Eriksson, M.; Söderberg, S. A rightward shift of the distribution of fasting and post-load glucose in northern Sweden between 1990 and 2009 and its predictors. Data from the Northern Sweden MONICA study. Diabet Med. 2013, 30, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Zhou, B.; Lu, Y.; Hajifathalian, K.; Bentham, J.; Di Cesare, M.; Danaei, G.; et al. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4·4 million participants. Lancet. 2016, 387, 1513–1530. [Google Scholar] [CrossRef] [PubMed]
- Agardh, E.; Allebeck, P.; Hallqvist, J.; Moradi, T.; Sidorchuk, A. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011, 40, 804–818. [Google Scholar] [CrossRef] [PubMed]
- Huebschmann, A.G.; Huxley, R.R.; Kohrt, W.M.; Zeitler, P.; Regensteiner, J.G.; Reusch, J.E. Sex differences in the burden of type 2 diabetes and cardiovascular risk across the life course. Diabetologia. 2019, 62, 1761–1772. [Google Scholar] [CrossRef]
- Magliano, D.J.; Islam, R.M.; Barr, E.L.; Gregg, E.W.; Pavkov, M.E.; Harding, J.L.; et al. Trends in incidence of total or type 2 diabetes: systematic review. BMJ. 2019, 366, 15003. [Google Scholar] [CrossRef]
- Cooper, A.J.; Gupta, S.R.; Moustafa, A.F.; Chao, A.M. Sex/Gender Differences in Obesity Prevalence, Comorbidities, and Treatment. Curr Obes Rep. 2021, 10, 458–466. [Google Scholar] [CrossRef]
- Federal Statistical Office (FSO). Swiss Health Survey 2017; Overweight and Obesity: Neuchâtel, 2020. [Google Scholar]
- Power, M.L.; Schulkin, J. Sex differences in fat storage, fat metabolism, and the health risks from obesity: possible evolutionary origins. Br J of Nutr. 2008, 99, 931–940. [Google Scholar] [CrossRef] [PubMed]
- Schorr, M.; Dichtel, L.E.; Gerweck, A.V.; Valera, R.D.; Torriani, M.; Miller, K.K.; et al. Sex differences in body composition and association with cardiometabolic risk. Biol Sex Differ. 2018, 9, 28. [Google Scholar] [CrossRef] [PubMed]
- Bray, G.A. Medical consequences of obesity. J Clin Endocrinol Metab. 2004, 89, 2583–2589. [Google Scholar] [CrossRef] [PubMed]
- Sattar, N. Gender aspects in type 2 diabetes mellitus and cardiometabolic risk. Best Pract Res Clin Endocrinol Metab. 2013, 27, 501–507. [Google Scholar] [CrossRef]
- Pasquali, R.; Vicennati, V.; Gambineri, A.; Pagotto, U. Sex-dependent role of glucocorticoids and androgens in the pathophysiology of human obesity. Int J Obes. 2008, 32, 1764–1779. [Google Scholar] [CrossRef]
- Nusrianto, R.; Tahapary, D.L.; Soewondo, P. Visceral adiposity index as a predictor for type 2 diabetes mellitus in Asian population: A systematic review. Diabetes Metab Syndr. 1231, 13, 1231–1235. [Google Scholar] [CrossRef]
- Lee, J.J.; Beretvas, S.N.; Freeland-Graves, J.H. Abdominal adiposity distribution in diabetic/prediabetic and nondiabetic populations: a meta-analysis. J Obes. 2014, 2014, 697264. [Google Scholar] [CrossRef]
- Shin, J.A.; Lee, J.H.; Lim, S.Y.; Ha, H.S.; Kwon, H.S.; Park, Y.M.; et al. Metabolic syndrome as a predictor of type 2 diabetes, and its clinical interpretations and usefulness. J Diabetes Investig. 2013, 4, 334–343. [Google Scholar] [CrossRef]
- O’Neill, S.; O’Driscoll, L. Metabolic syndrome: a closer look at the growing epidemic and its associated pathologies. Obes Rev. 2015, 16, 1–12. [Google Scholar] [CrossRef]
- Yadav, D.; Mahajan, S.; Subramanian, S.K.; Bisen, P.S.; Chung, C.H.; Prasad, G.B. Prevalence of metabolic syndrome in type 2 diabetes mellitus using NCEP-ATPIII, IDF and WHO definition and its agreement in Gwalior Chambal region of Central India. Glob J Health Sci. 2013, 5, 142–155. [Google Scholar] [CrossRef]
- Pradhan, A.D. Sex differences in the metabolic syndrome: implications for cardiovascular health in women. Clin Chem. 2014, 60, 44–52. [Google Scholar] [CrossRef]
- Nathan, D.M.; Davidson, M.B.; DeFronzo, R.A.; Heine, R.J.; Henry, R.R.; Pratley, R.; et al. American Diabetes Association. Impaired fasting glucose and impaired glucose tolerance: implications for care. Diabetes Care. 2007, 30, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Yan, H.; Yang, W.; Zhou, F.; Li, X.; Pan, Q.; Shen, Z.; et al. Estrogen Improves Insulin Sensitivity and Suppresses Gluconeogenesis via the Transcription Factor Foxo1. Diabetes. 2019, 68, 291–304. [Google Scholar] [CrossRef]
- Ding, E.L.; Song, Y.; Malik, V.S.; Liu, S. Sex differences of endogenous sex hormones and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA. 2006, 295, 1288–1299. [Google Scholar] [CrossRef]
- Plows, J.F.; Stanley, J.L.; Baker, P.N.; Reynolds, C.M.; Vickers, M.H. The Pathophysiology of Gestational Diabetes Mellitus. Int J Mol Sci. 2018, 19, 3342. [Google Scholar] [CrossRef] [PubMed]
- Kominiarek, M.A.; Peaceman, A.M. Gestational weight gain. Am J Obstet Gynecol. 2017, 217, 642–651. [Google Scholar] [CrossRef]
- Paulo, M.S.; Abdo, N.M.; Bettencourt-Silva, R.; Al-Rifai, R.H. Gestational Diabetes Mellitus in Europe: A Systematic Review and Meta-Analysis of Prevalence Studies. Front Endocrinol (Lausanne). 2021, 12, 691033. [Google Scholar] [CrossRef] [PubMed]
- Ryser Rüetschi, J.; Jornayvaz, F.R.; Rivest, R.; Huhn, E.A.; Irion, O.; Boulvain, M. Fasting glycaemia to simplify screening for gestational diabetes. BJOG. 2016, 123, 2219–2222. [Google Scholar] [CrossRef]
- Tramunt, B.; Smati, S.; Grandgeorge, N.; Lenfant, F.; Arnal, J.F.; Montagner, A.; et al. Sex differences in metabolic regulation and diabetes susceptibility. Diabetologia. 2020, 63, 453–461. [Google Scholar] [CrossRef]
- Tura, A.; Pacini, G.; Moro, E.; Vrbíková, J.; Bendlová, B.; Kautzky-Willer, A. Sex- and age-related differences of metabolic parameters in impaired glucose metabolism and type 2 diabetes compared to normal glucose tolerance. Diabetes Res Clin Pract. 2018, 146, 67–75. [Google Scholar] [CrossRef]
- Kautzky-Willer, A.; Brazzale, A.R.; Moro, E.; Vrbíková, J.; Bendlova, B.; Sbrignadello, S. , et al. Influence of increasing BMI on insulin sensitivity and secretion in normotolerant men and women of a wide age span. Obesity (Silver Spring). 2012, 20, 1966–1973. [Google Scholar] [CrossRef]
- Arnetz, L.; Ekberg, N.R.; Alvarsson, M. Sex differences in type 2 diabetes: focus on disease course and outcomes. Diabetes, Metab Syndr Obes. 2014, 7, 409–420. [Google Scholar] [CrossRef]
- Mattsson, C.; Olsson, T. Estrogens and glucocorticoid hormones in adipose tissue metabolism. Curr Med Chem. 2007, 14, 2918–2924. [Google Scholar] [CrossRef]
- Yao, Q.M.; Wang, B.; An, X.F.; Zhang, J.A.; Ding, L. Testosterone level and risk of type 2 diabetes in men: a systematic review and meta-analysis. Endocr Connect. 2018, 7, 220–231. [Google Scholar] [CrossRef] [PubMed]
- Rettberg, J.R.; Yao, J.; Brinton, R.D. Estrogen: A master regulator of bioenergetic systems in the brain and body. Front Neuroendocrinol. 2014, 35, 8–30. [Google Scholar] [CrossRef] [PubMed]
- Wake, D.J.; Strand, M.; Rask, E.; Westerbacka, J.; Livingstone, D.E.; Soderberg, S.; et al. Intra-adipose sex steroid metabolism and body fat distribution in idiopathic human obesity. Clin Endocrinol (Oxf). 2007, 66, 440–446. [Google Scholar] [CrossRef]
- Szalat, A.; Raz, I. Gender-specific care of diabetes mellitus: particular considerations in the management of diabetic women. Diabetes Obes Metab. 2008, 10, 1135–1156. [Google Scholar]
- Picard, F.; Wanatabe, M.; Schoonjans, K.; Lydon, J.; O’Malley, B.W.; Auwerx, J. Progesterone receptor knockout mice have an improved glucose homeostasis secondary to β-cell proliferation. Proc Natl Acad Sci USA. 2002, 99, 15644–15648. [Google Scholar] [CrossRef] [PubMed]
- Sitruk-Ware, R.; Nath, A. Characteristics and metabolic effects of estrogen and progestins contained in oral contraceptive pills. Best Prac Res Clin Endocrinol Metab. 2013, 27, 13–24. [Google Scholar] [CrossRef]
- Jensen, J.T. Evaluation of a new estradiol oral contraceptive: estradiol valerate and dienogest. Expert Opin Pharmacother. 2010, 11, 1147–1157. [Google Scholar] [CrossRef]
- Frystyk, J. Free insulin-like growth factors—measurements and relationships to growth hormone secretion and glucose homeostasis. Growth Horm IGF Res. 2004, 14, 337–375. [Google Scholar] [CrossRef]
- Gatford, K.L.; Egan, A.R.; Clarke, I.J.; Owens, P.C. Sexual dimorphism of the somatotrophic axis. J Endocrinol. 1998, 157, 373–389. [Google Scholar] [CrossRef]
- Meek, T.H.; Morton, G.J. The role of leptin in diabetes: metabolic effects. Diabetologia. 2016, 59, 928–932. [Google Scholar] [CrossRef] [PubMed]
- Thomas, T.; Burguera, B.; Melton LJ3rd Atkinson, E.J.; O’Fallon, W.M.; Riggs, B.L. , et al. Relationship of serum leptin levels with body composition and sex steroid and insulin levels in men and women. Metabolism. 2000, 49, 1278–1284. [Google Scholar] [CrossRef] [PubMed]
- Piemonti, L.; Calori, G.; Mercalli, A.; Lattuada, G.; Monti, P.; Garancini, M.P.; et al. Fasting plasma leptin, tumor necrosis factor-α receptor 2, and monocyte chemoattracting protein 1 concentration in a population of glucose-tolerant and glucose-intolerant women: impact on cardiovascular mortality. Diabetes Care. 2003, 26, 2883–2889. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Söderberg, S.; Stegmayr, B.; Stenlund, H.; Sjöström, L.G.; Agren, A.; Johansson, L.; et al. Leptin, but not adiponectin, predicts stroke in males. J Intern Med. 2004, 256, 128–136. [Google Scholar] [CrossRef]

© 2023 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Estoppey, P.; Clair, C.; Auderset, D.; Puder, J.J. Sex Differences in Type 2 Diabetes. Cardiovasc. Med. 2023, 26, 96. https://doi.org/10.4414/cvm.2023.02273
Estoppey P, Clair C, Auderset D, Puder JJ. Sex Differences in Type 2 Diabetes. Cardiovascular Medicine. 2023; 26(3):96. https://doi.org/10.4414/cvm.2023.02273
Chicago/Turabian StyleEstoppey, Paco, Carole Clair, Diane Auderset, and Jardena Jacqueline Puder. 2023. "Sex Differences in Type 2 Diabetes" Cardiovascular Medicine 26, no. 3: 96. https://doi.org/10.4414/cvm.2023.02273
APA StyleEstoppey, P., Clair, C., Auderset, D., & Puder, J. J. (2023). Sex Differences in Type 2 Diabetes. Cardiovascular Medicine, 26(3), 96. https://doi.org/10.4414/cvm.2023.02273



