Sinus Venosus Atrial Septal Defect with Partial Anomalous Pulmonary Vein Return †
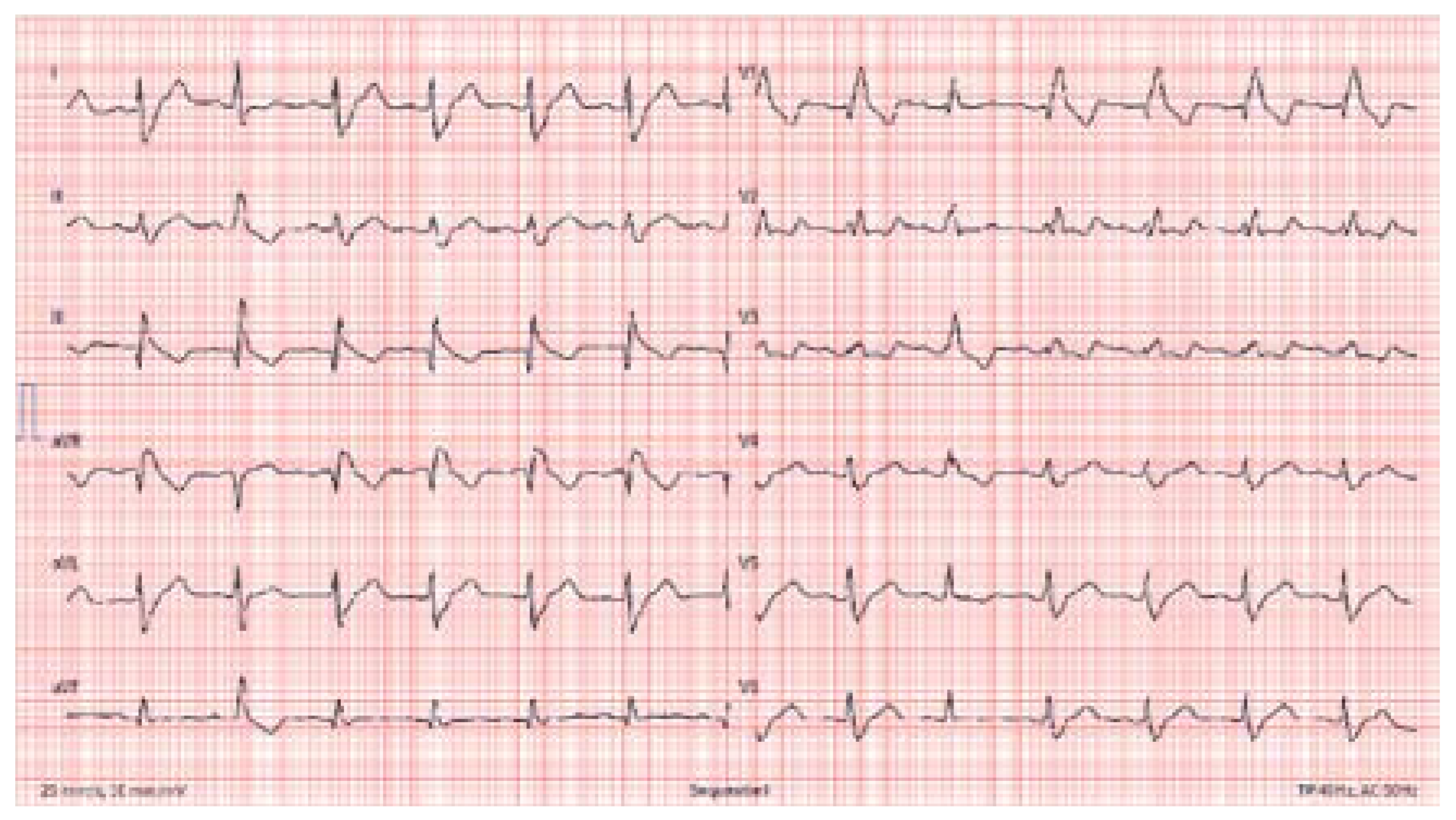
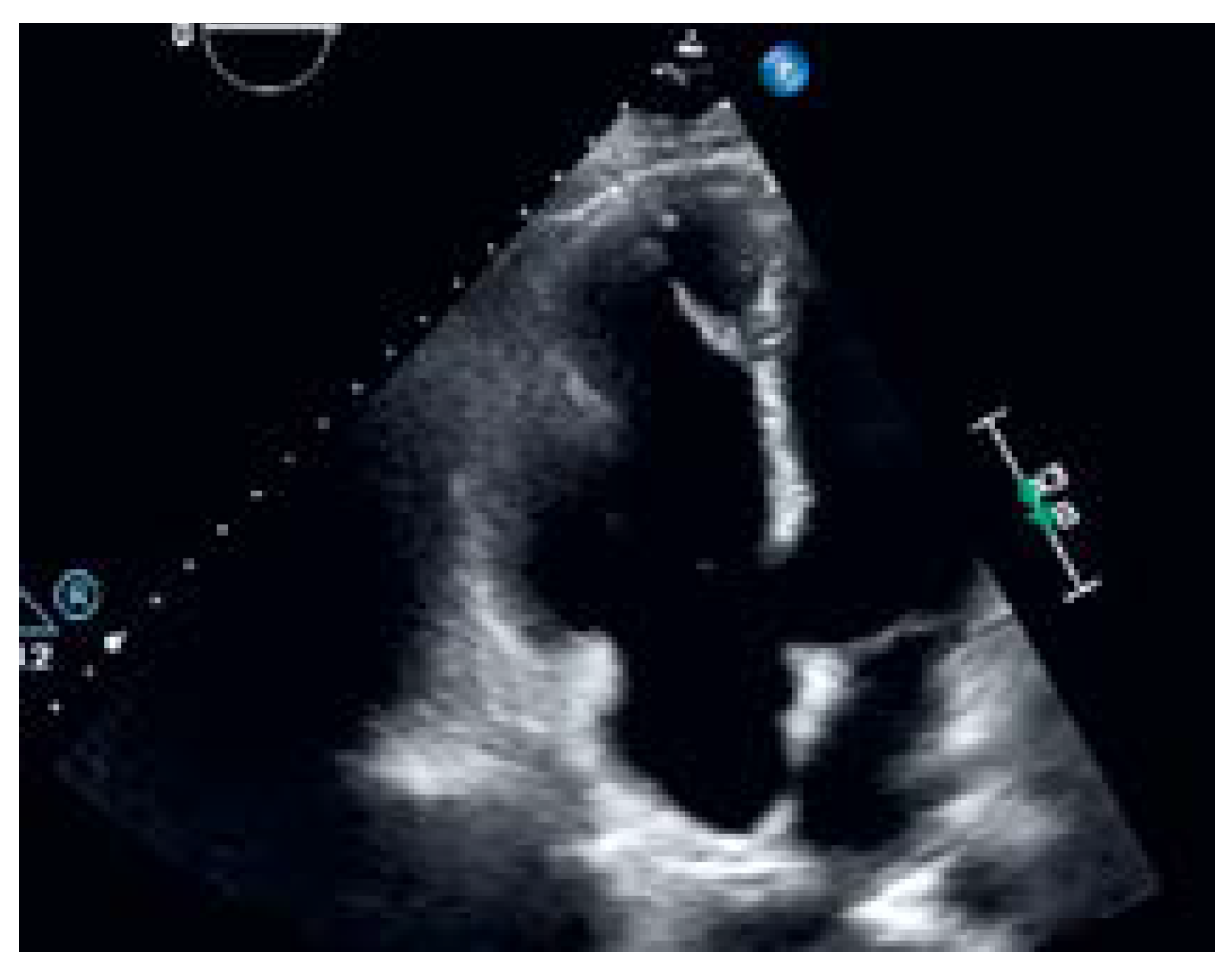
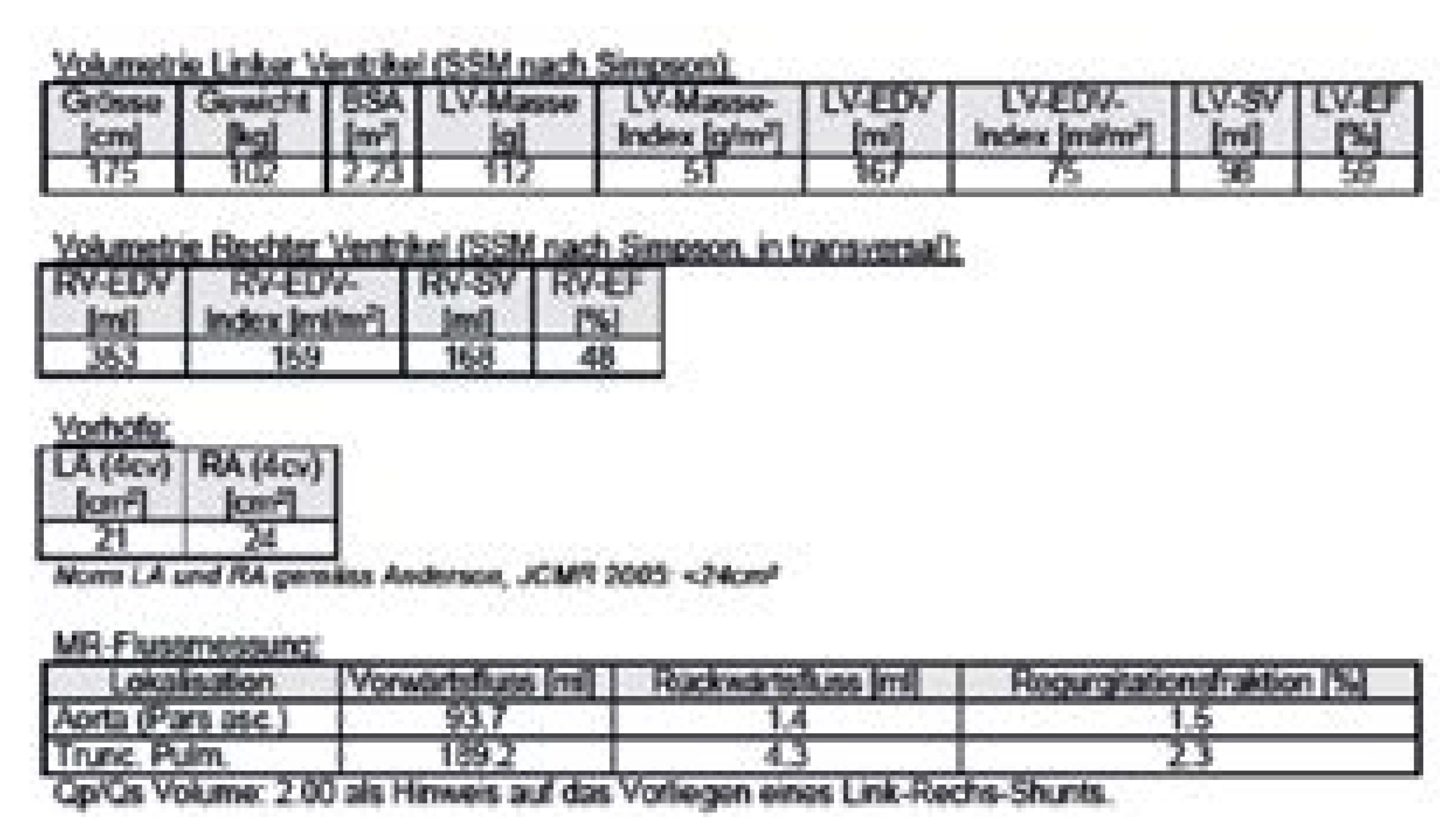
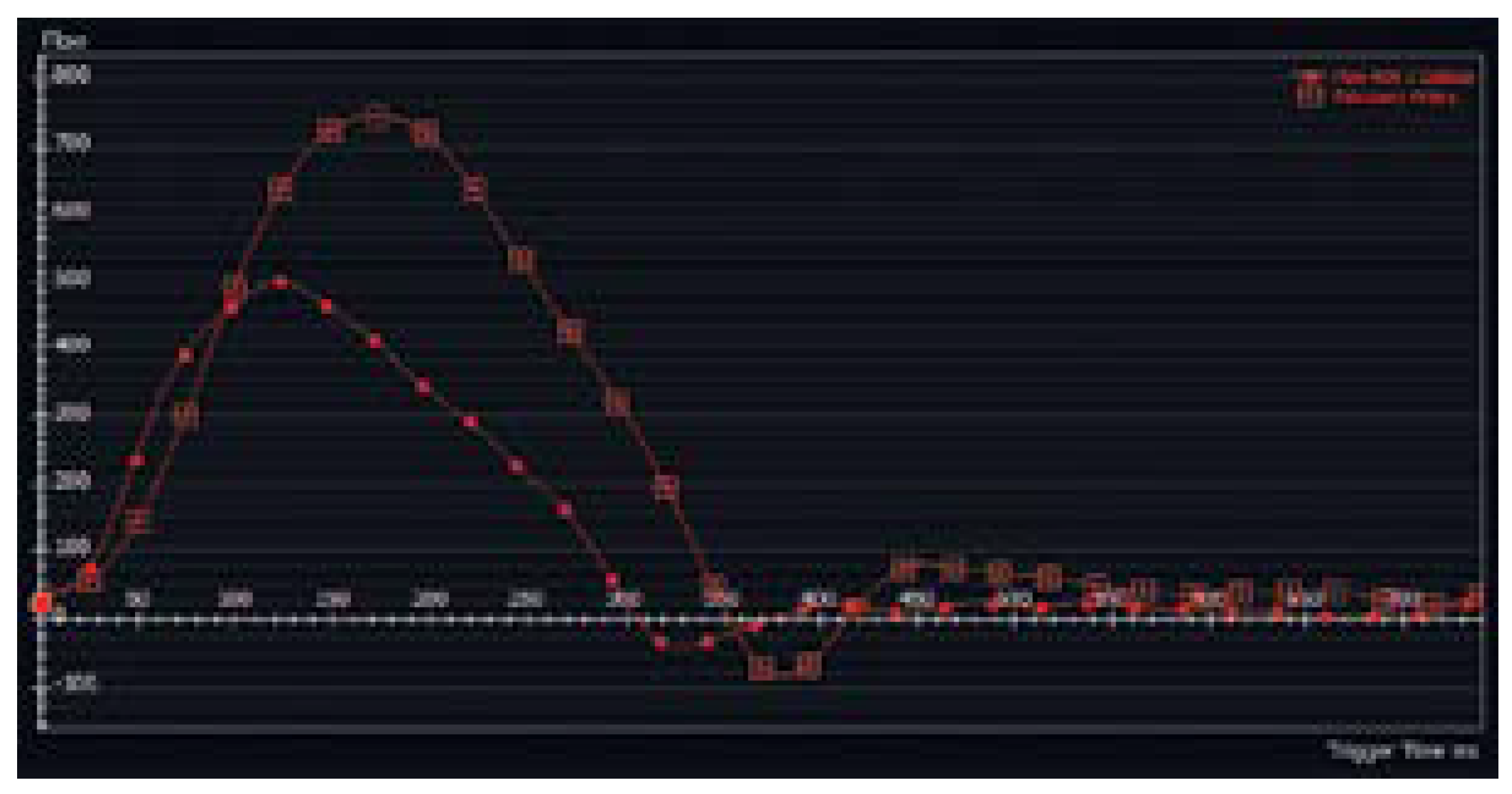
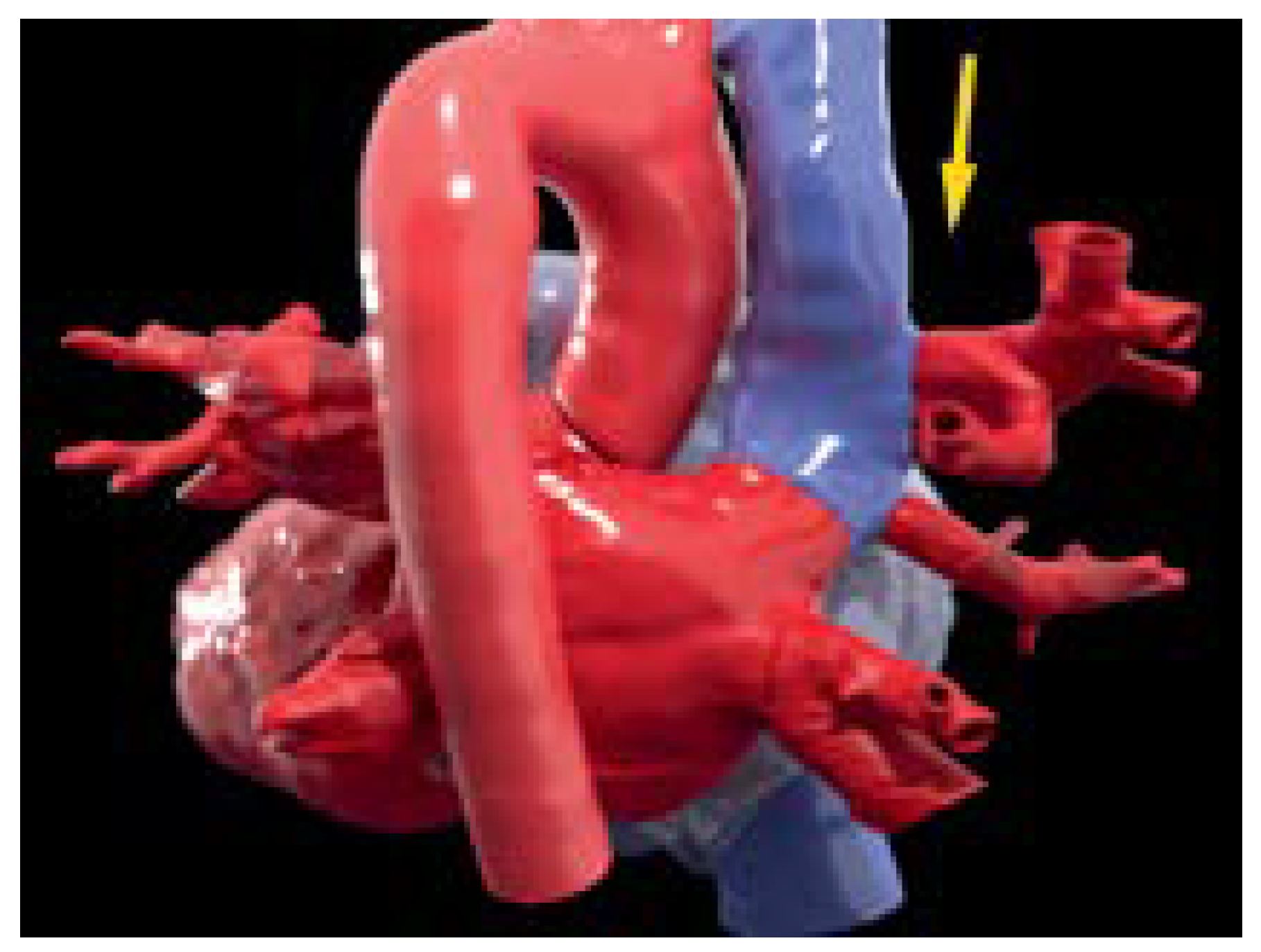
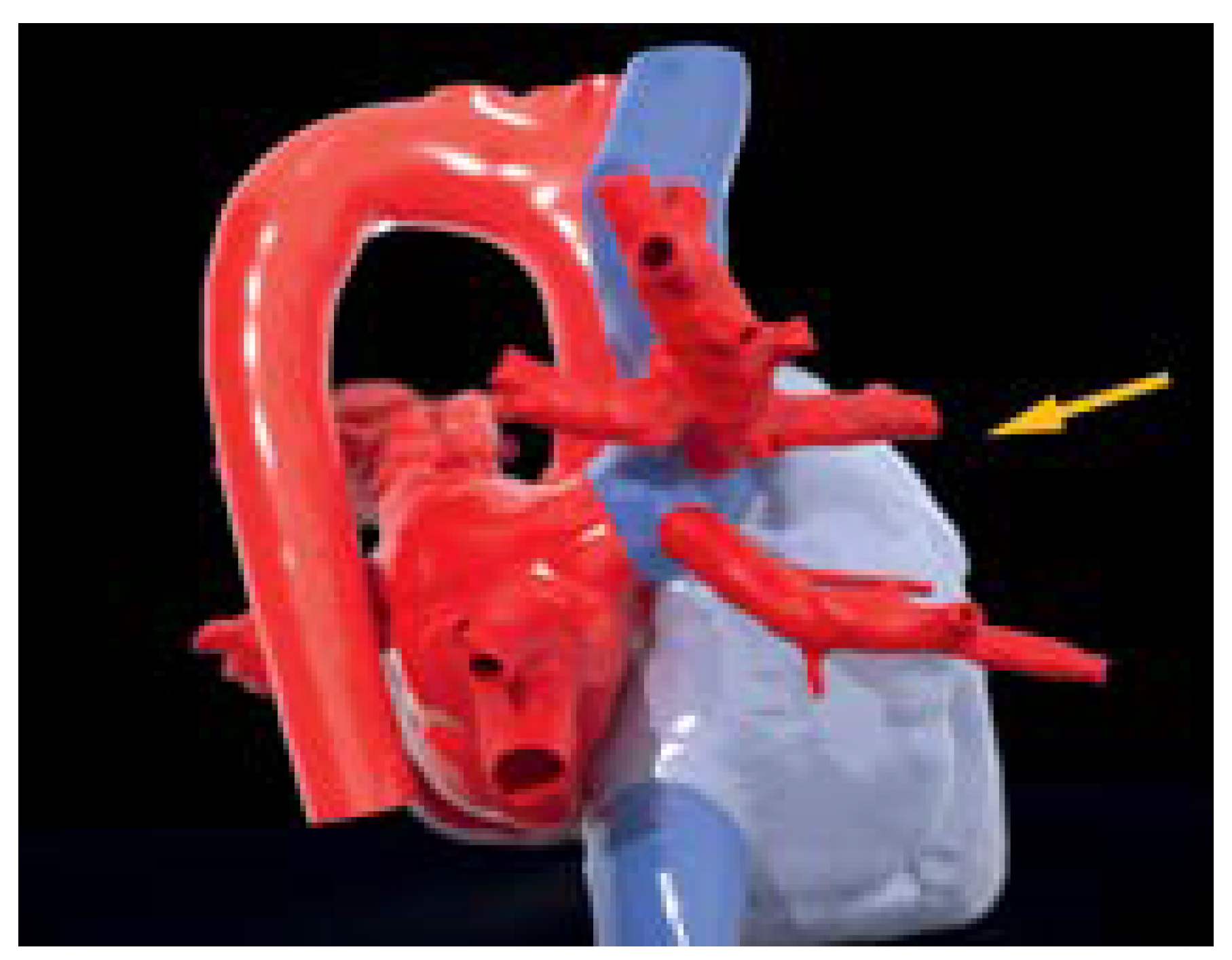
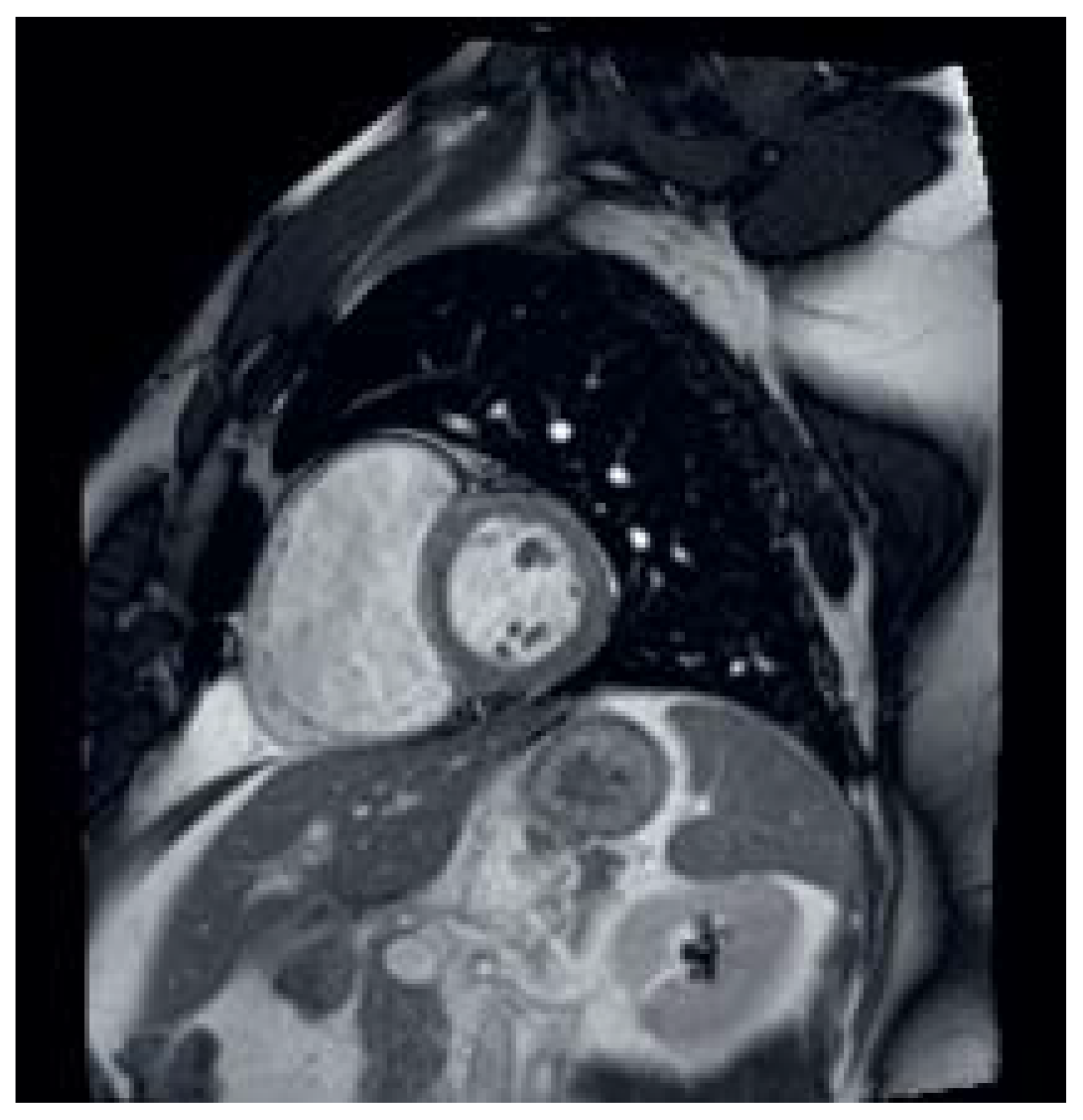
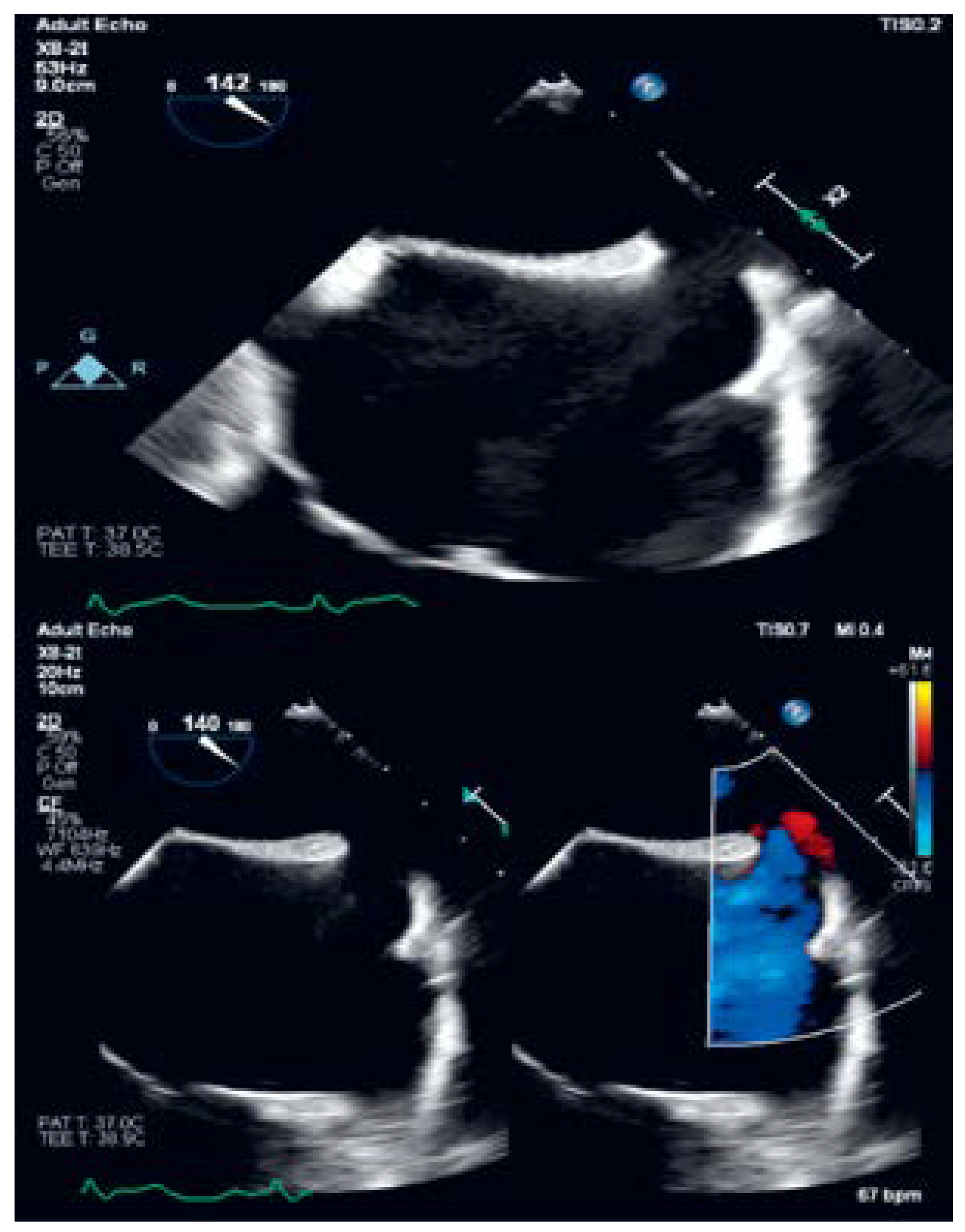
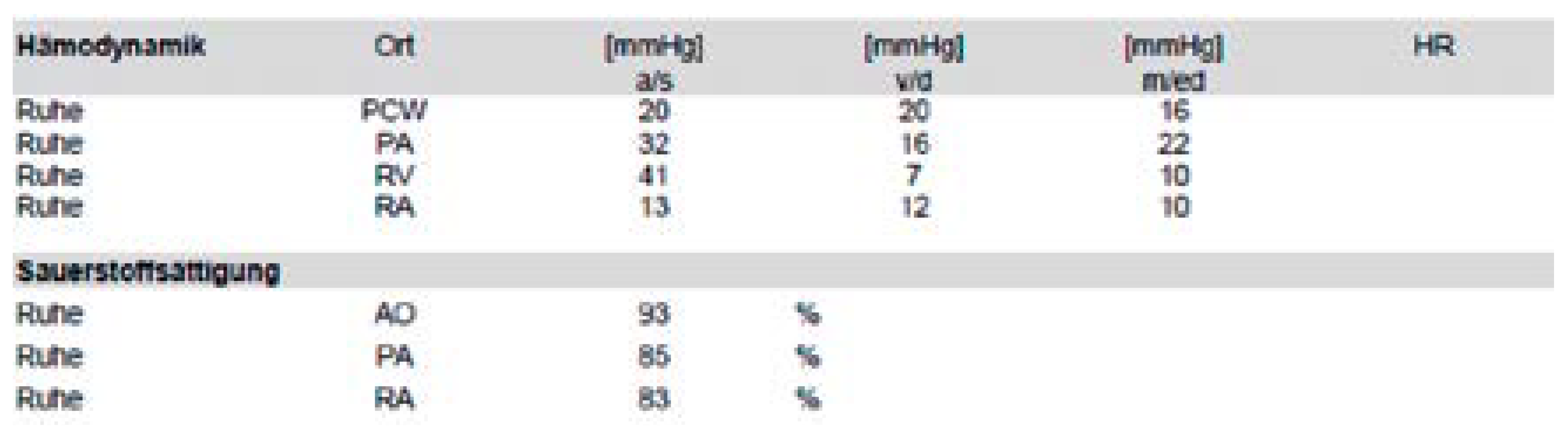
Case description
Discussion
Conflicts of Interest
References
- Baumgartner, H.; De Backer, J.; Babu-Narayan, S.V.; Budts, W.; Chessa, M.; Diller, G.P.; ESC Scientific Document Group; et al. 2020 ESC Guidelines for the management of adult congenital heart disease. Eur Heart J. 2021, 42, 563–645. [Google Scholar] [CrossRef] [PubMed]
- Pauwaa, S.; Farzaneh-Far, A. Isolated partial anomalous pulmonary venous return with intact atrial septum: A rare but treatable cause of pulmonary hypertension in adults. Eur Heart J Cardiovasc Imaging. 2014, 15, 830. [Google Scholar] [CrossRef] [PubMed]
- Winslow, J. Mem. Acad. Roy. d. Sc. Paris: 1739, 113.
- Hegde, M.; Manjunath, S.C.; Usha, M.K. Isolated Partial Anomalous Pulmonary Venous Connection: Development of Volume Overload and Elevated Estimated Pulmonary Pressure in Adults. J Clin Imaging Sci. 2019, 9, 29. [Google Scholar] [CrossRef] [PubMed]
- Pizzini, A.; Sonnweber, T.; Frank, R.; Theurl, M.; Weiss, G.; Tancevski, I.; et al. Clinical implications of partial anomalous pulmonary venous connection: A rare cause of severe pulmonary arterial hypertension. Pulm Circ. 2020, 10, 2045894019885352. [Google Scholar] [CrossRef] [PubMed]
- Gaynor, J.W.; Weinberg, P.M.; Spray, T.L. Congenital Heart Surgery Nomenclature and Database Project: Systemic venous anomalies. Ann Thorac Surg. 2000, 69 (Suppl. 4), S70–S76. [Google Scholar] [CrossRef] [PubMed]
- Stephen, L.; Shalini, W.; Eleanor, N.S.; Helen, M.; Michael, Y.; Mark, H. Anomalous pulmonary vein drainage: A pictorial essay with a CT focus. J. Congenit. Cardiol. 2017, 1, 1–13. [Google Scholar] [CrossRef]

© 2022 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Wojtal, R.; Spirig, A.; Ohletz, T.; Haegeli, L.M.; Fuchs, T.A. Sinus Venosus Atrial Septal Defect with Partial Anomalous Pulmonary Vein Return. Cardiovasc. Med. 2022, 25, 124. https://doi.org/10.4414/cvm.2022.02215
Wojtal R, Spirig A, Ohletz T, Haegeli LM, Fuchs TA. Sinus Venosus Atrial Septal Defect with Partial Anomalous Pulmonary Vein Return. Cardiovascular Medicine. 2022; 25(4):124. https://doi.org/10.4414/cvm.2022.02215
Chicago/Turabian StyleWojtal, Renata, Andres Spirig, Tim Ohletz, Laurent M. Haegeli, and Tobias A. Fuchs. 2022. "Sinus Venosus Atrial Septal Defect with Partial Anomalous Pulmonary Vein Return" Cardiovascular Medicine 25, no. 4: 124. https://doi.org/10.4414/cvm.2022.02215
APA StyleWojtal, R., Spirig, A., Ohletz, T., Haegeli, L. M., & Fuchs, T. A. (2022). Sinus Venosus Atrial Septal Defect with Partial Anomalous Pulmonary Vein Return. Cardiovascular Medicine, 25(4), 124. https://doi.org/10.4414/cvm.2022.02215



