EMPEROR Preserve and What It Means
Heart failure? What heart failure?
The surprising diabetic drugs
What is HFpEF?
EMPEROR Preserved: an important step forward
Modern heart failure management
Potential competing interests
References
- Withering, W. An Account of the Foxglove and of its medical uses: with practical remarks on dropsy and other diseases. Londen, 1785. [Google Scholar]
- McDonagh, T.A.; Metra, M.; Adamo, M.; Gardner, R.S.; Baumbach, A.; Böhm, M.; et al.; ESC Scientific Document Group 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021, 42, 3599–3726. [Google Scholar] [CrossRef]
- Digitalis Investigation Group. The effect of digoxin on mortality and morbidity in patients with heart failure. N Engl J Med. 1997, 336, 525–533. [Google Scholar] [CrossRef] [PubMed]
- Swedberg, K.; Held, P.; Kjekshus, J.; Rasmussen, K.; Rydén, L.; Wedel, H. Effects of the early administration of enalapril on mortality in patients with acute myocardial infarction. Results of the Cooperative New Scandinavian Enalapril Survival Study II (CONSENSUS II). N Engl J Med. 1992, 327, 678–684. [Google Scholar] [CrossRef] [PubMed]
- Swedberg, K.; Kjekshus, J.; Snapinn, S. Long-term survival in severe heart failure in patients treated with enalapril. Ten year follow-up of CONSENSUS I. Eur Heart J. 1999, 20, 136–139. [Google Scholar] [CrossRef] [PubMed]
- Chisholm, S.A.; Neal, T.J.; Alawattegama, A.B.; Birley, H.D.; Howe, R.A.; Ison, C.A. Emergence of high-level azithromycin resistance in Neisseria gonorrhoeae in England and Wales. J Antimicrob Chemother. 2009, 64, 353–358. [Google Scholar] [CrossRef]
- Packer, M.; Coats, A.J.; Fowler, M.B.; Katus, H.A.; Krum, H.; Mohacsi, P.; et al.; Carvedilol Prospective Randomized Cumulative Survival Study Group Effect of carvedilol on survival in severe chronic heart failure. N Engl J Med. 2001, 344, 1651–1658. [Google Scholar] [CrossRef]
- Effect of metoprolol CR/XL in chronic heart failure: Metoprolol CR/XL Randomised Intervention Trial in Congestive Heart Failure (MERITHF). Lancet. 1999, 353, 2001–2007. [CrossRef]
- Pitt, B.; Zannad, F.; Remme, W.J.; Cody, R.; Castaigne, A.; Perez, A.; et al.; Randomized Aldactone Evaluation Study Investigators The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999, 341, 709–717. [Google Scholar] [CrossRef]
- Zannad, F.; McMurray, J.J.; Krum, H.; van Veldhuisen, D.J.; Swedberg, K.; Shi, H.; et al.; EMPHASIS-HF Study Group Eplerenone in patients with systolic heart failure and mild symptoms. N Engl J Med. 2011, 364, 11–21. [Google Scholar] [CrossRef]
- McMurray, J.J.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; et al.; PARADIGM-HF Investigators and Committees Angiotensin-neprilysin inhibition versus enalapril in heart failure. N Engl J Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.; Coats, A.J.; et al.; ESC Scientific Document Group 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef]
- Solomon, S.D.; Claggett, B.; Lewis, E.F.; Desai, A.; Anand, I.; Sweitzer, N.K.; et al.; TOPCAT Investigators Influence of ejection fraction on outcomes and efficacy of spironolactone in patients with heart failure with preserved ejection fraction. Eur Heart J. 2016, 37, 455–462. [Google Scholar] [CrossRef]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; et al.; EMPA-REG OUTCOME Investigators Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N Engl J Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef]
- Clark, B.C.; Arnold, W.D. Strategies to Prevent Serious Fall Injuries: A Commentary on Bhasin et al. A Randomized Trial of a Multifactorial Strategy to Prevent Serious Fall Injuries. N Engl J Med. 2020;383(2):129-140. Adv Geriatr Med Res 2021, 3. [Google Scholar]
- McMurray, J.J.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; et al.; DAPA-HF Trial Committees and Investigators Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N Engl J Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef]
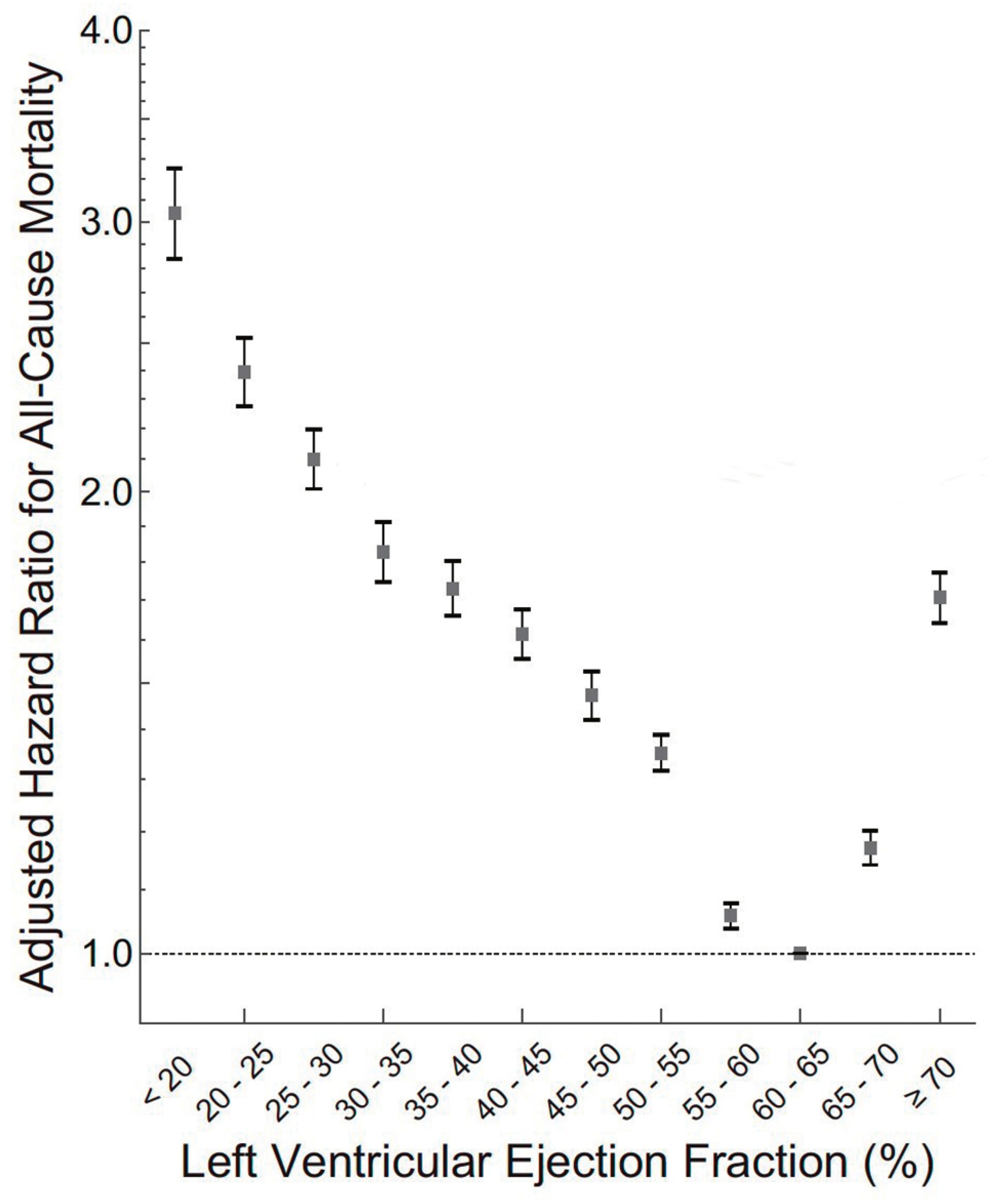
- Wehner, G.J.; Jing, L.; Haggerty, C.M.; Suever, J.D.; Leader, J.B.; Hartzel, D.N.; et al. Routinely reported ejection fraction and mortality in clinical practice: where does the nadir of risk lie? Eur Heart J. 2020, 41, 1249–1257. [Google Scholar] [CrossRef] [PubMed]
- Elliott, P.M.; Anastasakis, A.; Borger, M.A.; Borggrefe, M.; Cecchi, F.; Charron, P.; et al.; Authors/Task Force members 2014 ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014, 35, 2733–2779. [Google Scholar] [CrossRef] [PubMed]
- Williams, B.; Mancia, G.; Spiering, W.; Agabiti Rosei, E.; Azizi, M.; Burnier, M.; et al.; ESC Scientific Document Group 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018, 39, 3021–3104. [Google Scholar] [CrossRef] [PubMed]
- Maurer, M.S.; Schwartz, J.H.; Gundapaneni, B.; Elliott, P.M.; Merlini, G.; Waddington-Cruz, M.; et al.; ATTR-ACT Study Investigators Tafamidis Treatment for Patients with Transthyretin Amyloid Cardiomyopathy. N Engl J Med. 2018, 379, 1007–1016. [Google Scholar] [CrossRef]
- Adams, D.; Gonzalez-Duarte, A.; O’Riordan, W.D.; Yang, C.C.; Ueda, M.; Kristen, A.V.; et al. Patisiran, an RNAi Therapeutic, for Hereditary Transthyretin Amyloidosis. N Engl J Med. 2018, 379, 11–21. [Google Scholar] [CrossRef]
- Anker, S.D.; Butler, J.; Filippatos, G.; Ferreira, J.P.; Bocchi, E.; Böhm, M.; et al.; EMPEROR-Preserved Trial Investigators Empagliflozin in Heart Failure with a Preserved Ejection Fraction. N Engl J Med. 2021, 385, 1451–1461. [Google Scholar] [CrossRef]




 |
© 2021 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Lüscher, T.F. EMPEROR Preserve and What It Means. Cardiovasc. Med. 2021, 24, w10110. https://doi.org/10.4414/cvm.2021.02186
Lüscher TF. EMPEROR Preserve and What It Means. Cardiovascular Medicine. 2021; 24(6):w10110. https://doi.org/10.4414/cvm.2021.02186
Chicago/Turabian StyleLüscher, Thomas F. 2021. "EMPEROR Preserve and What It Means" Cardiovascular Medicine 24, no. 6: w10110. https://doi.org/10.4414/cvm.2021.02186
APA StyleLüscher, T. F. (2021). EMPEROR Preserve and What It Means. Cardiovascular Medicine, 24(6), w10110. https://doi.org/10.4414/cvm.2021.02186




