Abstract
As a result of advances in therapy many people living with heart failure reach both an advanced age and advanced stages of disease. This means, however, that they suffer symptoms and problems that may require an additional layer of care in order for them to be addressed. Involving elements of palliative care and, less frequently specialised palliative care or palliative care teams, can significantly limit the burden of symptoms and give patients and their relatives support in coping with challenging situations. Acknowledging the changing nature of palliative care, – as care appropriate for people living with serious diseases (and not only cancer) at every stage of the disease progression (and not only those of the dying) – can help to set up cooperation between cardiology and palliative care. The focus of modern palliative care, as of modern cardiology, is therefore similar – on saving life in the best possible quality. Screening for unaddressed needs could lead to a standard involvement of palliative care when needed. Palliative care reinforces a holistic understanding of a human being (going beyond seeing an ill “person” just in a patient’s role) and addresses the totality of the individual, respecting their relational existence according to the biopsychosocial-spiritual model. These unaddressed needs of people living with a disease and their families can lie in the physical, psychological, social and spiritual dimensions. Symptom control, support in all these dimensions, aiding in decision making, organising a network of care and, finally, as the person approaches the end of her or his life, care for the dying, can all enrich the quality of life of people living with the disease and their relatives. Support for the family is extended beyond the death of the loved ones in the form of bereavement counselling. Cooperation between cardiology and all other disciplines including palliative care should bear the hallmarks of care in the 21st century: caring for all dimensions of needs, always when they emerge and involving all disciplines needed.
Introduction
Progress in medical and device therapy has improved the survival of people affected by heart failure. Guideline-directed medical therapy improves quality of life, symptom burden and survival. Antitachyarrhythmic interventions with use of implantable cardioverters defibrillators and cardiac resynchronisation therapy with an implantable cardioverters defibrillator function (collectively cardiac implantable electronic devices [CIEDs]) decrease mortality by improving left ventricular function and preventing sudden cardiac death respectively [1]. As a consequence, people with heart failure live longer, reaching more advanced stages of the disease and more advanced age, when heart failure symptoms and comorbidities contribute markedly to limitation in the quality of life.
The population of people living with heart failure can be divided into two subgroups. First, those usually treated in specialised cardiology centres, i.e. younger people who commonly undergo coronary and valve interventions and CIED implantation. In this group, in the case of disease progression, heart transplantation or implantation of mechanical circulatory support can be considered as a treatment option. The second group, which is older and much larger, is usually treated by general practitioners and is often hospitalised in general internal disease departments in the case of acute decompensation of their heart failure. This group is often not seen in specialised cardiology centres on a regular basis. People from this group suffer and die more frequently from concomitant disease [2]. The symptom burden and need for medical support differ substantially between these subpopulations. For some proportion of people from both groups, the provision of palliative care could substantially improve their quality of life when added to optimal cardiological care [3,4,5,6].
Concept of palliative care
The vison of palliative care has changed substantially in the last few years. It is now defined as active, comprehensive care dedicated to improving the quality of life of people affected by a disease that causes a burden that cannot be improved by optimising disease specific (curative) treatment alone [7]. Quality of life refers to wellbeing and satisfaction in all domains of a human’s life, and includes physical, emotional, social and spiritual issues. Spirituality is probably the most underestimated domain in care for people with cardiovascular disease. It reflects, however, the way a person seeks and expresses the meaning and purpose of their own life, and the way they experience their connectedness to the moment, to themselves, to others, to nature and to the significant or sacred. Spirituality goes far beyond religiosity and should not have been overlooked in modern medicine, especially in countries like Switzerland, where a growing proportion of especially younger people describe themselves as not religious [8]. The current definition of palliative care no longer defines the risk of death as the main factor qualifying one for palliative care provision. This significant change in the scope of palliative care has barely been acknowledged by both the community and non-palliative care medical professionals. The misconception of palliative care is still the biggest barrier in improving its provision to those who have needs that could be addressed by implementing palliative care interventions.
The majority of publications on palliative care for people living with heart failure have tried to define the relevant prognostic criteria for triggering contact with palliative care [9]. This approach has failed and is responsible for the current situation, where only a small proportion of patients with heart failure receive palliative care for a much shorter period than people with oncological disease. Currently, palliative care should be provided for all people who have the need, irrespective of prognosis or planned treatment. To date, the only accessible tool (Needs Assessment Tool: Progressive Disease – Heart Failure, NAT: PD-HF) helping to identify needs among people living with heart failure aims to consider four domains that can be addressed by palliative care provision: (1) high probability for need of palliative care provision (lack of informal caregivers, patient or caregivers request for palliative care or caring-core team needing support in managing the care); (2) patient wellbeing (symptom burden, psychological, emotional or existential issues, need for intensified communication); (3) the ability of an informal caregiver to provide care; and (4) caregiver wellbeing. The NAT: PD-HF can be completed by any health professional. The fifth domain contains prompts helping this person to consider what actions, and what type and level of care are needed to cover the recognised needs [10,11]. The NAT: PD-HF form is accessible online [12]. The intensity of palliative care interventions can vary according to changes in needs, including stopping it if the condition improves or needs have been addressed successfully.
The experts who developed the European Association for Palliative Care (EAPC) position statement suggest three types of situations that should trigger assessment of needs. These are: (1) significant changes in heart failure trajectory; (2) periodic heart failure visit or essential changes in health status; and (3) patient/family related factors [13]. These triggers and a flow chart suggesting how to proceed after needs have been assessed are summarised in Figure 1.
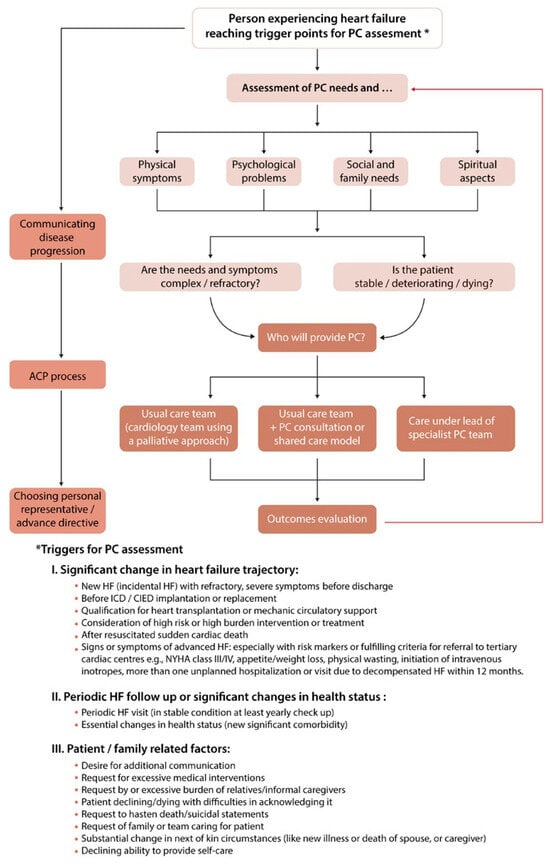
Figure 1.
Provision of palliative care for people living with heart failure flow chart and triggers for needs assessment. Reprinted from [13] by permission the Oxford University Press.
SENSE model of palliative care
The SENSE model, developed in Switzerland, describes the core components of palliative care. They are Symptom assessment and management, dEcision making, Networking, Support and End-of-life care [14]. This model stresses that palliative care is neither exclusively care for the dying nor for symptom management. The term support refers to several important “non-physical” domains – emotional, existential and spiritual – that especially if palliative care is provided in acute inpatient units (such as cardiology wards or intensive care units) remain unnoticed. Addressing symptoms, especially if they are severe, is of high urgency; however, it does not complete the scope of palliative care, but merely opens a space for interventions addressing highly meaningful needs(such as psychosocial, existential and spiritual issues). The components of needs change dynamically, usually parallel to changes in the life/disease trajectory [15]. Of all palliative care elements, only those that are needed and wished for should be implemented, as soon as possible after the emerging needs have been recognised. If palliative care is considered as support at the end of life only, it should be stated that nowadays the end-of-life period is defined as much longer than in the past. End-of-life refers now to a period of inevitable disease progression, one that cannot be arrested by the optimisation of disease-specific treatment and leads to natural death. The end-of-life period can last weeks to months and differs from imminent or active dying (lasting hours to days). This means that end-of-life care should not be postponed until the very last moments of life.
Elements of palliative care in heart failure
The most common symptoms reported by people living with heart failure are breathlessness, pain (quite often a consequence of concomitant disease), depression or anxiety [5,16]. The principles of medical treatment are discussed in the EAPC position paper [13]. In brief, getting skilled in prescribing opioids can be an important aid for healthcare professionals treating people with heart failure to improve management of pain and potentially breathlessness as well. Impairment of renal function, quite common among people with advanced heart failure, should be considered when choosing the most suitable opioid. Substances with active, potentially toxic metabolites with renal excretion, such morphine or oxycodone, should be avoided when glomerular filtration rate is below 30 ml/min/1.73 m2 [13,17].
One of the key elements of palliative care is support in decision making, especially decisions having potential consequences on life trajectory, including the trajectory of dying [18]. The communication on future health should include a discussion of risks and the expected mode of decline or the care the patient wishes to receive when death will become inevitable. This communication can be structured in the form of advance care planning [19]. The conclusions can (should) be documented in written form, for example as advance directives or an advance statement (in Switzerland “Patientenverfügung”). Another outcome of advance care planning would be the nomination of personal representatives for medical decision making, in the event of any loss of decision-making capacity by the patient her- or him-self. This communication needs compassionate sincerity without avoiding such topics as approaching death and dying or resigning from medical interventions (especially if the ill person considers the prolongation of life to be too burdensome) [20]. Medical professionals working in cardiology may feel uncomfortable discussing those topics. Some patients, especially those who are elderly, do not wish to discuss topics related to decline and dying in advance, and this has to be acknowledged and respected [21].
When death is approaching, adjusting treatment goals is desirable and should be aimed at the avoidance of side effects and limiting medicines to those assuring benefits for quality of life. Drugs improving prognosis with a long waiting time (e.g., statins) can be considered as inappropriate and probably be stopped. Drugs that influence the function of the circulatory system (like angiotensin converting enzyme inhibitors, angiotensin receptor blockers, angiotensin receptor neprilysin inhibitors, beta-blockers or diuretics) can be of significance for symptom management and should not be discontinued if they do not cause significant side effects. The dose regimen should, however, be evaluated and modified as needed. Some new drugs may be needed to improve symptom management, even for a short time, during active dying. Unnecessary blood tests or monitoring should be avoided in this phase [13].
Modification of CIED activity should be discussed in advance much earlier than when the person is entering the end-of-life or dying phase and performed in an agreed situation. The information about the option to stop some functions that can cause suffering whilst dying should be provided, according to the recommendations of different cardiological societies, in a sensitive way before CIED implantation [22]. Not all functions of CIED should be suspended, but only those causing potential harm or suffering or prolongation of the dying (defibrillation or cardioversion). If the goal of device activity modification is to allow a natural death without postponing it, deactivation of all antitachycardia functions may be appropriate. Antibradycardia pacing and resynchronisation therapy can prevent heart failure symptoms even in the last hours or days of life without prolonging dying. Thus, keeping these active should be seen as appropriate for maintaining quality of life during dying [23,24,25].
Implementation of palliative care in heart failure
The structures of care needed to provide optimal care for people living with heart failure have still not been defined. Palliative care can be delivered as a palliative care approach (the so-called generic or primary palliative care). This kind of care is delivered by all health care professionals incorporating the principles of palliative care (described in Table 1) in the care they usually provide. Specialist palliative care is delivered by professionals having specialist training and skills. Patients usually prefer to start receiving palliative care early in their disease trajectory and to stay under the care of a core cardiological team, one that is used to having cared for her or him for a longer time. Additionally, providing continuously optimised cardiological guideline-directed medical therapy is crucial, even in the case of very advanced disease. Based on these facts, it can be hypothesised that the optimal model of care should be the integration of palliative care into usual cardiac care. It can be implemented by strengthening basic palliative care skills among healthcare professionals working in cardiology and by establishing close cooperation with a palliative care team or at least a palliative care consultant. A survey of British medical staff working in cardiology revealed a lack of confidence in prescribing opioids (for pain and breathlessness management) and in challenging communication on issues related to disease progression and anticipated decline. According to local needs and traditions, a palliative care consultant/team can have a fixed position within the heart team, be a part of the hospital palliative care team or work as liaison palliative care, making connections between the cardio team and an external palliative care team. Cooperation between palliative care and cardiology is rather about patient-centred care provided based on the integration of services and not on transferring patients to (specialised) hospices. Referral to hospices is probably needed only for those with complex problems and needs and with a prolonged period of decline. This kind of care could be more commonly used for people living with heart failure in the community.

Table 1.
Principles of palliative care (based on [26]).
Any attempt to answer the thesis defined in the title of the paper must come to the conclusion that changes in the paradigms of care are needed on both sides. Healthcare professionals providing palliative care need to get used to caring for people with non-malignant and non-terminal conditions, with sometimes really unpredictable disease and life trajectories, sometimes living for quite long periods despite the constant high probability of death. Acute, life threatening decompensations are a common pattern of living with heart failure. Integrating palliative care can be appropriate in people expecting destination therapy (heart transplantation or mechanical circulatory support implantation) when the risk of death is very high, as high as the probability of drastic improvement in the expected length and quality of life if this therapy succeeds. All these aspects of care go far beyond the usual care pathways developed whilst caring for people with terminal cancer.
Healthcare professionals working in cardiology need to change the usual pattern of care by acknowledging that the risk of decline and dying can be anticipated and openly communicated to patients. Death, in some circumstances, needs to be considered as natural, not only as an avoidable failure of treatment. Paradoxically, supporting people approaching this natural death in the anticipated decline helps them to sustain quality of life and increases satisfaction of care. Involvement of palliative care should be driven by needs and currently is no longer restricted for those who are imminently dying. Acknowledging that including palliative care improves the quality of life of patients and their relatives and does not mean giving up helps to prepare for an inevitable death. Prolonging a life of the best possible quality can be achieved more easily whilst caring together for people with heart failure, along the whole disease trajectory, according to current needs. This approach is depicted in Figure 2.
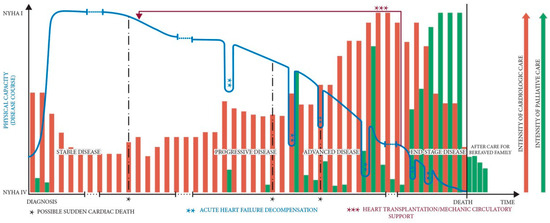
Figure 2.
Heart Failure disease trajectory and superimposed models of care. Disease trajectory describes events over the course of the illness that is shaped by patient’s response to the illness, its management and interactions with caregivers. Palliative care referral can be either integrated early in the disease course or in the more advanced stages. Reprinted from [27] by permission of the Oxford University Press.
Take-home messages
The key aspects of modern palliative care for people living with heart failure (based on [13]):
- Palliative care should be provided to all people with heart failure, who have needs that can be addressed by palliative care interventions. Palliative care should be provided alongside continuously optimised cardiological management.
- Prognostication or risk of death are not indicators of a need for palliative care. The prognosis-based approach has failed and is no longer recommended.
- Needs should be optimally assessed using validated tools. The Needs Assessment Tool: Progressive Disease-Heart Failure (NAT: PD-HF) is a simple tool aiding in the assessment of four domains of needs and in recognising the action needed to address them.
- Needs assessment should be performed regularly and after recognition of trigger events.
- Open and sensitive clinical communication should be fostered, starting from the beginning for those living with the disease. As the disease progresses, any discussion of future health should include elements of advance care planning, if desired by the patient.
- End-of-life interventions should include adjusting management according to actual goals – modification of cardiac implantable electronic devices, adjustment of cardiologic managment and implementing symptom / quality of life targeted interventions.
- The proper setting of care is caring together, not transferring from cardiac to palliative care.
Disclosure statement
No financial support and no potential conflict of interest relevant to this article was reported.
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; et al. ESC Scientific Document Group. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- Komajda, M.; Hanon, O.; Hochadel, M.; Follath, F.; Swedberg, K.; Gitt, A.; et al. Management of octogenarians hospitalized for heart failure in Euro Heart Failure Survey I. Eur Heart J. 2007, 28, 1310–1318. [Google Scholar] [CrossRef]
- Bekelman, D.B.; Hutt, E.; Masoudi, F.A.; Kutner, J.S.; Rumsfeld, J.S. Defining the role of palliative care in older adults with heart failure. Int J Cardiol. 2008, 125, 183–190. [Google Scholar] [CrossRef]
- Rogers, J.G.; Patel, C.B.; Mentz, R.J.; Granger, B.B.; Steinhauser, K.E.; Fiuzat, M.; et al. Palliative Care in Heart Failure: The PAL-HF Randomized, Controlled Clinical Trial. J Am Coll Cardiol. 2017, 70, 331–341. [Google Scholar] [CrossRef]
- Evangelista, L.S.; Liao, S.; Motie, M.; De Michelis, N.; Lombardo, D. On-going palliative care enhances perceived control and patient activation and reduces symptom distress in patients with symptomatic heart failure: A pilot study. Eur J Cardiovasc Nurs. 2014, 13, 116–123. [Google Scholar] [CrossRef]
- Sidebottom, A.C.; Jorgenson, A.; Richards, H.; Kirven, J.; Sillah, A. Inpatient palliative care for patients with acute heart failure: Outcomes from a randomized trial. J Palliat Med. 2015, 18, 134–142. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://www.eapcnet.eu/about-us/what-we-do (accessed on Feburary 2020).
- Rego, F.; Pereira, C.; Rego, G.; Nunes, R. The Psychological and Spiritual Dimensions of Palliative Care: A Descriptive Systematic Review. Neuropsychiatry (London). 2018, 8, 484–494. [Google Scholar] [CrossRef]
- Murray, S.A.; Boyd, K.; Sheikh, A. Palliative care in chronic illness. BMJ. 2005, 330, 611–612. [Google Scholar] [CrossRef]
- Waller, A.; Girgis, A.; Davidson, P.M.; Newton, P.J.; Lecathelinais, C.; Macdonald, P.S.; et al. Facilitating needs-based support and palliative care for people with chronic heart failure: Preliminary evidence for the acceptability, inter-rater reliability, and validity of a needs assessment tool. J Pain Symptom Manage. 2013, 45, 912–925. [Google Scholar] [CrossRef]
- Girgis, A.; et al. Palliative Care Needs Assessment Guidelines; The Centre for Health Research & Psycho-oncology: Newcastle, NSW, Australia, 2006. [Google Scholar]
- Needs Assessment Tool: Progressive Disease Heart Failure (NAT:PD-HF). [Internet]. Available online: https://www.eapcnet.eu/Portals/0/NATPDHF%20adjusted.pdf (accessed on February 2020).
- Sobanski, P.Z.; Alt-Epping, B.; Currow, D.C.; Goodlin, S.J.; Grodzicki, T.; Hogg, K.; et al. Palliative care for people living with heart failure: European Association for Palliative Care Task Force expert position statement. Cardiovasc Res. 2020, 116, 12–27. [Google Scholar] [CrossRef]
- Eychmüller, S. [SENS is making sense on the way to an innovative approach to structure Palliative Care problems]. Ther Umsch. 2012, 69, 87–90. (In German) [Google Scholar] [CrossRef] [PubMed]
- Murray, S.A.; Kendall, M.; Grant, E.; Boyd, K.; Barclay, S.; Sheikh, A. Patterns of social, psychological, and spiritual decline toward the end of life in lung cancer and heart failure. J Pain Symptom Manage. 2007 34, 393–402. [CrossRef]
- Kavalieratos, D.; Kamal, A.H.; Abernethy, A.P.; Biddle, A.K.; Carey, T.S.; Dev, S.; et al. Comparing unmet needs between community-based palliative care patients with heart failure and patients with cancer. J Palliat Med. 2014, 17, 475–481. [Google Scholar] [CrossRef]
- Pham, P.C.; Khaing, K.; Sievers, T.M.; Pham, P.M.; Miller, J.M.; Pham, S.V.; et al. 2017 update on pain management in patients with chronic kidney disease. Clin Kidney J. 2017, 10, 688–697. [Google Scholar] [CrossRef]
- Denvir, M.A.; Murray, S.A.; Boyd, K.J. Future care planning: A first step to palliative care for all patients with advanced heart disease. Heart. 2015, 101, 1002–1007. [Google Scholar] [CrossRef] [PubMed]
- Rietjens, J.A.C.; Sudore, R.L.; Connolly, M.; van Delden, J.J.; Drickamer, M.A.; Droger, M.; et al. European Association for Palliative Care. Definition and recommendations for advance care planning: An international consensus supported by the European Association for Palliative Care. Lancet Oncol. 2017, 18, e543–e551. [Google Scholar] [CrossRef] [PubMed]
- Ratcliffe, T.M. Healthcare providers need to improve communication with patients who have heart failure. Br J Gen Pract. 2007, 57, 180–182. [Google Scholar]
- Houben, C.H.; Spruit, M.A.; Schols, J.M.; Wouters, E.F.; Janssen, D.J. Patient-Clinician Communication About End-of-Life Care in Patients With Advanced Chronic Organ Failure During One Year. J Pain Symptom Manage. 2015, 49, 1109–1115. [Google Scholar] [CrossRef]
- Tajouri, T.H.; Ottenberg, A.L.; Hayes, D.L.; Mueller, P.S. The use of advance directives among patients with implantable cardioverter defibrillators. Pacing Clin Electrophysiol. 2012, 35, 567–573. [Google Scholar] [CrossRef]
- Goldstein, N.E.; Kalman, J.; Kutner, J.S.; Fromme, E.K.; Hutchinson, M.D.; Lipman, H.I.; et al. A study to improve communication between clinicians and patients with advanced heart failure: Methods and challenges behind the working to improve discussions about defibrillator management trial. J Pain Symptom Manage. 2014, 48, 1236–1246. [Google Scholar] [CrossRef] [PubMed]
- Padeletti, L.; Arnar, D.O.; Boncinelli, L.; Brachman, J.; Camm, J.A.; Daubert, J.C.; et al. Reviewers; EuropeanHeart RhythmAssociation; Heart Rhythm Society. EHRA Expert Consensus Statement on the management of cardiovascular implantable electronic devices in patients nearing end of life or requesting withdrawal of therapy. Europace. 2010, 12, 1480–1489. [Google Scholar] [CrossRef] [PubMed]
- Lampert, R.; Hayes, D.L.; Annas, G.J.; Farley, M.A.; Goldstein, N.E.; Hamilton, R.M.; et al. American College of Cardiology; American Geriatrics Society; American Academy of Hospice and Palliative Medicine; American Heart Association; European Heart Rhythm Association; Hospice and Palliative Nurses Association. HRS Expert Consensus Statement on the Management of Cardiovascular Implantable Electronic Devices (CIEDs) in patients nearing end of life or requesting withdrawal of therapy. Heart Rhythm. 2010, 7, 1008–1026. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://hospicecare.com/what-we-do/publications/getting-started/6-principles-of-palliative-care (accessed on July 2020).
- Sobanski, P. Palliative and end-of-life care in elderly subjects with cardiovascular disease. In ESC CardioMed, 3rd ed.; Camm, J.A., et al., Eds.; Oxford University Press: Oxford, UK, 2018; pp. 2940–2944. [Google Scholar]
© 2020 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.