Prognostic Role of Atrial Fibrillation in Acute Coronary Syndromes: A Real-Life, Contemporary Analysis
Abstract
Introduction
Methods
Study population
Endpoints
Statistical analysis
Results
ACS-AF patients’ characteristics
In-hospital mortality and its predictors
One-year Follow up
Major Bleeding
Discussion
- –
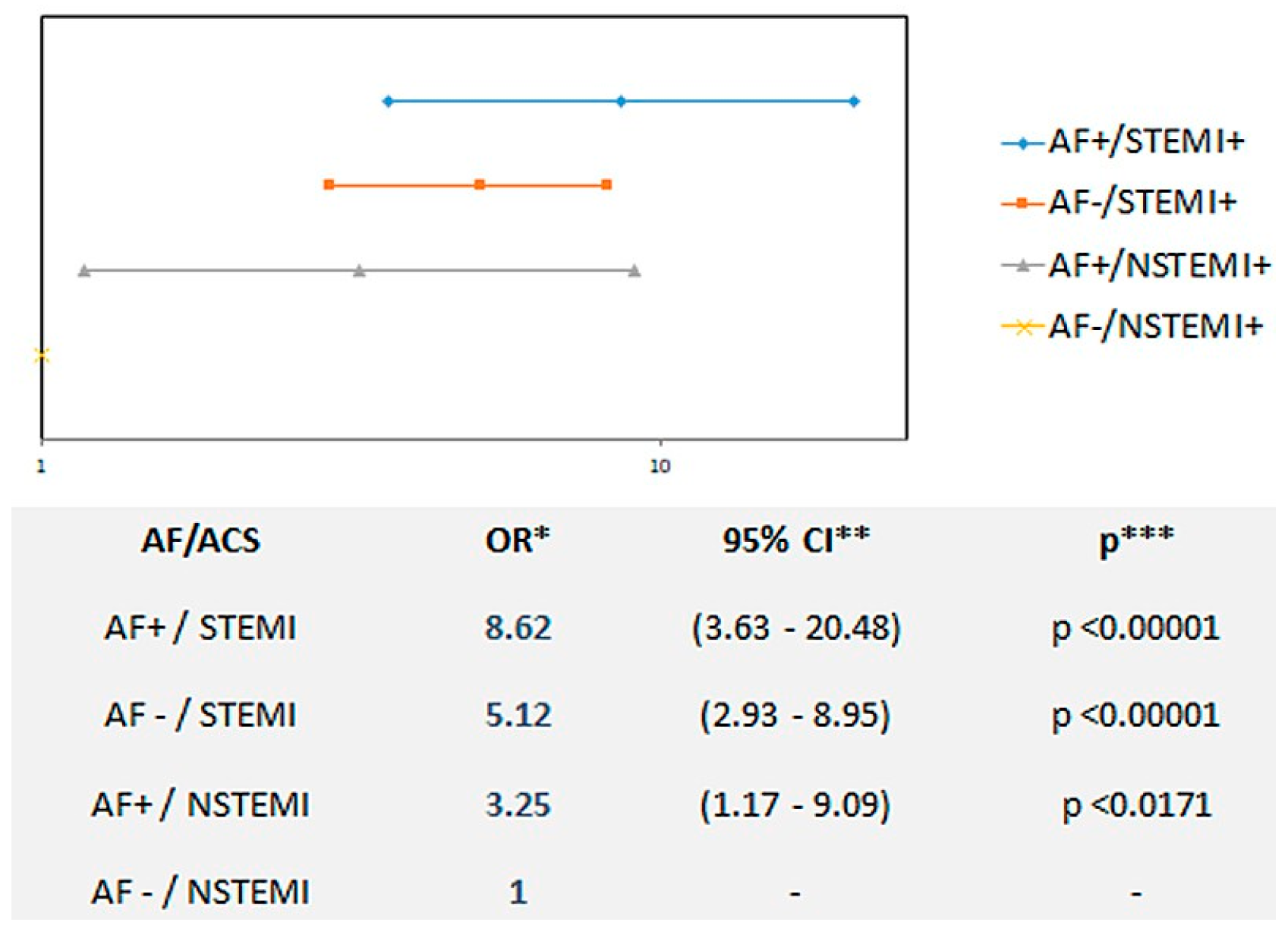
- The presence of atrial fibrillation in the clinical context of an ACS should be regarded as a red flag identifying those patients at higher risk of in-hospital mortality.
- –
- An interplay between presence/absence of AF and ACS clinical presentation (NSTEMI vs STEMI) was clearly evident from a prognostic perspective.
- –
- Owing to the lack of significance after multivariable analysis (adjustment for ACS type and age), the role of AF as an independent prognosticator in ACS remains elusive.
Conclusion
Disclosure statement
References
- Al Khdair, D.; Alshengeiti, L.; Elbarouni, B.; Yan, R.T.; Grondin, F.R.; Spencer, F.A.; et al. Global Registry of Acute Coronary Events (GRACE/GRACE2) and the Canadian Registry of Coronary Events (CANRACE) Investigators. Management and outcome of acute coronary syndrome patients in relation to prior history of atrial fibrillation. Can J Cardiol. 2012, 28, 443–449. [Google Scholar] [CrossRef]
- Rathore, S.S.; Berger, A.K.; Weinfurt, K.P.; Schulman, K.A.; Oetgen, W.J.; Gersh, B.J.; et al. Acute myocardial infarction complicated by atrial fibrillation in the elderly: prevalence and outcomes. Circulation. 2000, 101, 969–974. [Google Scholar] [CrossRef]
- Schmitt, J.; Duray, G.; Gersh, B.J.; Hohnloser, S.H. Atrial fibrillation in acute myocardial infarction: a systematic review of the incidence, clinical features and prognostic implications. Eur Heart J. 2009, 30, 1038–1045. [Google Scholar] [CrossRef]
- Lau, D.H.; Huynh, L.T.; Chew, D.P.; Astley, C.M.; Soman, A.; Sanders, P. Prognostic impact of types of atrial fibrillation in acute coronary syndromes. Am J Cardiol. 2009, 104, 1317–1323. [Google Scholar] [CrossRef]
- Podolecki, T.; Lenarczyk, R.; Kowalczyk, J.; Kurek, T.; Boidol, J.; Chodor, P.; et al. Effect of type of atrial fibrillation on prognosis in acute myocardial infarction treated invasively. Am J Cardiol. 2012, 109, 1689–1693. [Google Scholar] [CrossRef] [PubMed]
- González-Pacheco, H.; Eid-Lidt, G.; Altamirano-Castillo, A.; Álvarez-Sangabriel, A.; González-Hermosillo, A.; Meléndez-Ramírez, G.; et al. Prevalence and prognostic implications of different types of atrial fibrillation in patients admitted to a coronary care unit. Int J Cardiol. 2014, 172, e379–e381. [Google Scholar] [CrossRef]
- Lopes, R.D.; Pieper, K.S.; Horton, J.R.; Al-Khatib, S.M.; Newby, L.K.; Mehta, R.H.; et al. Short- and long-term outcomes following atrial fibrillation in patients with acute coronary syndromes with or without ST-segment elevation. Heart. 2008, 94, 867–873. [Google Scholar] [CrossRef]
- Rubboli, A.; Schlitt, A.; Kiviniemi, T.; Biancari, F.; Karjalainen, P.P.; Valencia, J.; et al. AFCAS Study Group. One-year outcome of patients with atrial fibrillation undergoing coronary artery stenting: an analysis of the AFCAS registry. Clin Cardiol. 2014, 37, 357–364. [Google Scholar] [CrossRef]
- Rene, A.G.; Généreux, P.; Ezekowitz, M.; Kirtane, A.J.; Xu, K.; Mehran, R.; et al. Impact of atrial fibrillation in patients with ST-elevation myocardial infarction treated with percutaneous coronary intervention (from the HORIZONS-AMI [Harmonizing Outcomes With Revascularization and Stents in Acute Myocardial Infarction] trial). Am J Cardiol. 2014, 113, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Rubboli, A.; Sciahbasi, A.; Briguori, C.; Saia, F.; Palmieri, C.; Moroni, L.A.; et al. WARfarin and coronary STENTing registry. In-hospital management and outcome of patients on warfarin undergoing coronary stent implantation: results of the multicenter, prospective WARfarin and coronary STENTing (WAR-STENT) registry. J Invasive Cardiol. 2013, 25, 170–176. [Google Scholar] [PubMed]
- Lamberts, M.; Gislason, G.H.; Olesen, J.B.; Kristensen, S.L.; Schjerning Olsen, A.M.; Mikkelsen, A.; et al. Oral anticoagulation and antiplatelets in atrial fibrillation patients after myocardial infarction and coronary intervention. J Am Coll Cardiol. 2013, 62, 981–989. [Google Scholar] [CrossRef] [PubMed]
- Pilgrim, T.; Kalesan, B.; Zanchin, T.; Pulver, C.; Jung, S.; Mattle, H.; et al. Impact of atrial fibrillation on clinical outcomes among patients with coronary artery disease undergoing revascularisation with drug-eluting stents. EuroIntervention. 2013, 8, 1061–1071. [Google Scholar] [CrossRef]
- Windecker, S.; Kolh, P.; Alfonso, F.; Collet, J.P.; Cremer, J.; Falk, V.; et al. Authors/Task Force members. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014, 35, 2541–2619. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Collet, J.P.; Haude, M.; Byrne, R.; Chung, E.H.; Fauchier, L.; et al. ESC Scientific Document Group. 2018 Joint European consensus document on the management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous cardiovascular interventions: a joint consensus document of the European Heart Rhythm Association (EHRA), European Society of Cardiology Working Group on Thrombosis, European Association of Percutaneous Cardiovascular Interventions (EAPCI), and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS), Latin America Heart Rhythm Society (LAHRS), and Cardiac Arrhythmia Society of Southern Africa (CASSA). Europace. 2019, 21, 192–193. [Google Scholar] [CrossRef]
- Gorenek, B.; Blomström Lundqvist, C.; Brugada Terradellas, J.; Camm, A.J.; Hindricks, G.; Huber, K.; et al. Cardiac arrhythmias in acute coronary syndromes: position paper from the joint EHRA, ACCA, and EAPCI task force. Europace. 2014, 16, 1655–1673. [Google Scholar] [CrossRef]
- Heidbuchel, H.; Verhamme, P.; Alings, M.; Antz, M.; Diener, H.C.; Hacke, W.; et al. Updated European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist anticoagulants in patients with non-valvular atrial fibrillation. Europace. 2015, 17, 1467–1507. [Google Scholar] [CrossRef]
- Mehta, S.R.; Bainey, K.R.; Cantor, W.J.; Lordkipanidzé, M.; Marquis-Gravel, G.; Robinson, S.D.; et al. members of the Secondary Panel. 2018 Canadian Cardiovascular Society/Canadian Association of interventional Cardiology focused update of the guidelines for the use of antiplatelet therapy. Can J Cardiol. 2018, 34, 214–233. [Google Scholar] [CrossRef]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Simoons, M.L.; Chaitman, B.R.; White, H.D.; et al. Writing Group on the Joint ESC/ACCF/AHA/WHF Task Force for the Universal Definition of Myocardial Infarction; ESC Committee for Practice Guidelines (CPG). Third universal definition of myocardial infarction. Eur Heart J. 2012, 33, 2551–2567. [Google Scholar] [CrossRef] [PubMed]
- Camm, A.J.; Lip, G.Y.; De Caterina, R.; Savelieva, I.; Atar, D.; Hohnloser, S.H.; et al. ESC Committee for Practice Guidelines-CPG; Document Reviewers. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation--developed with the special contribution of the European Heart Rhythm Association. Europace. 2012, 14, 1385–1413. [Google Scholar] [CrossRef] [PubMed]
- Cutlip, D.E.; Windecker, S.; Mehran, R.; Boam, A.; Cohen, D.J.; van Es, G.A.; et al. Academic Research Consortium. Clinical end points in coronary stent trials: a case for standardized definitions. Circulation. 2007, 115, 2344–2351. [Google Scholar] [CrossRef]
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; et al. Standardized bleeding definitions for cardiovascular clinical trials: a consensus report from the Bleeding Academic Research Consortium. Circulation. 2011, 123, 2736–2747. [Google Scholar] [CrossRef] [PubMed]
- McManus, D.D.; Huang, W.; Domakonda, K.V.; Ward, J.; Saczysnki, J.S.; Gore, J.M.; et al. Trends in atrial fibrillation in patients hospitalized with an acute coronary syndrome. Am J Med. 2012, 125, 1076–1084. [Google Scholar] [CrossRef]
- Lopes, R.D.; Li, L.; Granger, C.B.; Wang, T.Y.; Foody, J.M.; Funk, M.; et al. Atrial fibrillation and acute myocardial infarction: antithrombotic therapy and outcomes. Am J Med. 2012, 125, 897–905. [Google Scholar] [CrossRef]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; et al. ESC Scientific Document Group. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS: The Task Force for the management of atrial fibrillation of the European Society of Cardiology (ESC). Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef]
- Angeli, F.; Reboldi, G.; Garofoli, M.; Ramundo, E.; Poltronieri, C.; Mazzotta, G.; et al. Atrial fibrillation and mortality in patients with acute myocardial infarction: a systematic overview and meta-analysis. Curr Cardiol Rep. 2012, 14, 601–610. [Google Scholar] [CrossRef]
- Mehta, R.H.; Dabbous, O.H.; Granger, C.B.; Kuznetsova, P.; Kline-Rogers, E.M.; Anderson, F.A., Jr.; et al. GRACE Investigators. Comparison of outcomes of patients with acute coronary syndromes with and without atrial fibrillation. Am J Cardiol. 2003, 92, 1031–1036. [Google Scholar] [CrossRef]
- Poçi, D.; Hartford, M.; Karlsson, T.; Edvardsson, N.; Caidahl, K. Effect of new versus known versus no atrial fibrillation on 30-day and 10-year mortality in patients with acute coronary syndrome. Am J Cardiol. 2012, 110, 217–221. [Google Scholar] [CrossRef]
- Biasco, L.; Radovanovic, D.; Moccetti, M.; Rickli, H.; Roffi, M.; Eberli, F.; et al. New-onset or Pre-existing Atrial Fibrillation in Acute Coronary Syndromes: Two Distinct Phenomena With a Similar Prognosis. Rev Esp Cardiol (Engl Ed). 2019, 72, 383–391. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; FitzGerald, G.; Goldberg, R.J.; Gore, J.; McManus, R.H.; Awad, H.; et al. TRACE-CORE Investigators. Performance of the GRACE risk score 2.0 simplified algorithm for predicting 1-year death following hospitalisation for an acute coronary syndrome in a contemporary multiracial cohort. Am J Cardiol. 2016, 118, 1105–1110. [Google Scholar] [CrossRef]
- Gibson, C.M.; Mehran, R.; Bode, C.; Halperin, J.; Verheugt, F.W.; Wildgoose, P.; et al. Prevention of bleeding in patients with atrial fibrillation undergoing PCI. N Engl J Med. 2016, 375, 2423–2434. [Google Scholar] [CrossRef] [PubMed]
- Cannon, C.P.; Bhatt, D.L.; Oldgren, J.; Lip, G.Y.H.; Ellis, S.G.; Kimura, T.; et al. RE-DUAL PCI Steering Committee and Investigators. Dual antithrombotic therapy with dabigatran after PCI in atrial fibrillation. N Engl J Med. 2017, 377, 1513–1524. [Google Scholar] [CrossRef]
- Lopes, R.D.; Heizer, G.; Aronson, R.; Vora, A.N.; Massaro, T.; Mehran, R.; et al. AUGUSTUS Investigators. Antithrombotic therapy after acute coronary syndrome or PCI in atrial fibrillation. N Engl J Med. 2019, 380, 1509–1524. [Google Scholar] [CrossRef] [PubMed]
- Vranckx, P.; Valgimigli, M.; Eckardt, L.; Tijssen, J.; Lewalter, T.; Gargiulo, G.; et al. Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen after successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): a randomised, open-label, phase 3b trial. Lancet. 2019, 394, 1335–1343. [Google Scholar] [CrossRef] [PubMed]
- Kozieł, M.; Potpara, T.S.; Lip, G.Y.H. Triple therapy in patients with atrial fibrillation and acute coronary syndrome or percutaneous coronary intervention/stenting. Res Pract Thromb Haemost. 2020, 4, 357–365. [Google Scholar] [CrossRef] [PubMed]


| ACS-AF cohort | |
|---|---|
| Number | 187 |
| Age (years) | 74 ± 11 |
| Female (%) | 31 |
| ACS STEMI (%) | 43.8 |
| ACS NSTEMI (%) | 56.2 |
| Cardiogenic shock (%) | 10.7 |
| New onset AF (%) | 46 |
| CHADS2-VASC score | 4.1 ± 1.5 |
| HAS-BLED score | 3 ± 1.2 |
| LVEF (%) | 46 ± 12.5 |
| Radial access (%) | 19.5 |
| Acute treatment | |
| – PCI (%) | 64.5 |
| – CABG (%) | 7.5 |
| – Medical (%) | 28 |
| Mortality | OR | 95% CI | p-value |
|---|---|---|---|
| AF− AF+ | 1.00 (base) 1.44 | – (0.78–2.65) | – 0.246 |
| ST− ST+ | 1.00 (base) 5.56 | – (3.38–9.15) | – 0.0001 |
| Sex female Sex male | 1.00 (base) 1.03 | – (0.65–1.64) | – 0.887 |
| Age, per year | 1.06 | (1.04–1.08) | 0.0001 |
| Triple therapy | SAPT + OAC | DAPT | p-value | |
|---|---|---|---|---|
| Number | 45 | 23 | 88 | - |
| Age (years) | 77 ± 7 | 76 ± 11 | 71 ± 12 | 0.04 |
| Gender female (%) | 31.3 | 21.7 | 32.7 | 0.65 |
| STEMI/NSTEMI (%) | 33.3/66.7 | 39.1/60.9 | 50/50 | 0.14 |
| Cardiogenic shock (%) | 6.3 | 13 | 13.3 | 0.42 |
| New onset AF (%) | 41.7 | 60.9 | 42.9 | 0.27 |
| CHADS2-VASC score | 4± 1.5 | 4.7± 1.9 | 4.1± 1.6 | 0.24 |
| HAS-BLED score | 3 ± 1.3 | 3.1 ± 1 | 2.9 ± 1.3 | 0.64 |
| LVEF (%) | 47 ± 12.3 | 43 ± 9.8 | 46 ± 13.1 | 0.35 |
| Radial access (%) | 20.8 | 8.7 | 21.4 | 0.41 |
| Acute treatment | ||||
| – PCI, n (%) | 34 (75.6) | 11 (47.8) | 62 (70.5) | 0.04 |
| – CABG, n (%) | 0 (0) | 6 (26.1) | 2 (2.2) | 0.001 |
| – Medical, n (%) | 11 (24.4) | 6 (26.1) | 24 (27.3) | 0.94 |
| 1-year outcomes | Triple therapy n = 45 | AOC + SAPT n = 23 | DAPT n = 88 | p-value* |
|---|---|---|---|---|
| Death n; HR; 95% CI | n = 3 HR = 1.48 95% CI 0.33–6.63 | n = 3 HR = 3.06 95% CI [0.68 -13.67] | n = 4 HR = 1 (base) | 0.31 |
| MACE n; HR; 95% CI | n = 7 HR = 1.95 95% CI 0.68–5.51 | n = 3 HR = 1.83 95% CI [0.47 -7.10] | n = 7 HR = 1 (base) | 0.41 |
| Major bleeding n; HR; 95% CI | n = 5 HR = 1.68 95% CI 0.51–5.50 | n = 0 – – | n = 6 HR = 1 (base) | 0.27 |
| 1 year outcomes | Triple therapy n = 45 | OAC + SAPT n = 23 | DAPT n = 88 | p-value* |
|---|---|---|---|---|
| Deaths HR; 95% CI | HR = 2.68 95% CI 0.39–18.51 | HR = 3.66 95% CI 0.44–30.26 | HR = 1 (base) | 0.44 |
| MACE HR; 95% CI | HR = 3.41 95% CI 0.93–12.45 | HR = 1.52 95% CI 0.25–9.20 | HR = 1 (base) | 0.17 |
| Major bleeding HR; 95% CI | HR = 2.33 95% CI 0.64–8.52 | – – | HR = 1 (base) | 0.13 |
© 2020 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Boris, A.; Luigi, B.; Serena, M.; Stefano, S.; Alessandra, C.; Elena, P.; Tiziano, M.; Marco, M.; Catherine, K.; Giovanni, P. Prognostic Role of Atrial Fibrillation in Acute Coronary Syndromes: A Real-Life, Contemporary Analysis. Cardiovasc. Med. 2020, 23, w02123. https://doi.org/10.4414/cvm.2020.02123
Boris A, Luigi B, Serena M, Stefano S, Alessandra C, Elena P, Tiziano M, Marco M, Catherine K, Giovanni P. Prognostic Role of Atrial Fibrillation in Acute Coronary Syndromes: A Real-Life, Contemporary Analysis. Cardiovascular Medicine. 2020; 23(5):w02123. https://doi.org/10.4414/cvm.2020.02123
Chicago/Turabian StyleBoris, Adjibodou, Biasco Luigi, Marcon Serena, Svab Stefano, Chiodini Alessandra, Pasotti Elena, Moccetti Tiziano, Moccetti Marco, Klersy Catherine, and Pedrazzini Giovanni. 2020. "Prognostic Role of Atrial Fibrillation in Acute Coronary Syndromes: A Real-Life, Contemporary Analysis" Cardiovascular Medicine 23, no. 5: w02123. https://doi.org/10.4414/cvm.2020.02123
APA StyleBoris, A., Luigi, B., Serena, M., Stefano, S., Alessandra, C., Elena, P., Tiziano, M., Marco, M., Catherine, K., & Giovanni, P. (2020). Prognostic Role of Atrial Fibrillation in Acute Coronary Syndromes: A Real-Life, Contemporary Analysis. Cardiovascular Medicine, 23(5), w02123. https://doi.org/10.4414/cvm.2020.02123




