Solution
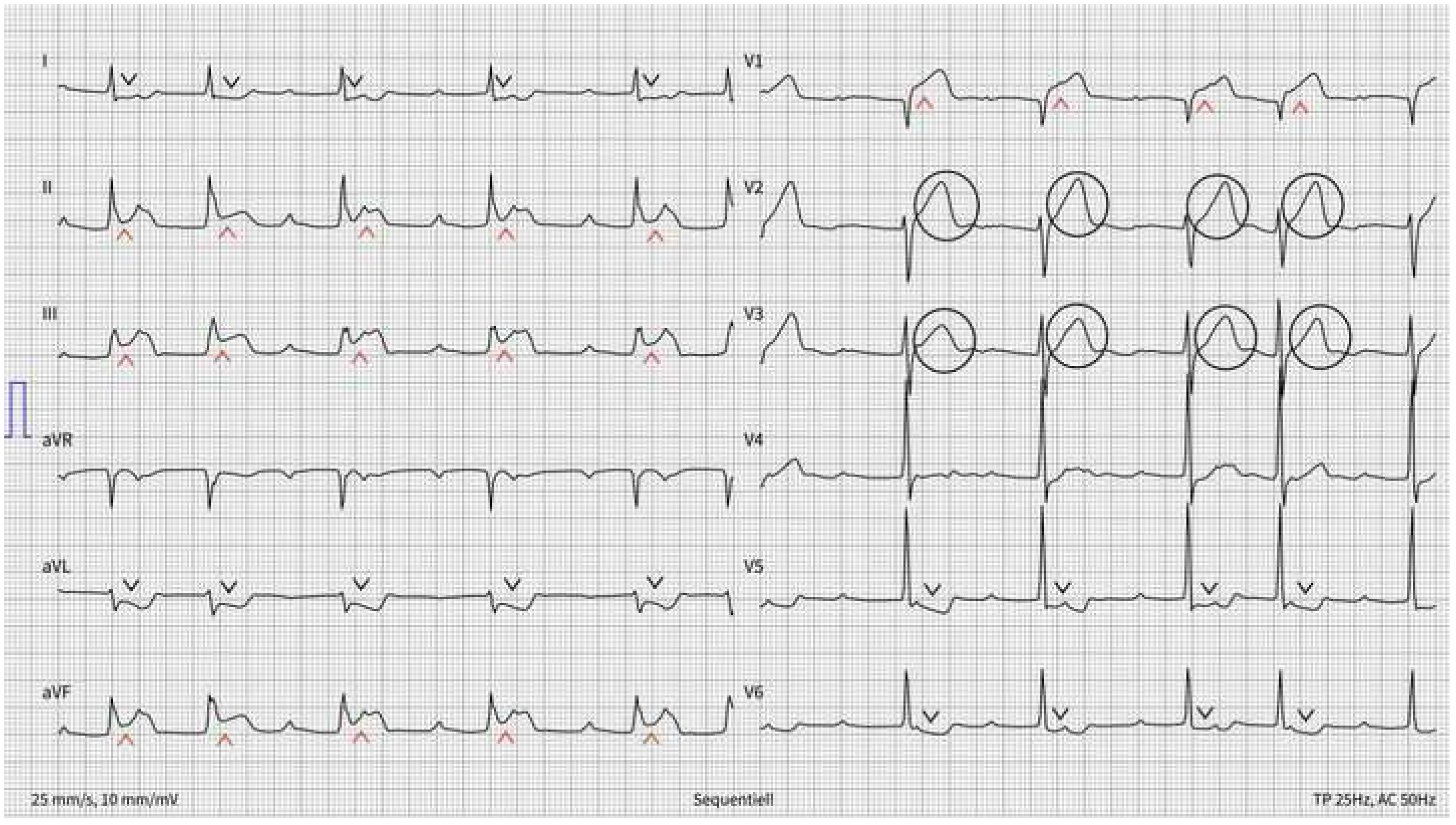
There is an irregular rhythm with a ventricular rate of 61 bpm. QRS complexes are narrow. Big amplitude T-waves are seen in V1 through V3 (circled). There is significant ST segment elevation in leads II-III, aVF and V1 (red arrowheads) with reciprocal ST segment depression in leads aVL, V5 and V6 (black arrowheads). An increased number of P waves (black and red arrows, corresponding respectively to conducted and non-conducted P waves), compared to the number of QRS complexes (green arrows), can be counted. The PP interval is regular. An increasing PR interval (red lines with increasing length) is measured, with a resulting non-conducted P wave (2nd red arrow and terminated red line), compatible with a Wenckebach phenomenon. The non-conducted P wave is merged in the QRS complex and can be better visualized in V2 and V3 (leftward bending red arrows). The following QRS complex (green arrowhead) results from conduction with a very long PR interval or represents a junctional escape beat. The PR interval of the preceding P wave is indeed too short to result in AV conduction. Thereafter, a 2:1 block occurs for 2 cycles (underlined in black), followed by a repeat Wenckebach phenomenon (red lines with increasing length and finally terminated). The blocked P wave is hidden in the QRS complex and can be better spotted in V5 and V6 (rightward bending red arrows).
Based on these ECGs, an inferior ST-segment elevation myocardial infarction (STEMI) with associated atrioventricular (AV) nodal conduction abnormalities is suspected. The ST-segment elevation in lead III > II associated with an ST-segment elevation in V1 suggest an associated right ventricular infarction [
1]. Additionally, a 2nd degree Mobitz type I AV block with 2:1 ventricular conduction is present. An intranodal rather than infranodal AV block is suggested, due to the prolonged PR interval and documented Wenckebach phenomenon with 3:2 conduction [
2]. A proximal to mid-right coronary artery (RCA) lesion is probable, with resulting ischemia of the right ventricle, as well as the AV nodal artery perfusion area.
The cath lab should be immediately activated and further management should follow the STEMI guidelines. A right-sided 12-lead ECG should be obtained to confirm right ventricular infarction, and pre-load reducing drugs (i.e., opiates, nitroglycerine) used with caution. Finally, due to 2nd degree AV block, usage of AV blocking drugs (i.e., beta-blockers, calcium channel blockers) should be avoided. This is particularly relevant when the transradial approach is selected for percutaneous revascularization.
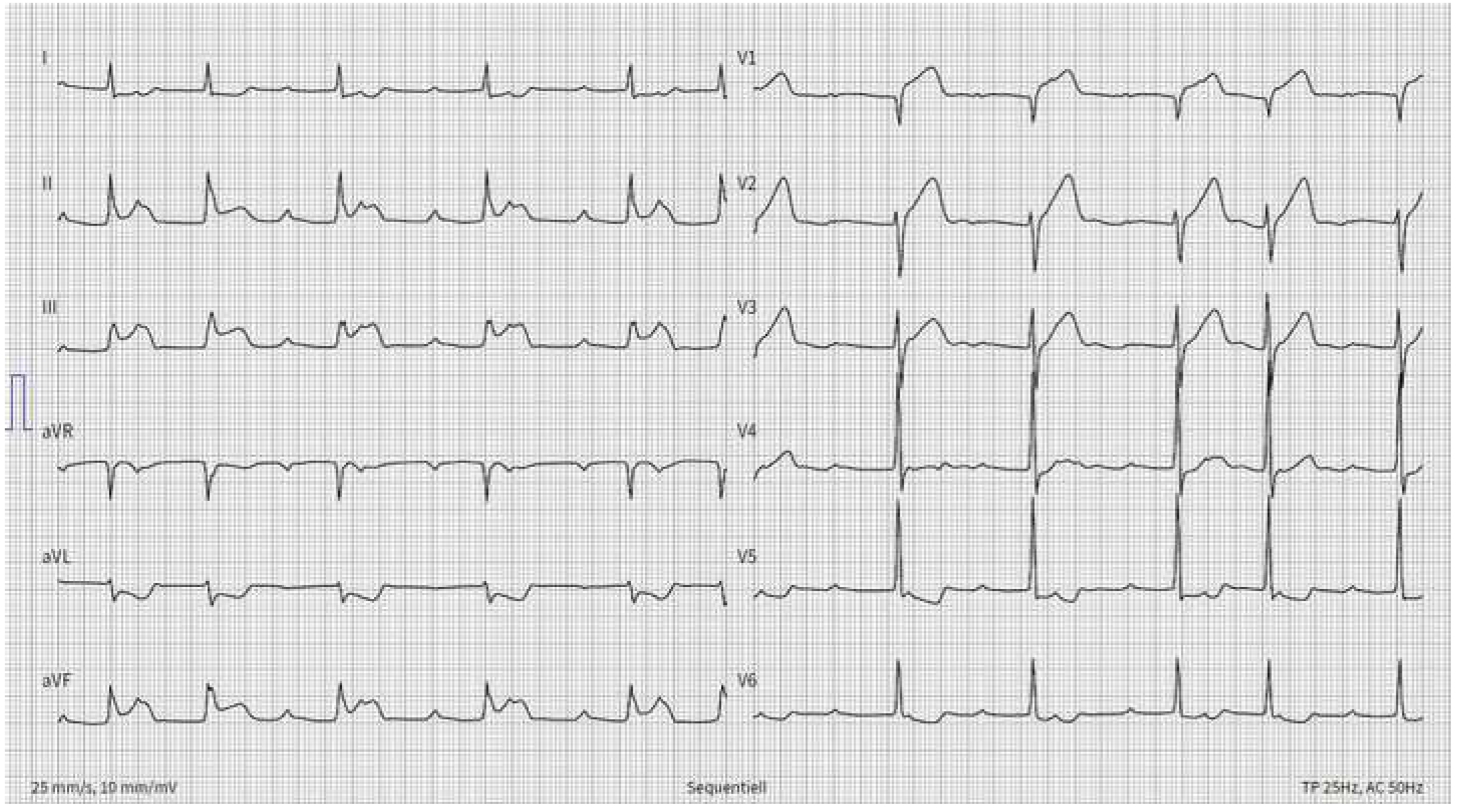
The coronarangiography confirmed an inferior wall STEMI due to a thrombotic occlusion of the mid-right coronary artery (RCA) (
Figure 1A).
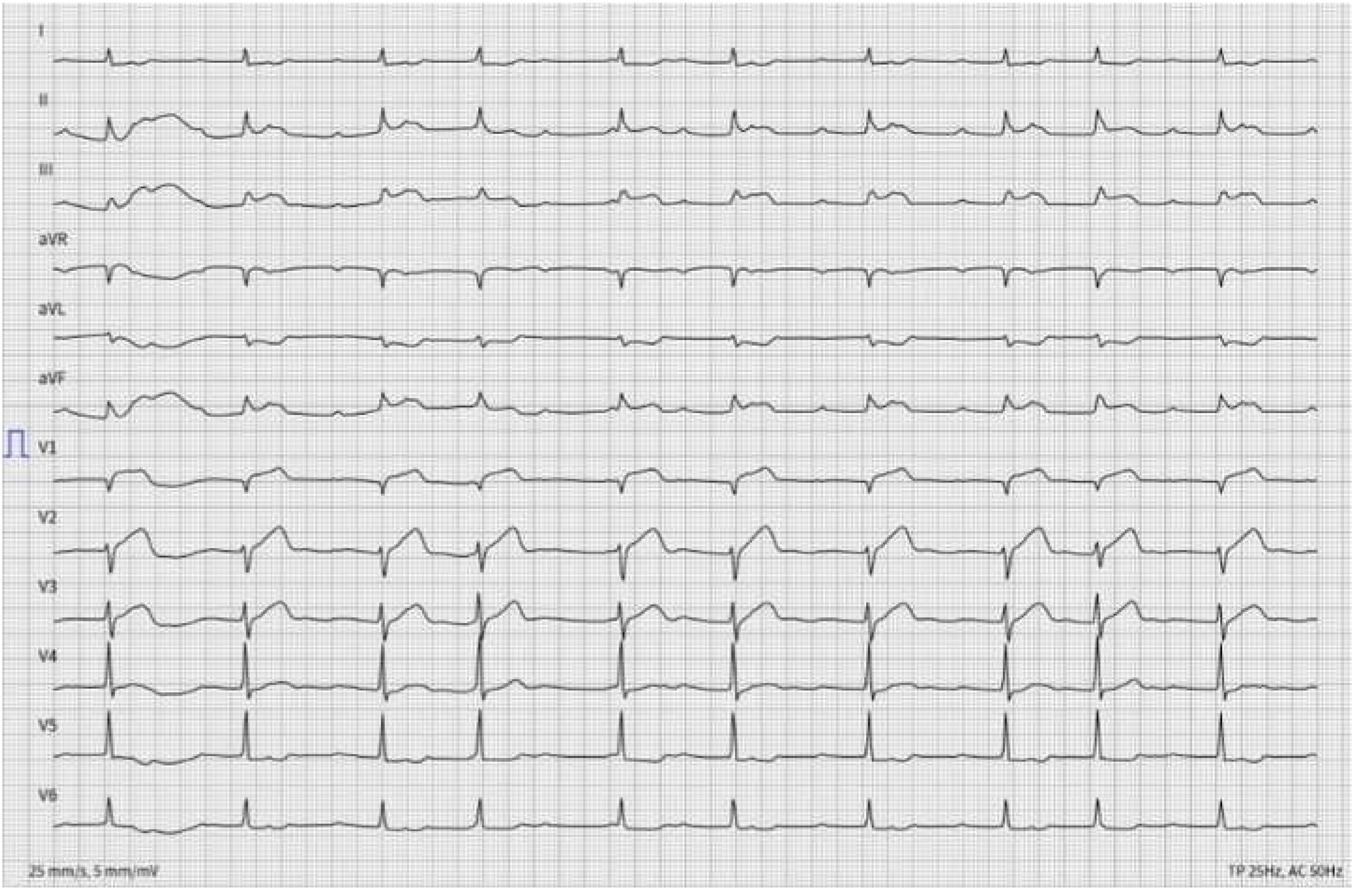
Figure 1B shows the final angiographic result after balloon angioplasty and stenting with a single drug-eluting stent, with subsequent reperfusion of the AV nodal artery.
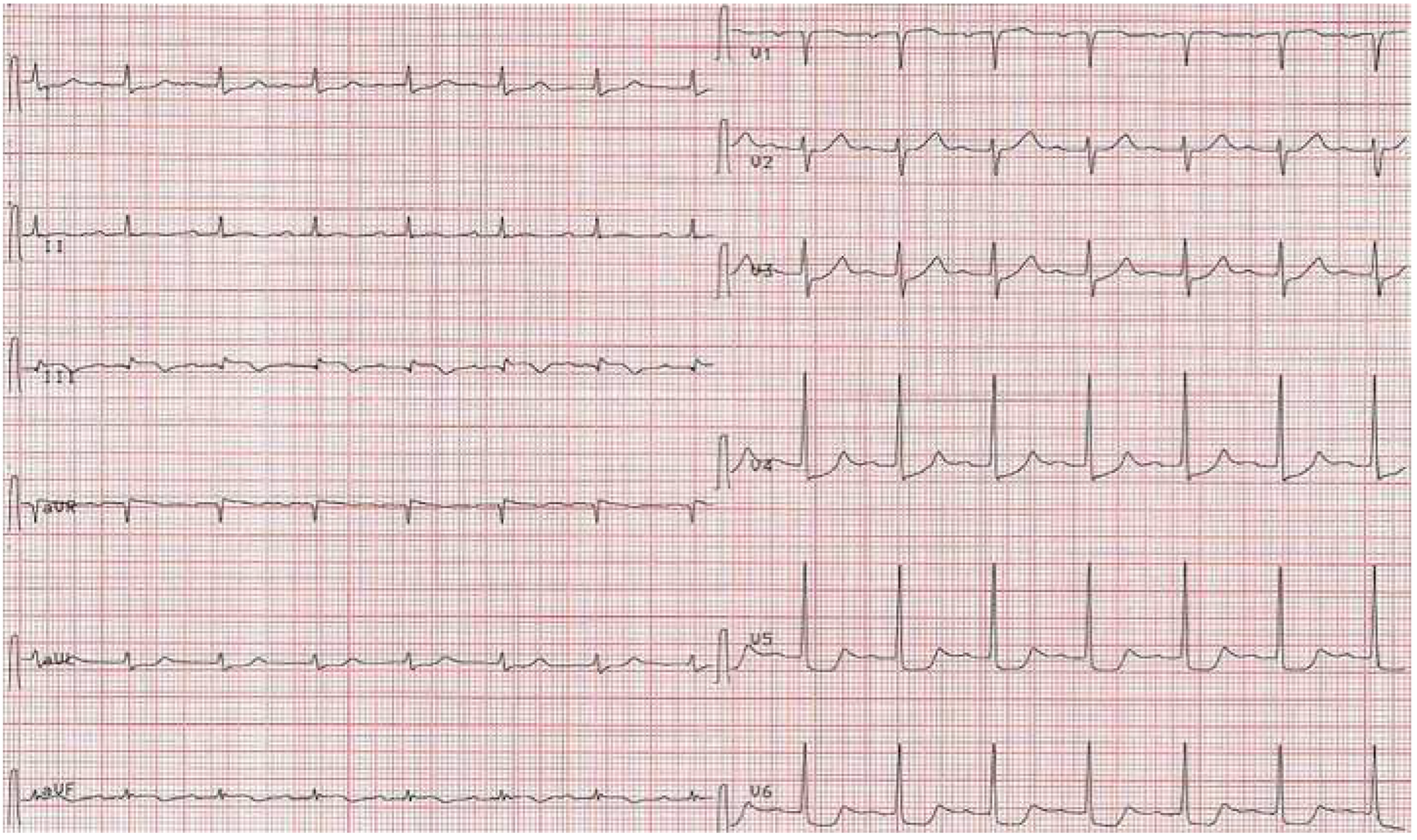
ECG C, obtained 1 h after percutaneous coronary intervention (PCI) shows a regular sinus rhythm with at a heart rate of 87 bpm and a 1st degree AV block (AV interval 232 ms). Early recovery from the ischemia-related 2:1 AV block after successful recanalization of the RCA is observed.
High degree AV block (HAVB) can complicate up to 7% of patients with inferior STEMI and about 9% of patients with STEMI require a permanent pacemaker implantation due to persistent or recurrent HAVB [
3]. In patients with 2nd degree, Mobitz type I AV block, no specific therapy is needed other than ischemia-related therapy. Atropine should be used in symptomatic patients with a ventricular rate that does not exceed 50 bpm, with premature ventricular complexes and/or associated bundle branch blocks or signs of heart failure [
2]. Temporary pacing therapy is rarely needed.
An anteroseptal wall myocardial infarction (MI) can also cause AV conduction abnormalities due to ischemia in the perfusion zone of the septal perforators of the left anterior descending artery (LAD). However, in this case, ischemia would involve the infranodal conduction system (i.e., the conduction system below the AV node and the bundle of His), which would predominantly result in a 2nd degree, Mobitz type II AV block. As this situation increases the potential for progression to complete heart block, temporary pacing should be considered [
2].