Minimal Use of Contrast Media in Patients with Severe Chronic Kidney Disease Undergoing Transcatheter Aortic Valve Implantation
Abstract
Introduction
Methods
Study population
TAVI work-up and MR protocols
TAVI procedure
Procedural modifications in patients with severe chronic kidney disease
Definitions
Statistical analysis
Results
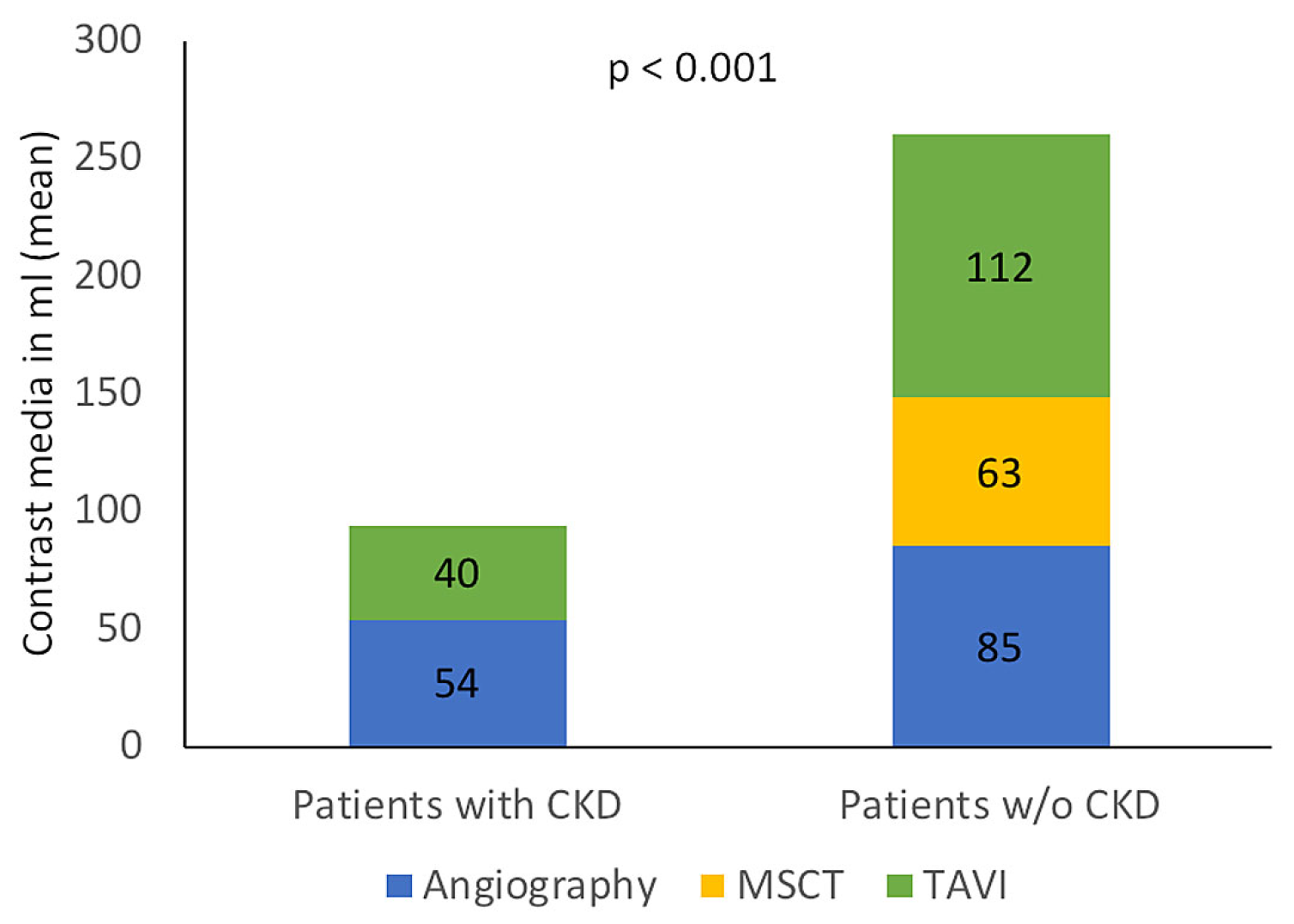
Use of contrast media for TAVI work-up and procedure
In-hospital outcomes
30 day and 6 month outcomes
Discussion
Pathophysiology of acute kidney injury
Relevance of contrast media
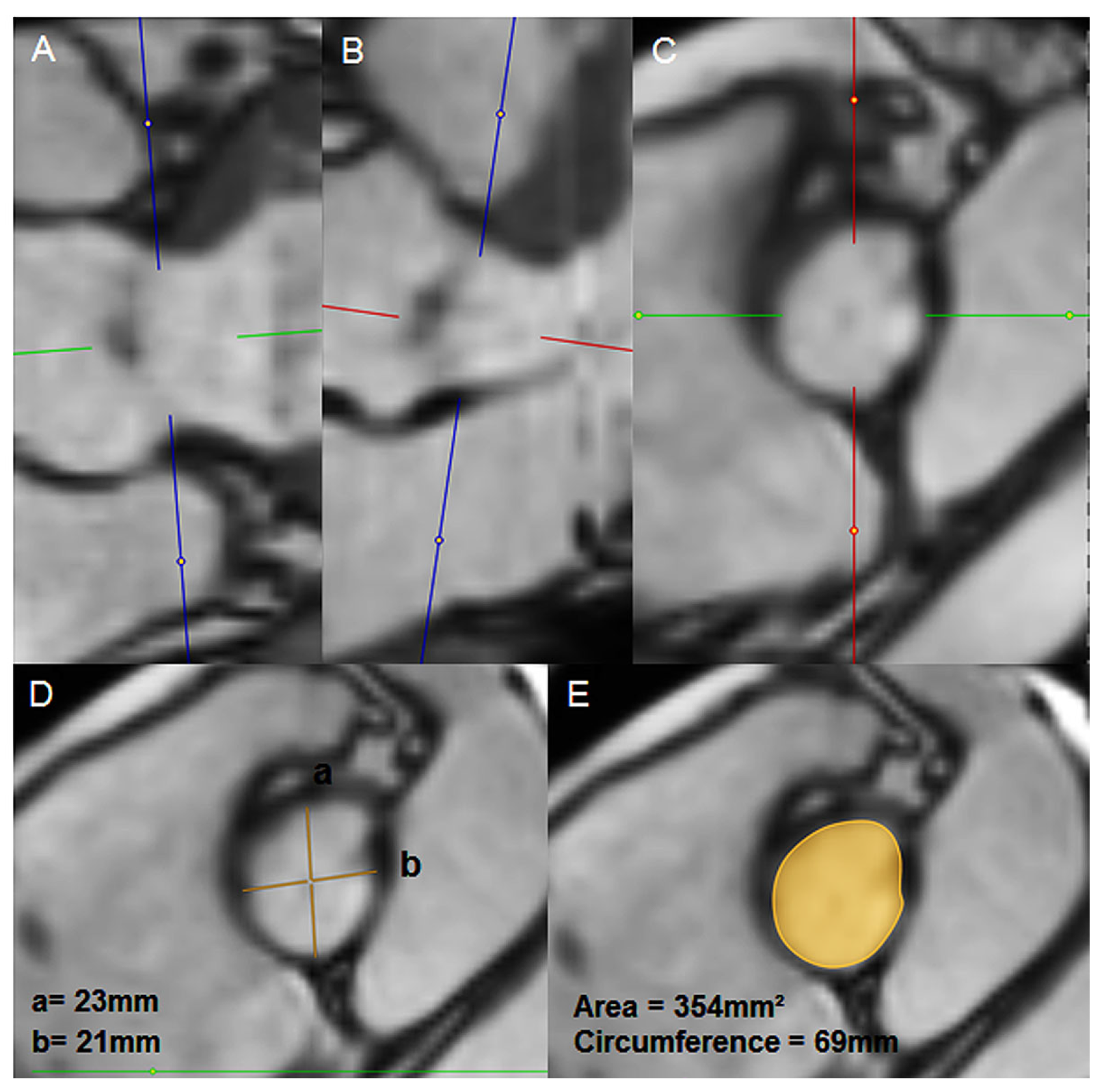
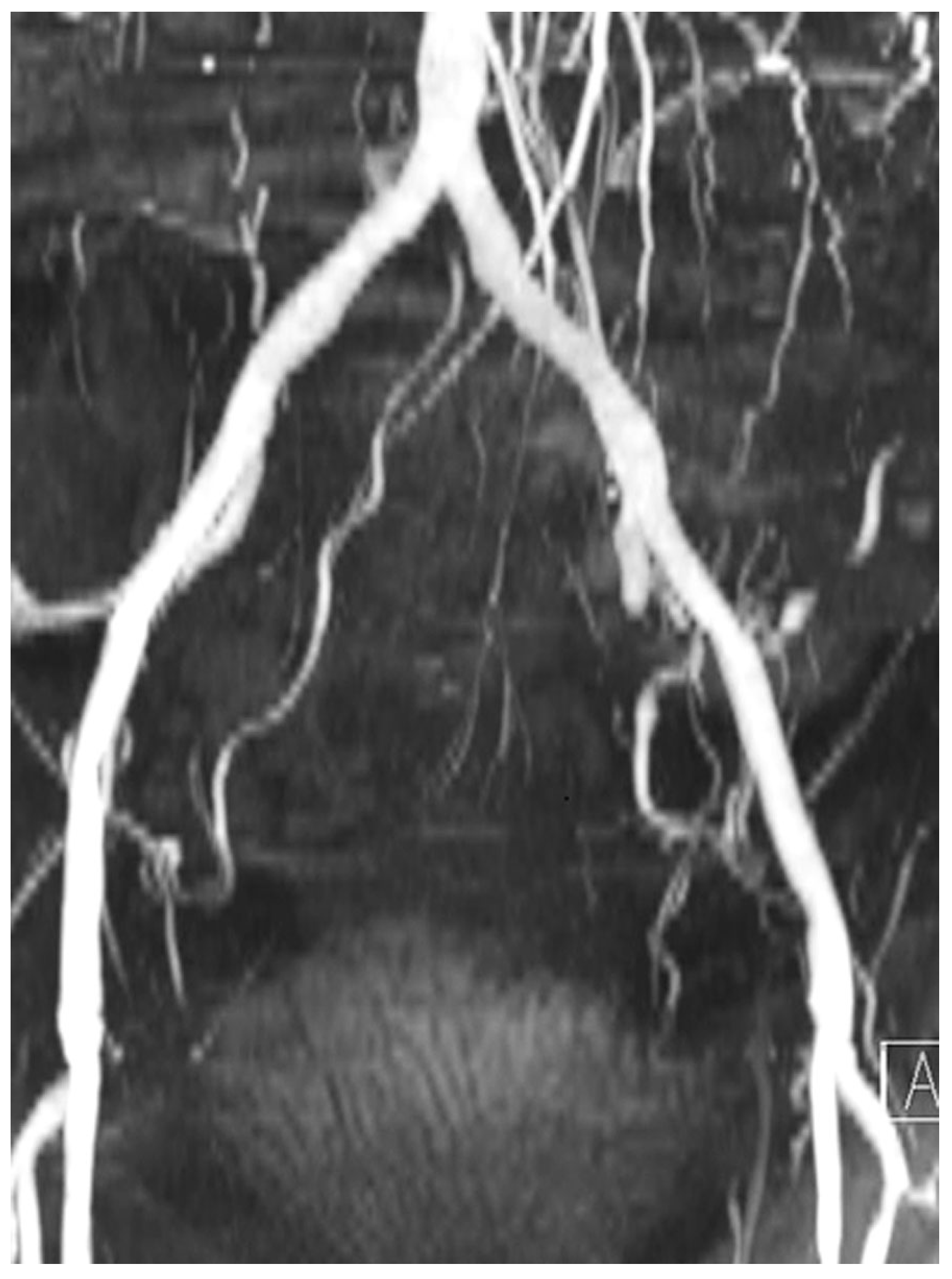
MR for valve selection
Study limitations
Conclusion
Conflicts of Interest
Abbreviations
| AKI | Acute kidney injury |
| CAD | Coronary artery disease |
| CKD | Chronic kidney disease |
| CM | Contrast medium |
| GFR | Glomerular filtration rate |
| MSCT | Multislice computer tomography |
| MR | Magnet resonance tomography |
| TAVI | Transcatheter aortic valve replacement |
| PCI | Percutaneous coronary intervention |
References
- Toggweiler, S.; Gurvitch, R.; Leipsic, J.; Wood, D.A.; Willson, A.B.; Binder, R.K.; et al. Percutaneous aortic valve replacement: vascular outcomes with a fully percutaneous procedure. J Am Coll Cardiol. 2012, 59, 113–118. [Google Scholar] [CrossRef]
- Hansen, J.W.; Foy, A.; Yadav, P.; Gilchrist, I.C.; Kozak, M.; Stebbins, A.; et al. Death and Dialysis After Transcatheter Aortic Valve Replacement: An Analysis of the STS/ACC TVT Registry. JACC Cardiovasc Interv. 2017, 10, 2064–2075. [Google Scholar] [CrossRef] [PubMed]
- Wenaweser, P.; Pilgrim, T.; Kadner, A.; Huber, C.; Stortecky, S.; Buellesfeld, L.; et al. Clinical outcomes of patients with severe aortic stenosis at increased surgical risk according to treatment modality. J Am Coll Cardiol. 2011, 58, 2151–2162. [Google Scholar] [CrossRef]
- Yamamoto, M.; Hayashida, K.; Mouillet, G.; Chevalier, B.; Meguro, K.; Watanabe, Y.; et al. Renal function-based contrast dosing predicts acute kidney injury following transcatheter aortic valve implantation. JACC Cardiovasc Interv. 2013, 6, 479–486. [Google Scholar] [CrossRef] [PubMed]
- Abdel-Wahab, M.; Mehilli, J.; Frerker, C.; Neumann, F.J.; Kurz, T.; Tölg, R.; et al.; CHOICE investigators Comparison of balloon-expandable vs self-expandable valves in patients undergoing transcatheter aortic valve replacement: the CHOICE randomized clinical trial. JAMA. 2014, 311, 1503–1514. [Google Scholar] [CrossRef] [PubMed]
- Madershahian, N.; Scherner, M.; Liakopoulos, O.; Rahmanian, P.; Kuhn, E.; Hellmich, M.; et al. Renal impairment and transapical aortic valve implantation: impact of contrast medium dose on kidney function and survival. Eur J Cardiothorac Surg. 2012, 41, 1225–1232. [Google Scholar] [CrossRef][Green Version]
- Bagur, R.; Webb, J.G.; Nietlispach, F.; Dumont, E.; De Larochellière, R.; Doyle, D.; et al. Acute kidney injury following transcatheter aortic valve implantation: predictive factors, prognostic value, and comparison with surgical aortic valve replacement. Eur Heart J. 2010, 31, 865–874. [Google Scholar] [CrossRef]
- Meneguz-Moreno, R.A.; Ramos, A.I.; Siqueira, D.; de Castro-Filho, A.; Jatene, T.; Dias Jeronimo, A.; et al. Prognostic value of renal function in patients with aortic stenosis treated with transcatheter aortic valve replacement. Catheter Cardiovasc Interv. 2017, 89, 452–459. [Google Scholar] [CrossRef]
- Achenbach, S.; Delgado, V.; Hausleiter, J.; Schoenhagen, P.; Min, J.K.; Leipsic, J.A. SCCT expert consensus document on computed tomography imaging before transcatheter aortic valve implantation (TAVI)/transcatheter aortic valve replacement (TAVR). J Cardiovasc Comput Tomogr. 2012, 6, 366–380. [Google Scholar] [CrossRef]
- Khalique, O.K.; Pulerwitz, T.C.; Halliburton, S.S.; Kodali, S.K.; Hahn, R.T.; Nazif, T.M.; et al. Practical considerations for optimizing cardiac computed tomography protocols for comprehensive acquisition prior to transcatheter aortic valve replacement. J Cardiovasc Comput Tomogr. 2016, 10, 364–374. [Google Scholar] [CrossRef]
- Thamcharoen, N.; Thongprayoon, C.; Edmonds, P.J.; Cheungpasitporn, W. Periprocedural Nebivolol for the Prevention of Contrast-Induced Acute Kidney Injury: A Systematic Review and Meta-analysis. N Am J Med Sci. 2015, 7, 446–451. [Google Scholar] [CrossRef]
- Elhmidi, Y.; Bleiziffer, S.; Deutsch, M.A.; Krane, M.; Mazzitelli, D.; Lange, R.; et al. Acute kidney injury after transcatheter aortic valve implantation: incidence, predictors and impact on mortality. Arch Cardiovasc Dis. 2014, 107, 133–139. [Google Scholar] [CrossRef]
- Wenaweser, P.; Pilgrim, T.; Guerios, E.; Stortecky, S.; Huber, C.; Khattab, A.A.; et al. Impact of coronary artery disease and percutaneous coronary intervention on outcomes in patients with severe aortic stenosis undergoing transcatheter aortic valve implantation. EuroIntervention. 2011, 7, 541–548. [Google Scholar] [CrossRef]
- Appel, C.F.; Hultkvist, H.; Nylander, E.; Ahn, H.; Nielsen, N.E.; Freter, W.; et al. Transcatheter versus surgical treatment for aortic stenosis: patient selection and early outcome. Scand Cardiovasc J. 2012, 46, 301–307. [Google Scholar] [CrossRef][Green Version]
- Najjar, M.; Salna, M.; George, I. Acute kidney injury after aortic valve replacement: incidence, risk factors and outcomes. Expert Rev Cardiovasc Ther. 2015, 13, 301–316. [Google Scholar] [CrossRef]
- Aikawa, E.; Aikawa, M.; Libby, P.; Figueiredo, J.L.; Rusanescu, G.; Iwamoto, Y.; et al. Arterial and aortic valve calcification abolished by elastolytic cathepsin S deficiency in chronic renal disease. Circulation. 2009, 119, 1785–1794. [Google Scholar] [CrossRef] [PubMed]
- Scolari, F.; Ravani, P.; Gaggi, R.; Santostefano, M.; Rollino, C.; Stabellini, N.; et al. The challenge of diagnosing atheroembolic renal disease: clinical features and prognostic factors. Circulation. 2007, 116, 298–304. [Google Scholar] [CrossRef] [PubMed]
- Vellanki, K.; Bansal, V.K. Neurologic Complications of Chronic Kidney Disease. Curr Neurol Neurosci Rep. 2015, 15, 50. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Chertow, G.M.; Fan, D.; McCulloch, C.E.; Hsu, C.Y. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. 2004, 351, 1296–1305. [Google Scholar] [CrossRef]
- Massy, Z.A.; Ivanovski, O.; Nguyen-Khoa, T.; Angulo, J.; Szumilak, D.; Mothu, N.; et al. Uremia accelerates both atherosclerosis and arterial calcification in apolipoprotein E knockout mice. J Am Soc Nephrol. 2005, 16, 109–116. [Google Scholar] [CrossRef]
- Schwarz, U.; Buzello, M.; Ritz, E.; Stein, G.; Raabe, G.; Wiest, G.; et al. Morphology of coronary atherosclerotic lesions in patients with end-stage renal failure. Nephrol Dial Transplant. 2000, 15, 218–223. [Google Scholar] [CrossRef]
- Elhmidi, Y.; Bleiziffer, S.; Piazza, N.; Hutter, A.; Opitz, A.; Hettich, I.; et al. Incidence and predictors of acute kidney injury in patients undergoing transcatheter aortic valve implantation. Am Heart J. 2011, 161, 735–739. [Google Scholar] [CrossRef]
- Nuis, R.J.; Van Mieghem, N.M.; Tzikas, A.; Piazza, N.; Otten, A.M.; Cheng, J.; et al. Frequency, determinants, and prognostic effects of acute kidney injury and red blood cell transfusion in patients undergoing transcatheter aortic valve implantation. Catheter Cardiovasc Interv. 2011, 77, 881–889. [Google Scholar] [CrossRef] [PubMed]
- Barbash, I.M.; Ben-Dor, I.; Dvir, D.; Maluenda, G.; Xue, Z.; Torguson, R.; et al. Incidence and predictors of acute kidney injury after transcatheter aortic valve replacement. Am Heart J. 2012, 163, 1031–1036. [Google Scholar] [CrossRef] [PubMed]
- Khawaja, M.Z.; Thomas, M.; Joshi, A.; Asrress, K.N.; Wilson, K.; Bolter, K.; et al. The effects of VARC-defined acute kidney injury after transcatheter aortic valve implantation (TAVI) using the Edwards bioprosthesis. EuroIntervention. 2012, 8, 563–570. [Google Scholar] [CrossRef]
- McCullough, P.A.; Wolyn, R.; Rocher, L.L.; Levin, R.N.; O’Neill, W.W. Acute renal failure after coronary intervention: incidence, risk factors, and relationship to mortality. Am J Med. 1997, 103, 368–375. [Google Scholar] [CrossRef]
- Iakovou, I.; Dangas, G.; Mehran, R.; Lansky, A.J.; Ashby, D.T.; Fahy, M.; et al. Impact of gender on the incidence and outcome of contrast-induced nephropathy after percutaneous coronary intervention. J Invasive Cardiol. 2003, 15, 18–22. [Google Scholar] [CrossRef]
- McCullough, P.A.; Adam, A.; Becker, C.R.; Davidson, C.; Lameire, N.; Stacul, F.; CIN Consensus Working Panel; et al. Risk prediction of contrast-induced nephropathy. Am J Cardiol. 2006, 98, 27K–36K. [Google Scholar] [CrossRef]
- Mehran, R.; Aymong, E.D.; Nikolsky, E.; Lasic, Z.; Iakovou, I.; Fahy, M.; et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: development and initial validation. J Am Coll Cardiol. 2004, 44, 1393–1399. [Google Scholar] [CrossRef] [PubMed]
- Rihal, C.S.; Textor, S.C.; Grill, D.E.; Berger, P.B.; Ting, H.H.; Best, P.J.; et al. Incidence and prognostic importance of acute renal failure after percutaneous coronary intervention. Circulation. 2002, 105, 2259–2264. [Google Scholar] [CrossRef]
- Wöhrle, J.; Gonska, B.; Rodewald, C.; Trepte, U.; Koch, S.; Scharnbeck, D.; et al. Transfemoral aortic valve implantation with the repositionable Lotus valve compared with the balloon-expandable Edwards Sapien 3 valve. Int J Cardiol. [CrossRef]
- Willson, A.B.; Webb, J.G.; Labounty, T.M.; Achenbach, S.; Moss, R.; Wheeler, M.; et al. 3-dimensional aortic annular assessment by multidetector computed tomography predicts moderate or severe paravalvular regurgitation after transcatheter aortic valve replacement: a multicenter retrospective analysis. J Am Coll Cardiol. 2012, 59, 1287–1294. [Google Scholar] [CrossRef] [PubMed]
- Bernhardt, P.; Rodewald, C.; Seeger, J.; Gonska, B.; Buckert, D.; Radermacher, M.; et al. Non-contrast-enhanced magnetic resonance angiography is equal to contrast-enhanced multislice computed tomography for correct aortic sizing before transcatheter aortic valve implantation. Clin Res Cardiol. 2016, 105, 273–278. [Google Scholar] [CrossRef] [PubMed]
- Arrigo, M.; Maisano, F.; Haueis, S.; Binder, R.K.; Taramasso, M.; Nietlispach, F. Transcatheter aortic-valve implantation with one single minimal contrast media injection. Catheter Cardiovasc Interv. 2015, 85, 1248–1253. [Google Scholar] [CrossRef] [PubMed]
- Pulerwitz, T.C.; Khalique, O.K.; Nazif, T.N.; Rozenshtein, A.; Pearson, G.D.; Hahn, R.T.; et al. Very low intravenous contrast volume protocol for computed tomography angiography providing comprehensive cardiac and vascular assessment prior to transcatheter aortic valve replacement in patients with chronic kidney disease. J Cardiovasc Comput Tomogr. 2016, 10, 316–321. [Google Scholar] [CrossRef]
- Kappetein, A.P.; Head, S.J.; Généreux, P.; Piazza, N.; van Mieghem, N.M.; Blackstone, E.H.; et al. Updated standardized endpoint definitions for transcatheter aortic valve implantation: the Valve Academic Research Consortium-2 consensus document. J Am Coll Cardiol. 2012, 60, 1438–1454. [Google Scholar] [CrossRef]
| Magnet resonance tomography without gadolinium instead of multislice computed tomography |
| Coronary angiography with 3-4 views |
| Prehydration with 500 ml of saline 0.9% |
| Transcatheter aortic valve replacement under conscious sedation |
| Rapid pacing for determination of implant view |
| Transthoracic echocardiography to assess paravalvular regurgitation |
| Careful postprocedural monitoring and care |
| All patients (n =168) | Patients with severe CKD (n = 20) | Patients without severe CKD (n = 148) | p value | ||
| Age, years | 81 ± 6 | 84 ± 6 | 81 ± 6 | 0.05 | |
| Female sex | 92 (55%) | 13 (65%) | 79 (53%) | 0.35 | |
| Hypertension | 142 (85%) | 17 (85%) | 125 (84%) | 1.0 | |
| Diabetes | 30 (18%) | 4 (20%) | 26 (18%) | 0.76 | |
| Coronary artery disease | 83 (49%) | 9 (45%) | 74 (50%) | 0.81 | |
| Prior stroke | 19 (11%) | 1 (5%) | 18 (12%) | 0.48 | |
| STS PROM, % | 4.3 ± 3.7 | 8.2 ± 4.0 | 3.8 ± 3.4 | <0.01 | |
| Echocardiographic parameters | Aortic valve area, cm2 | 0.76 ± 0.19 | 0.7 ± 0.22 | 0.77 ± 0.19 | 0.16 |
| Mean gradient, mmHg | 47 ± 17 | 45 ± 13 | 48 ± 18 | 0.52 | |
| Left ventricular ejection fraction, % | 59 ± 13 | 51 ± 15 | 58 ± 13 | 0.03 | |
| Laboratory parameters | Creatinine (µmol/L) | 107 ± 56 | 198 ± 62 | 94 ± 42 | <0.01 |
| GFR (ml/min) | 54 ± 24 | 24 ± 5 | 58 ± 23 | <0.01 | |
| Implanted valve | Acurate neo | 106 (63%) | 14 (70%) | 92 (62%) | 0.95 |
| Sapien 3 | 49 (29%) | 5 (25%) | 44 (30%) | ||
| Evolut R | 10 (6%) | 1 (5%) | 9 (7%) | ||
| Allegra | 3 (2%) | 0 (0%) | 3 (2%) | ||
| All patients (n = 168) | Patients with severe CKD (n = 20) | Patients without severe CKD (n = 148) | p value | ||
| Aortic valve area, cm2 | 2.1 ± 0.5 | 2.1 ± 0.5 | 2.1 ± 0.5 | 0.64 | |
| Mean gradient, mmHg | 6.8 ± 3.6 | 5.5 ± 3.3 | 6.9 ± 3.7 | 0.12 | |
| Paravalvular regurgitation | none/trace | 103 (64%) | 12 (60%) | 91 (64%) | 0.85 |
| mild | 57 (35%) | 8 (40%) | 49 (35%) | ||
| moderate | 2 (1.2%) | 0 (0%) | 2 (1.4%) | ||
| Acute kidney injury stage 2 or 3 | 5 (3.0%) | 1 (5.0%) | 4 (2.7%) | 0.054 | |
| All patients (n = 168) | Patients with severe CKD (n = 20) | Patients without severe CKD (n = 148) | p value | |
| All-cause mortality | 3 (1.8%) | 0 (0%) | 3 (2.0%) | 0.68 |
| Device success | 159 (96.4%) | 20 (100%) | 139 (95.9%) | 1.0 |
| Early safety | 150 (91%) | 18 (90%) | 132 (91%) | 1.0 |
| Clinical efficacy | 156 (95.1%) | 20 (100%) | 136 (94.4%) | 0.6 |
| Any stroke | 0 (0%) | 0 (0%) | 0 (0%) | N/A |
| New permanent pacemaker | 6 (3.6%) | 2 (10%) | 4 (2.7%) | 0.15 |
| Major vascular complication | 11 (6.6%) | 1 (5%) | 10 (6.8%) | 1.0 |
| Major or life-threatening bleeding | 12 (7.1%) | 1 (5%) | 11 (7.4%) | 1.0 |
© 2019 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Brinkert, M.; de Boeck, B.; Petryka, J.; Buhmann, R.; Fornaro, J.; Weberndörfer, V.; Bossard, M.; Roos, J.; Cuculi, F.; Kobza, R.; et al. Minimal Use of Contrast Media in Patients with Severe Chronic Kidney Disease Undergoing Transcatheter Aortic Valve Implantation. Cardiovasc. Med. 2019, 22, w02021. https://doi.org/10.4414/cvm.2019.02021
Brinkert M, de Boeck B, Petryka J, Buhmann R, Fornaro J, Weberndörfer V, Bossard M, Roos J, Cuculi F, Kobza R, et al. Minimal Use of Contrast Media in Patients with Severe Chronic Kidney Disease Undergoing Transcatheter Aortic Valve Implantation. Cardiovascular Medicine. 2019; 22(1):w02021. https://doi.org/10.4414/cvm.2019.02021
Chicago/Turabian StyleBrinkert, Miriam, Bart de Boeck, Joanna Petryka, Ralf Buhmann, Jürgen Fornaro, Vanessa Weberndörfer, Matthias Bossard, Justus Roos, Florim Cuculi, Richard Kobza, and et al. 2019. "Minimal Use of Contrast Media in Patients with Severe Chronic Kidney Disease Undergoing Transcatheter Aortic Valve Implantation" Cardiovascular Medicine 22, no. 1: w02021. https://doi.org/10.4414/cvm.2019.02021
APA StyleBrinkert, M., de Boeck, B., Petryka, J., Buhmann, R., Fornaro, J., Weberndörfer, V., Bossard, M., Roos, J., Cuculi, F., Kobza, R., & Toggweiler, S. (2019). Minimal Use of Contrast Media in Patients with Severe Chronic Kidney Disease Undergoing Transcatheter Aortic Valve Implantation. Cardiovascular Medicine, 22(1), w02021. https://doi.org/10.4414/cvm.2019.02021




