Patients admitted with bradycardia may present with a variety of clinical pictures, ranging from fatigue to syncope and cardiac arrest. It is important to be able to identify the mechanism of bradycardia in order to distinguish benign from life-threatening situations.
In general, sinus bradycardia or arrest, as well as atrioventricular block (AVB) at the nodal level, have a benign prognosis. Infranodal block (bundle of His or bundle branches) may lead to prolonged asystole without an escape rhythm. Proper clinical evaluation will lead to appropriate therapeutic measures, whereas mismanagement may have a fatal outcome.
Clinical evaluation
Obviously, not all documented bradycardia needs treatment and, conversely, undocumented but suspected bradycardia may need backup measures to avoid asystole. Overall, therapy for bradycardia aims to (1) avoid asystole, (2) improve haemodynamic status, or (3) avoid tachycardia (e.g., in the setting of a prolonged QT interval with torsades de pointes). Management strategies for bradycardia depend upon a number of factors, listed below:
- –
- Presence, duration and gravity of symptoms (for how long has the patient been symptomatic? Was there syncope? If yes, did it result in trauma?)
- –
- Vital signs
- –
- Systemic repercussions of bradycardia and a lowoutput state (renal function, lactate, etc.)
- –
- Type of bradycardia (sinus, AVB II Wenckebach vs Mobitz 2, AVB III)
- –
- Presence or absence of a documented escape rhythm
- –
- Effect of pharmacological treatment (isoprenaline, atropine)
- –
- Anticipated duration of the bradycardia
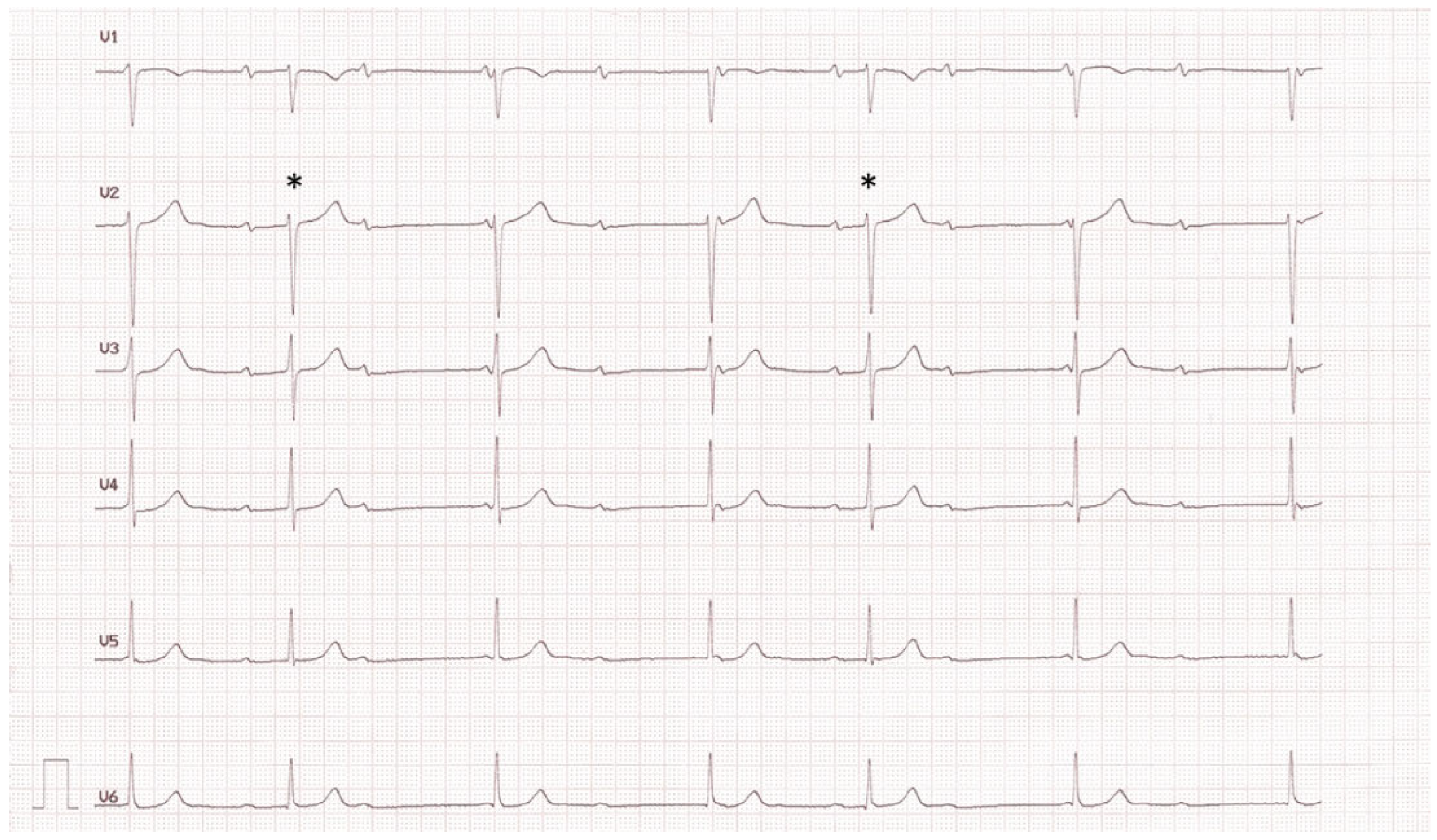
Nodal AVB can be distinguished from infranodal AVB by careful analysis of the electrocardiogram and by diagnostic bedside manoeuvres (Table 1). AVB III may occur at both nodal as well as infranodal levels, although the latter is more frequent. High-grade AVB is defined as ≥3:1 AVB. A common mistake is to misdiagnose AVB III by failing to recognise conducted P waves (Figure 1).

Table 1.
Clues to help distinguish nodal from infranodal atrioventricular block.
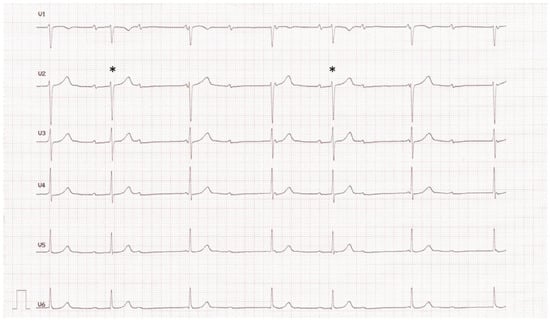
Figure 1.
Patient with misdiagnosis of AVB III. Note the presence of conducted beats (asterisks), alternating with AVB II and junctional escape rhythm (the short PR intervals preceding the third and sixth QRS complexes are too short to have conducted).
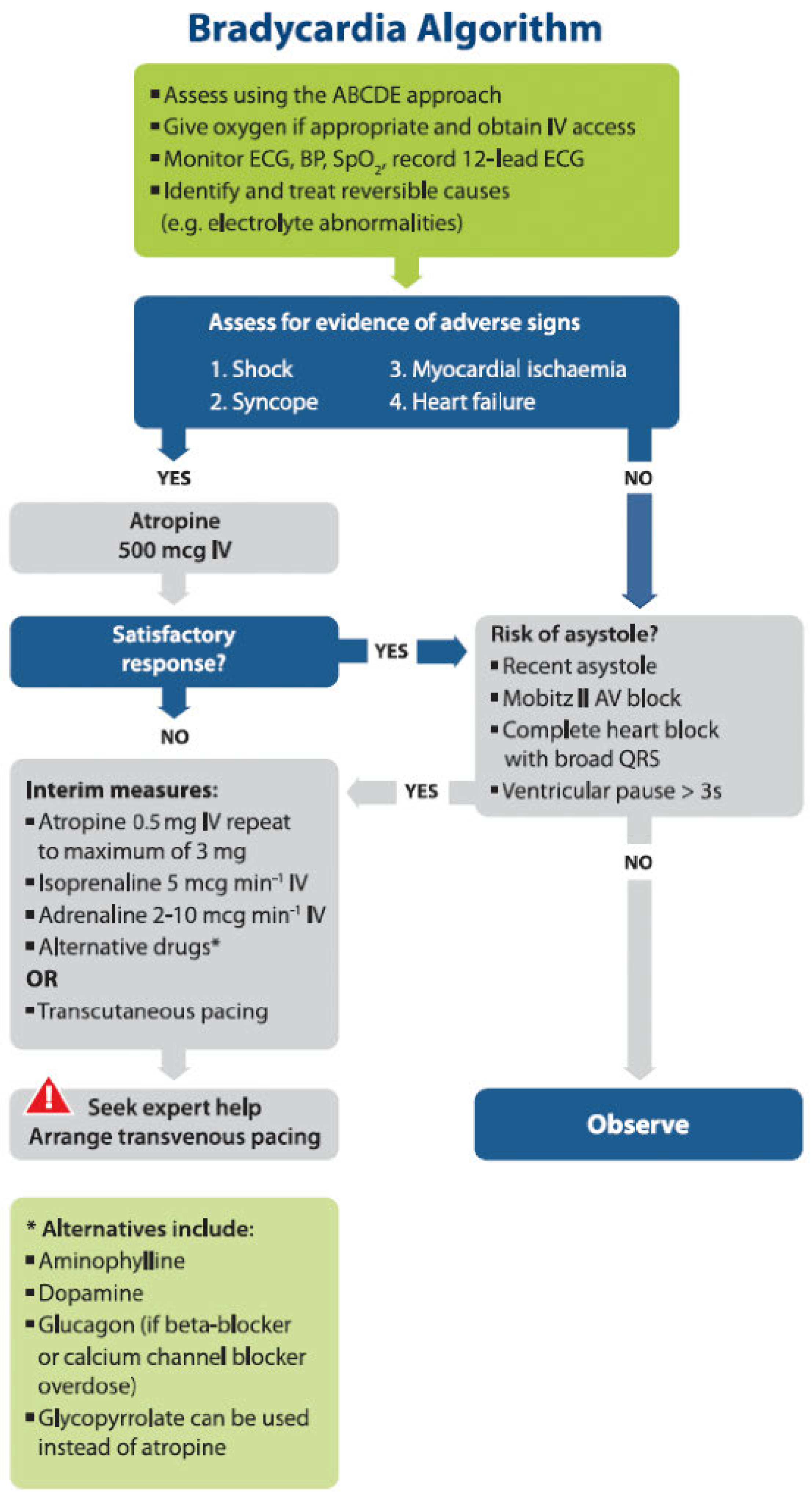
In 2015, the European Resuscitation Council published guidelines on advanced life support [1], which include an algorithm for the acute management of bradycardia (Figure 2).
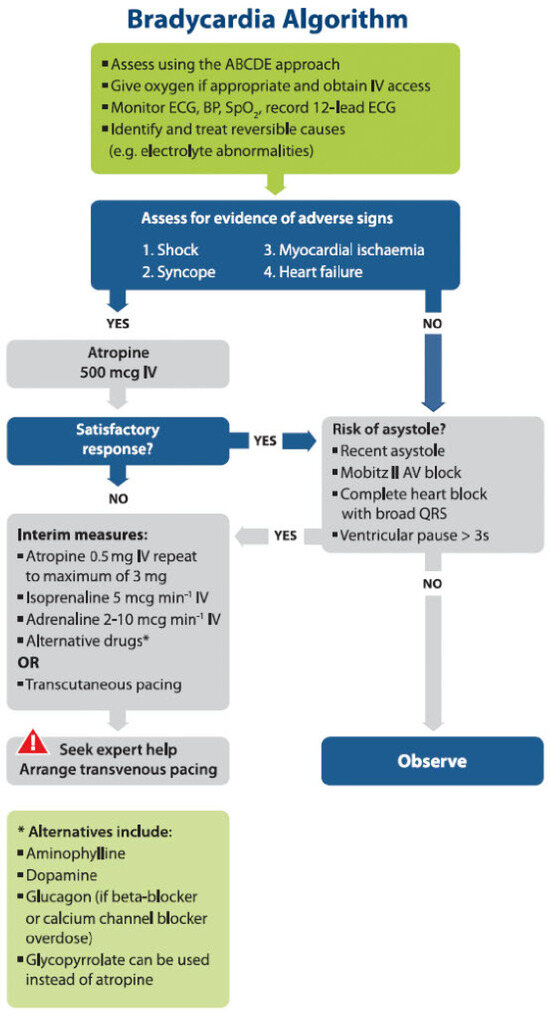
Figure 2.
Management of acute bradycardia according to the 2015 European Resuscitation Council guidelines [1].
Pharmacological therapy
Pharmacological therapy is most often the first line of treatment for bradycardia because it is the most readily available. A list of the drugs used is shown in Table 2. It should be noted that drugs that increase sinus rate may worsen infranodal block. However, in the case of infranodal AVB III, heart rate may increase with infusion of catecholamines (e.g., isoprenaline) owing to acceleration of the automatic escape rhythm, and may therefore be of therapeutic interest despite lack of improvement in AV conduction. Pharmacological treatment for bradycardia due to drug toxicity is summarised in Table 3.

Table 2.
Drugs used to increase heart rate.

Table 3.
Specific treatment options for bradycardia due to drug toxicity.
Transcutaneous pacing
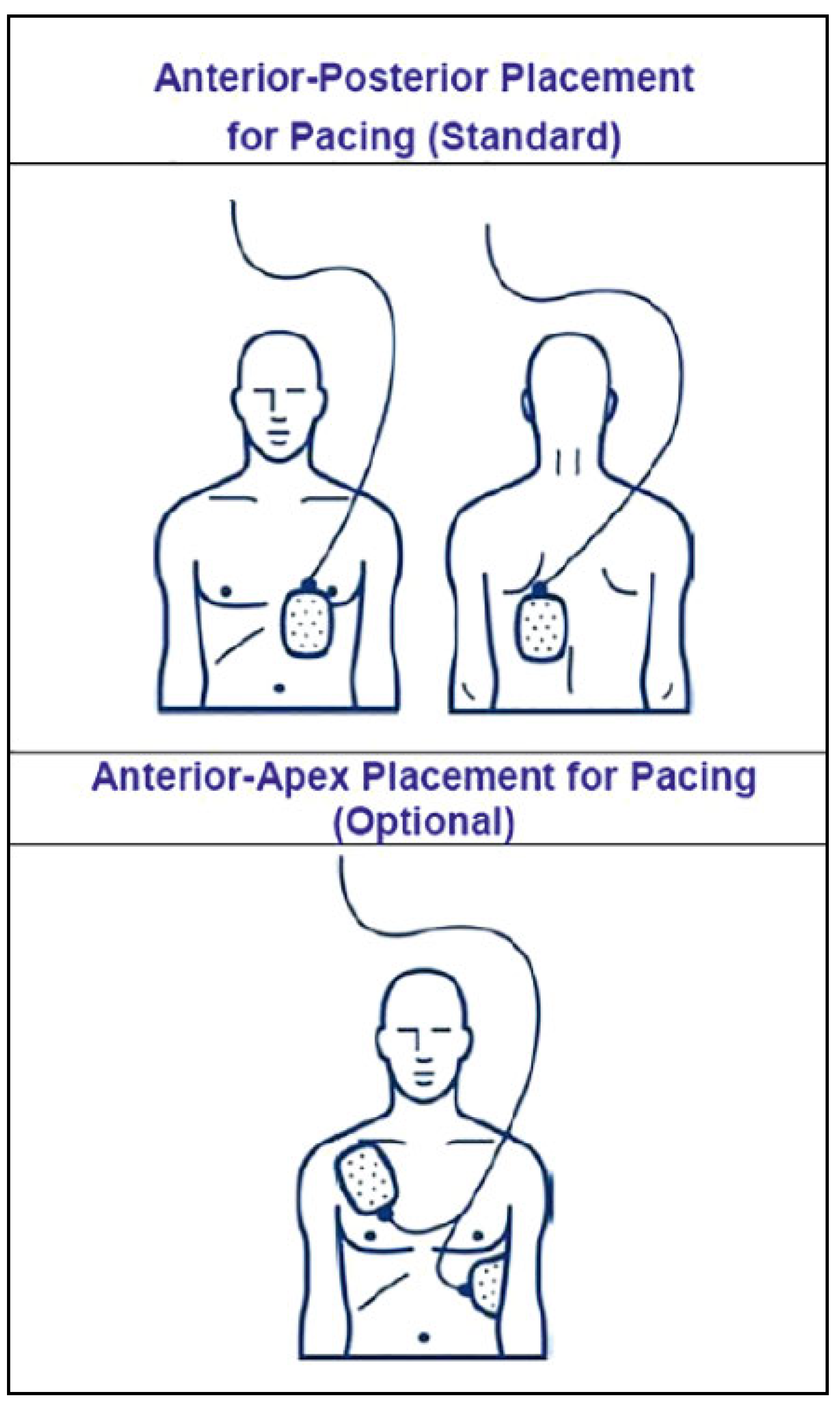
This modality is readily available, usually effective (if properly delivered), but underused in clinical practice because of reluctance to cause discomfort to the patient. It is suitable as an emergency life-saving measure, or as a backup for infrequent pacing (e.g., paroxysmal AV block, transient sinus asystole following cardioversion of atrial fibrillation, etc.). It is delivered using external defibrillators, but not all models offer this option. Pacing output can usually be set between 20–180 mA. It is important to place the patches in an anteroposterior position (Figure 3), ideally over bony surfaces (pain being caused by skeletal muscle contraction). The pads should not be repositioned, as they may lose conductive gel and adhere less well.
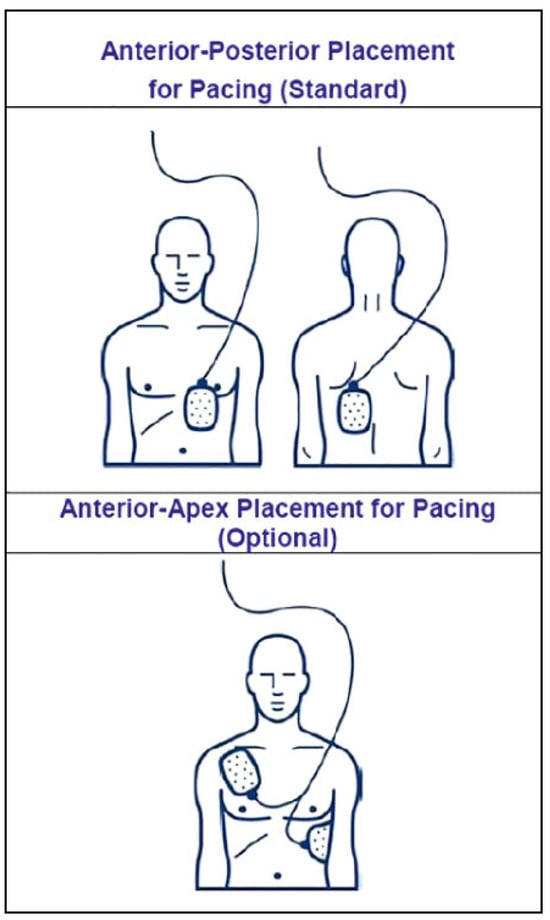
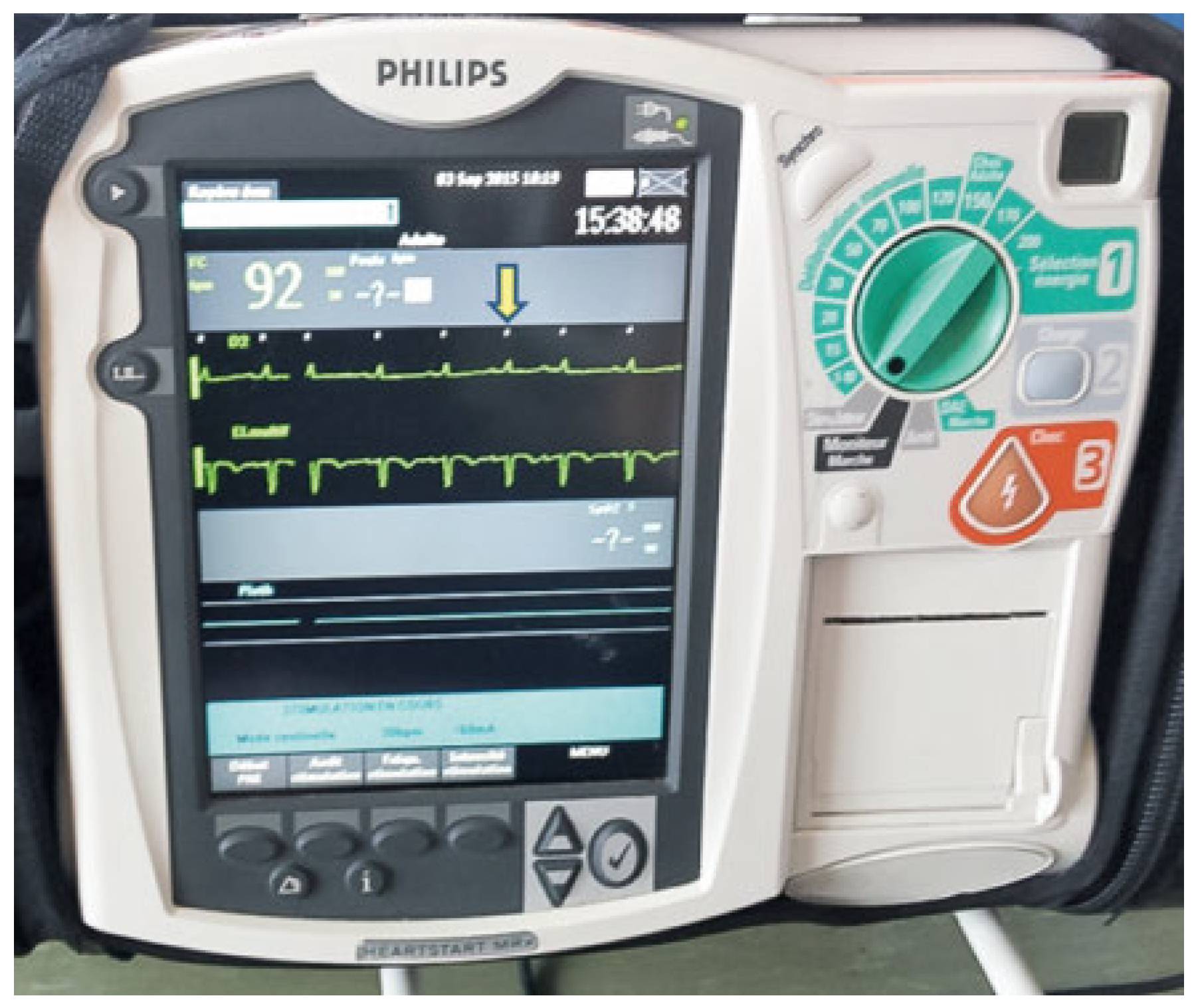
Figure 3.
Placement of defibrillator patches for transcutaneous pacing.
In a conscious patient, the initial output may be set at, for example, 80 mA. In an unconscious patient, output may be programmed to the maximal value, and then down-titrated as appropriate. In a pre-hospital setting in 32 patients, average capture thresholds were 64 ± 33 mA [2].
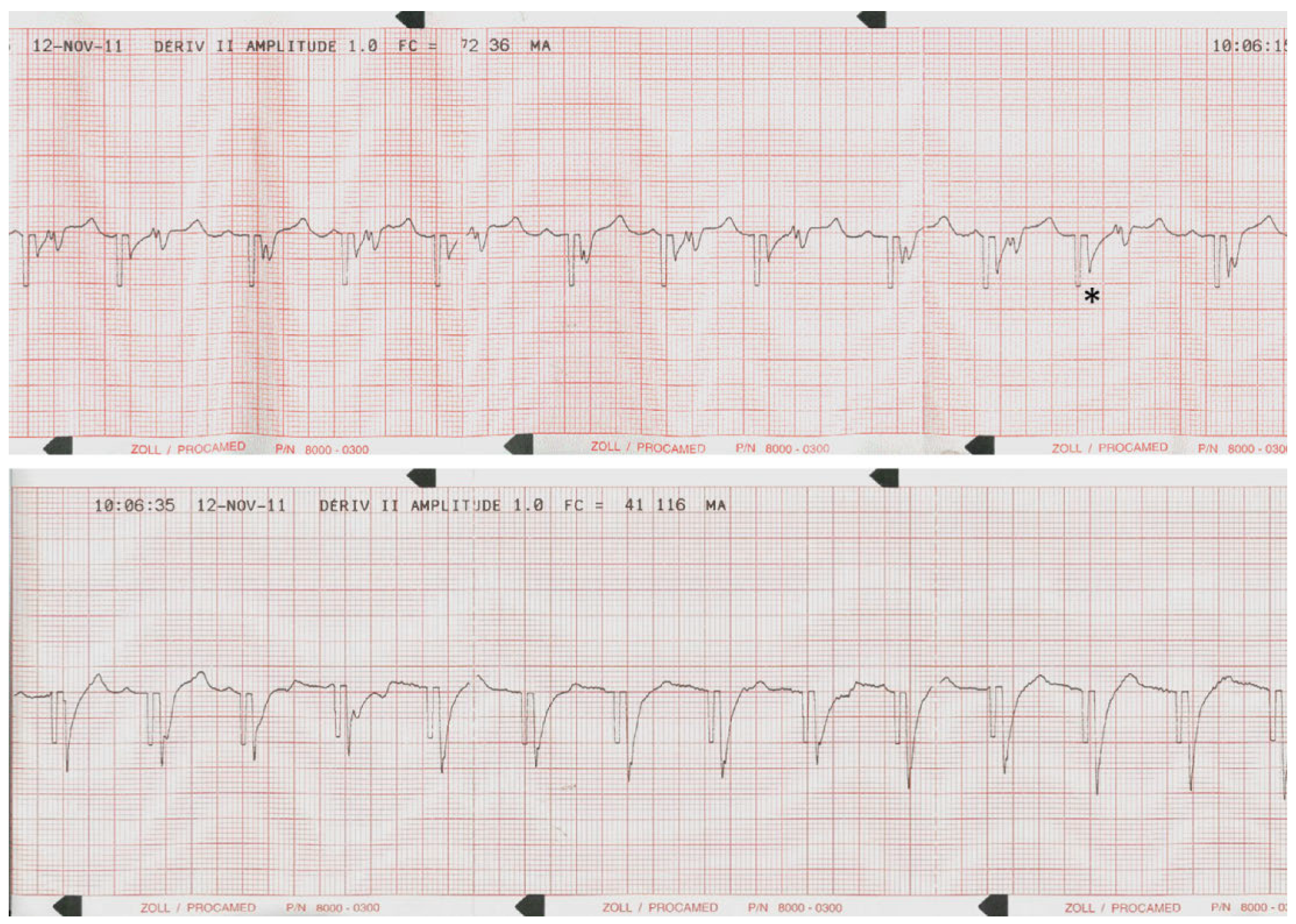
Presence of ventricular capture should be verified by evaluating the patient’s pulse either manually or using an oximeter (Figure 4), as the ECG may be deceptive or difficult to analyse (Figure 4 and Figure 5). Obviously, pectoral muscle contraction does not indicate myocardial capture! It is important to verify adequate sensing by checking that sensing markers are properly aligned with each intrinsic QRS complex (Figure 6).

Figure 4.
Emergency transcutaneous pacing administered to a patient admitted for complete atrioventricular block with asystole, who was immediately transferred to the operating room for permanent pacemaker implantation. Left: Transcutaneous pacing was effective at 160 mA output, despite suboptimal placement of the patches (which were not repositioned as the patient was pacemaker-dependant). Right: Monitor screen with an uninterpretable ECG, but finger oximetry showing an effective pulse at the paced rate of 40 bpm.
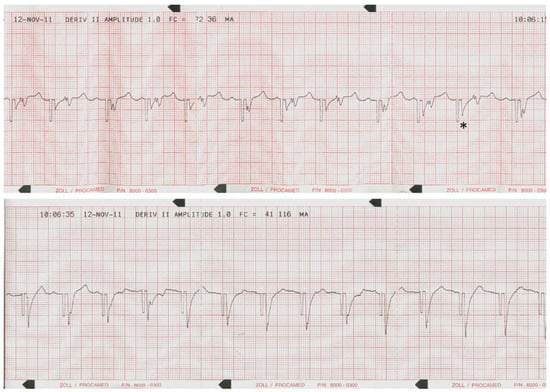
Figure 5.
ECG analysis of ventricular capture by transcutaneous pacing in an obese patient with paroxysmal AV block, in whom it was deemed appropriate to test efficacy of backup pacing . Top: lack of myocardial capture, with presence of intrinsic P and QRS complexes. The pacing afterpotential (*) may be mistaken for a QRS complex. Bottom: Increase in pacing output with presence of capture, which can be identified by the presence of T waves, as the QRS complexes are masked by the pacing afterpotentials.
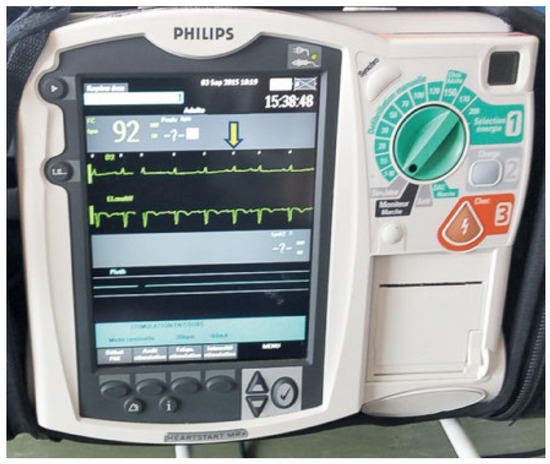
Figure 6.
Adequate sensing of QRS complexes by the external defibrillator set to backup pacing at 30 bpm. The sensing markers are indicated on the screen by the white ticks (yellow arrow). Note the absence of undersensing (all QRS complexes are sensed) or oversensing (absence of ticks between QRS complexes).
In the event of undersensing, unnecessary pacing may be delivered (which may be potentially pro-arrhythmic if it falls on a T wave).
In the case of oversensing (e.g., of artefacts), pacing may not be delivered (even in the case of asystole). As sensitivity levels usually cannot be modified, a different lead vector needs to be chosen if there are sensing issues. As the external defibrillator may rely on cable electrodes for sensing, these should be properly fastened (if necessary secured by tape).
The backup pacing rate is usually set to a low value (e.g., 30 bpm) to avoid unnecessary pacing, and should be set with an output that is likely to result in capture e.g., 160 mA).
If transcutaneous pacing is expected to be ineffective (e.g., in an obese patient), it is wise to test capture first (see Figure 5). If necessary, patients may be sedated with analgesia.
Transoesophaeal pacing
This modality has been abandoned at our institution. A pacing wire is inserted into the oesophagus via the nose in order to pace the left atrium (which lies just anteriorly).
This modality is therefore not suitable for pacing in cases of AV block, and also provides inconsistent capture.
Transvenous pacing
Temporary transvenous pacing doubles the risk of subsequent permanent pacemaker infection [3], and is associated with a risk of serious complications such as perforation and tamponade.
According to the 2013 European Society of Cardiology (ESC) guidelines on pacing [4], temporary transvenous pacing should be used “only as a last resort when chronotropic drugs (e.g., isoproterenol, epinephrine, etc) are insufficient” and “should be limited to cases of (i) high-degree AV block without escape rhythm, (ii) life-threatening bradyarrhythmias, such as those that occur during interventional procedures (e.g., during percutaneous coronary intervention, etc) or, rarely, in acute settings such as acute myocardial infarction, drug toxicity or concomitant systemic infection.”
The 2015 ESC guidelines on prevention of sudden death are equally restrictive on use of temporary transvenous pacing [5].
Venous access is most often obtained via the femoral vein, although it is also possible to place pacing wires via the internal jugular or subclavian vein (the latter may, however, compromise future permanent pacemaker implantation because of sterility or thrombotic issues). Pacing from the femoral vein requires the patient to stay lying and relatively immobile, as there is a risk of lead dislodgment. It is therefore unsuitable for agitated patients.
Temporary pacing wires are sized from 4–6 F. Thinner wires are less traumatic but less stable, whereas thicker wires carry a higher risk of perforation (Figure 7). Some wires have inflatable balloons just behind the tip designed to facilitate placement of the wires in the right ventricle (e.g., if fluoroscopy is not available). The balloon, if left inflated, may protect the patient from perforation by the lead (but stability needs to be verified under fluoroscopy). Temporary pacing of the atrium, although feasible, is rarely used because stability is a major issue. There are sparse data in the literature on complications associated with temporary pacing. Dislodgment is a frequent issue, therefore sensing and capture thresholds need to be checked periodically (at least daily), with continuous rhythm monitoring. Perforation and tamponade may occur at any time after placement, and sometimes become manifest only after the temporary lead is withdrawn. Another issue is inadvertent placement of the lead via a patent foramen ovale into the left ventricle, with the risk of stroke (see Figure 7).
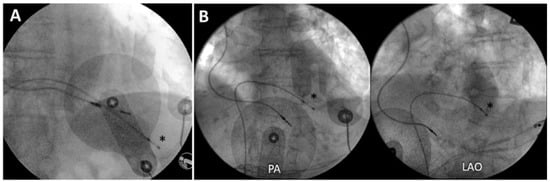
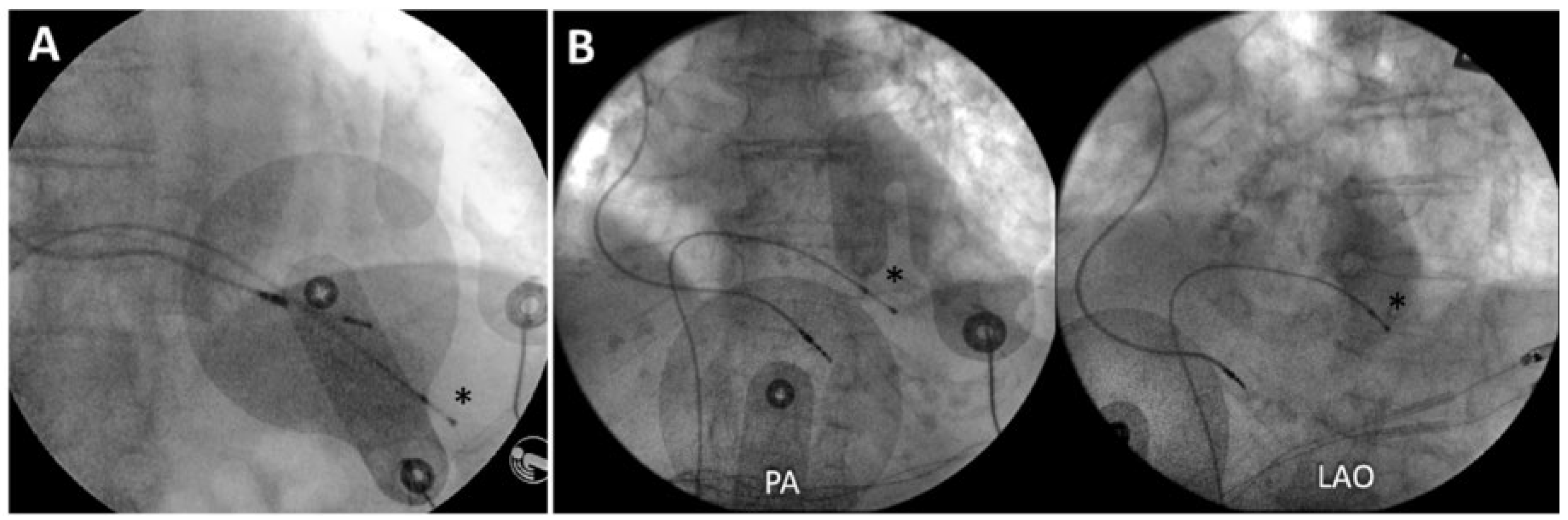
Figure 7.
Complications of temporary pacing wires in two patients. Left: Perforation of the temporary lead. Right: Inadvertent placement in the left ventricle via a patent foramen ovale. In both cases, the permanent pacing lead is implanted in the right ventricular apex (the temporary wires are indicated by an asterisk).
When temporary pacing is required for more than a few days or in the atrium, a standard pacemaker screw-in lead may be implanted via the internal jugular vein and connected to a recycled pacemaker (Figure 8). This allows pacing for up to 6 weeks [6] or more, allows mobilisation (and in selected cases even temporary discharge) of the patient, provides reliable pacing and sensing, and has a lesser risk of perforation than with temporary wires (which are stiffer).

Figure 8.
Pacemaker-dependant patient explanted for infection, with temporary pacing for 2 weeks with a standard pacemaker lead implanted via the internal jugular vein and connected to a recycled generator.
Conclusions
Bradycardia is a frequently encountered issue in the emergency setting, and is a potential cause of mortality if inappropriately managed. Identification of high risk patients requires careful clinical evaluation and electrocardiographic analysis. Importantly, localisation of the site of AV block through ECG analysis and provocative manoeuvres allows delivery of appropriate therapy. Therapeutic strategies for persistent or suspected bradycardia in the emergency setting include pharmacological measures as well as temporary pacing, either transcutaneous or transvenous. Emergency medical teams should be well trained in the delivery of these therapies, as they may be life saving.
Disclosure statement
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Soar, J.; Nolan, J.P.; Bottiger, B.W.; Perkins, G.D.; Lott, C.; Carli, P.; et al. European Resuscitation Council Guidelines for Resuscitation 2015: Section 3. Adult advanced life support. Resuscitation 2015, 95, 100–147. [Google Scholar] [CrossRef] [PubMed]
- Morrison, L.J.; Long, J.; Vermeulen, M.; Schwartz, B.; Sawadsky, B.; Frank, J.; et al. A randomized controlled feasibility trial comparing safety and effectiveness of prehospital pacing versus conventional treatment: ‘PrePACE’. Resuscitation 2008, 76, 341–349. [Google Scholar] [CrossRef] [PubMed]
- Polyzos, K.A.; Konstantelias, A.A.; Falagas, M.E. Risk factors for cardiac implantable electronic device infection: A systematic review and meta analysis. Europace 2015, 17, 767–777. [Google Scholar] [CrossRef] [PubMed]
- Brignole, M.; Auricchio, A.; Baron Esquivias, G.; Bordachar, P.; Boriani, G.; Breithardt, O.A.; et al. 2013 ESC guidelines on cardiac pacing and cardiac resynchronization therapy: The task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 2013, 15, 1070–1118. [Google Scholar]
- Priori, S.G.; Blomstrom Lundqvist, C.; Mazzanti, A.; Blom, N.; Borggrefe, M.; Camm, J.; et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC). Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J 2015, 36, 2793–2867. [Google Scholar] [PubMed]
- Kawata, H.; Pretorius, V.; Phan, H.; Mulpuru, S.; Gadiyaram, V.; Patel, J.; et al. Utility and safety of temporary pacing using active fixation leads and externalized re usable permanent pacemakers after lead extraction. Europace 2013, 15, 1287–1291. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.