Incomplete Stent Apposition Resolves One Year After Implantation
Abstract
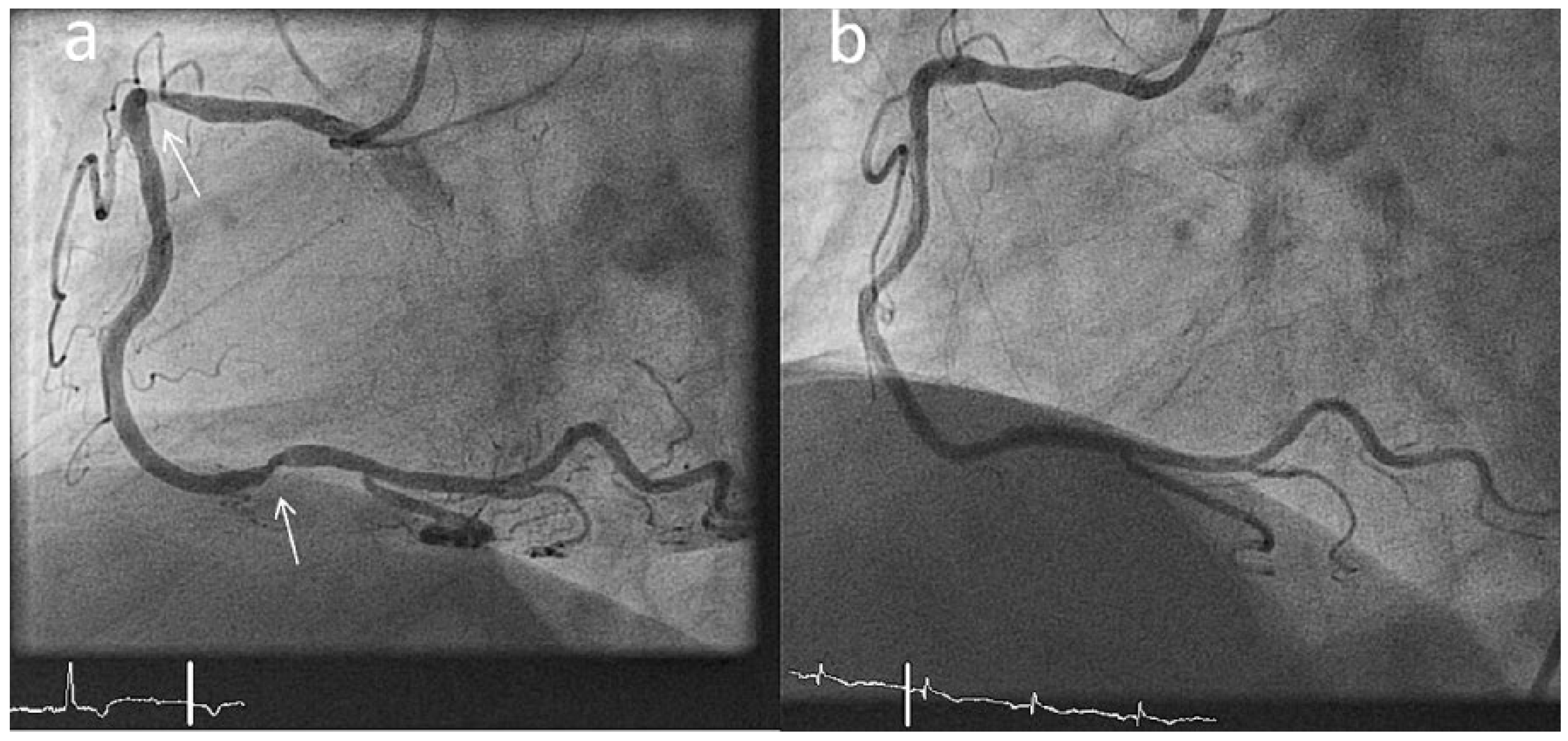
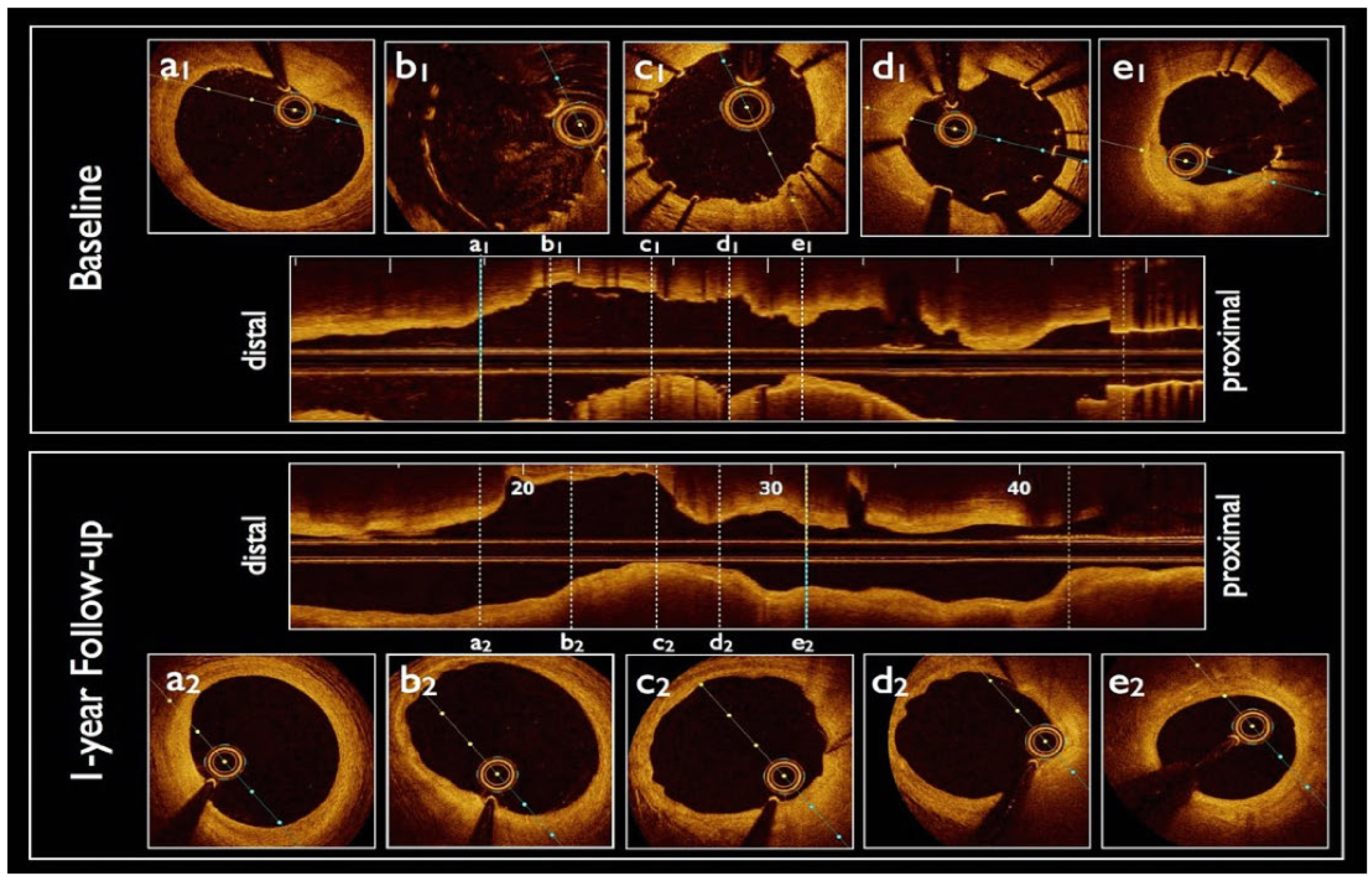
Case report
Discussion
Disclosure Statement
References
- Lindsey, J.B.; Marso, S.P. Incomplete stent apposition: Should we appose or oppose? JACC Cardiovasc Interv. 2010, 3, 495–497. [Google Scholar] [CrossRef] [PubMed]
- Foin, N.; Gutiérrez-Chico, J.L.; Nakatani, S.; Torii, R.; Bourantas, C.V.; Sen, S.; et al. Incomplete stent apposition causes high shear flow disturbances and delay in neointimal coverage as a function of strut to wall detachment distance: Implications for the management of incomplete stent apposition. Circ Cardiovasc Interv. 2014, 7, 180–9. [Google Scholar] [CrossRef] [PubMed]
- Gomez-Lara, J.; Radu, M.; Brugaletta, S.; Farooq, V.; Diletti, R.; Onuma, Y.; et al. Serial analysis of the malapposed and uncovered struts of the new generation of everolimus-eluting bioresorbable scaffold with optical coherence tomography. JACC Cardiovasc Interv. 2011, 4, 992–1001. [Google Scholar] [CrossRef] [PubMed]
- Cook, S.; Wenaweser, P.; Togni, M.; Billinger, M.; Morger, C.; Seiler, C.; et al. Incomplete stent apposition and very late stent thrombosis after drug-eluting stent implantation. Circulation. 2007, 115, 2426–2434. [Google Scholar] [CrossRef] [PubMed]
- Onuma, Y.; Serruys, P.W. Rather Thick, Yet Antithrombogenic: Is the Magmaris Scaffold a New Hope for Bioresorbable Coronary Scaffold? Circ Cardiovasc Interv. 2017, 10. [Google Scholar] [CrossRef] [PubMed]
- Puricel, S.; Cuculi, F.; Weissner, M.; Schmermund, A.; Jamshidi, P.; Nyffenegger, T.; et al. Bioresorbable Coronary Scaffold Thrombosis: Multicenter Comprehensive Analysis of Clinical Presentation, Mechanisms, and Predictors. J Am Coll Cardiol. 2016, 67, 921–931. [Google Scholar] [CrossRef] [PubMed]
© 2017 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Stierlin, F.B.; Cook, S.; Stadelmann, M. Incomplete Stent Apposition Resolves One Year After Implantation. Cardiovasc. Med. 2017, 20, 216. https://doi.org/10.4414/cvm.2017.00515
Stierlin FB, Cook S, Stadelmann M. Incomplete Stent Apposition Resolves One Year After Implantation. Cardiovascular Medicine. 2017; 20(9):216. https://doi.org/10.4414/cvm.2017.00515
Chicago/Turabian StyleStierlin, Florian Basile, Stéphane Cook, and Mathieu Stadelmann. 2017. "Incomplete Stent Apposition Resolves One Year After Implantation" Cardiovascular Medicine 20, no. 9: 216. https://doi.org/10.4414/cvm.2017.00515
APA StyleStierlin, F. B., Cook, S., & Stadelmann, M. (2017). Incomplete Stent Apposition Resolves One Year After Implantation. Cardiovascular Medicine, 20(9), 216. https://doi.org/10.4414/cvm.2017.00515



