The Diagnostic Dilemma of Myocardial Infarction with Unobstructed Coronary Arteries
Abstract
Introduction
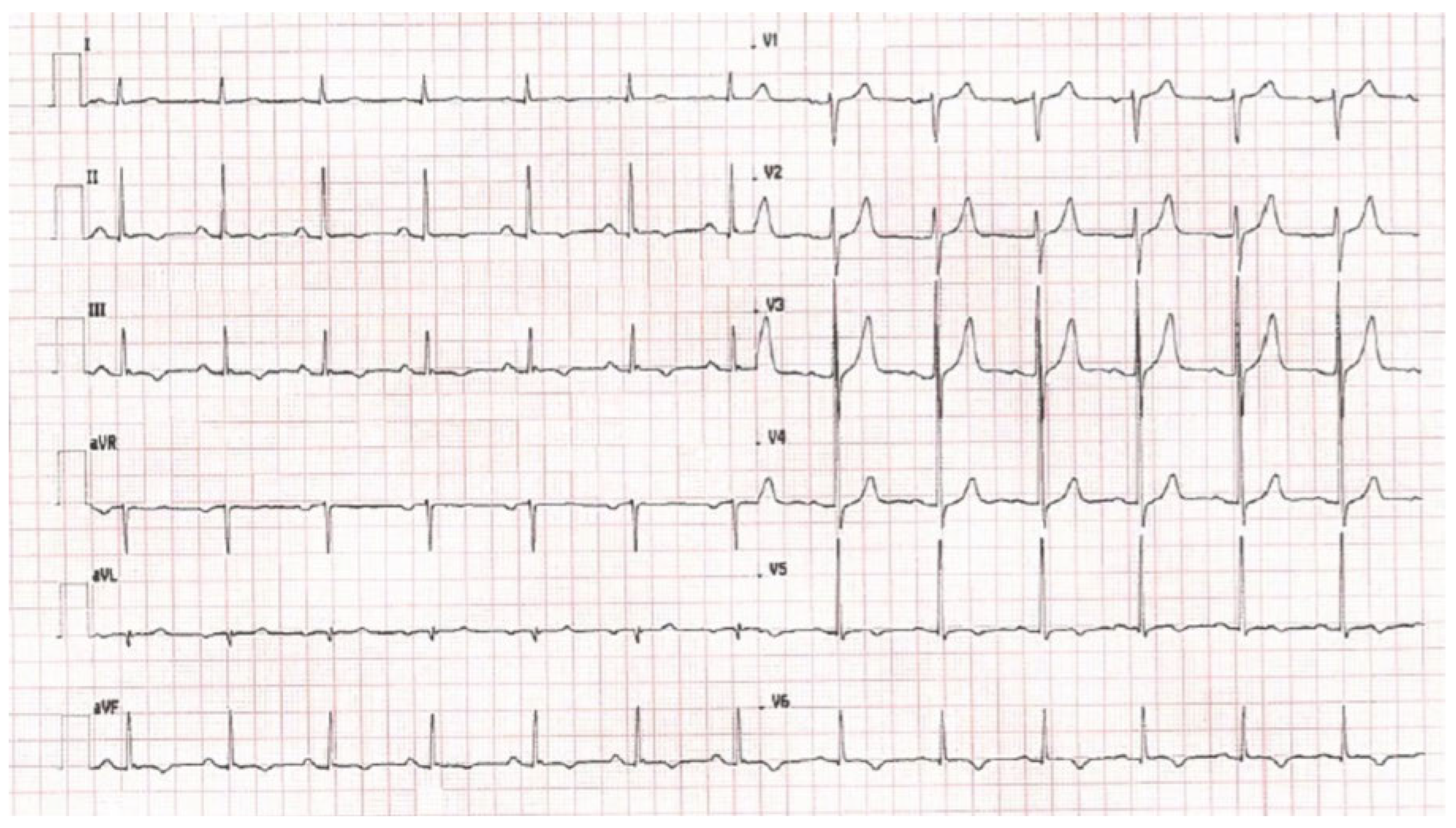
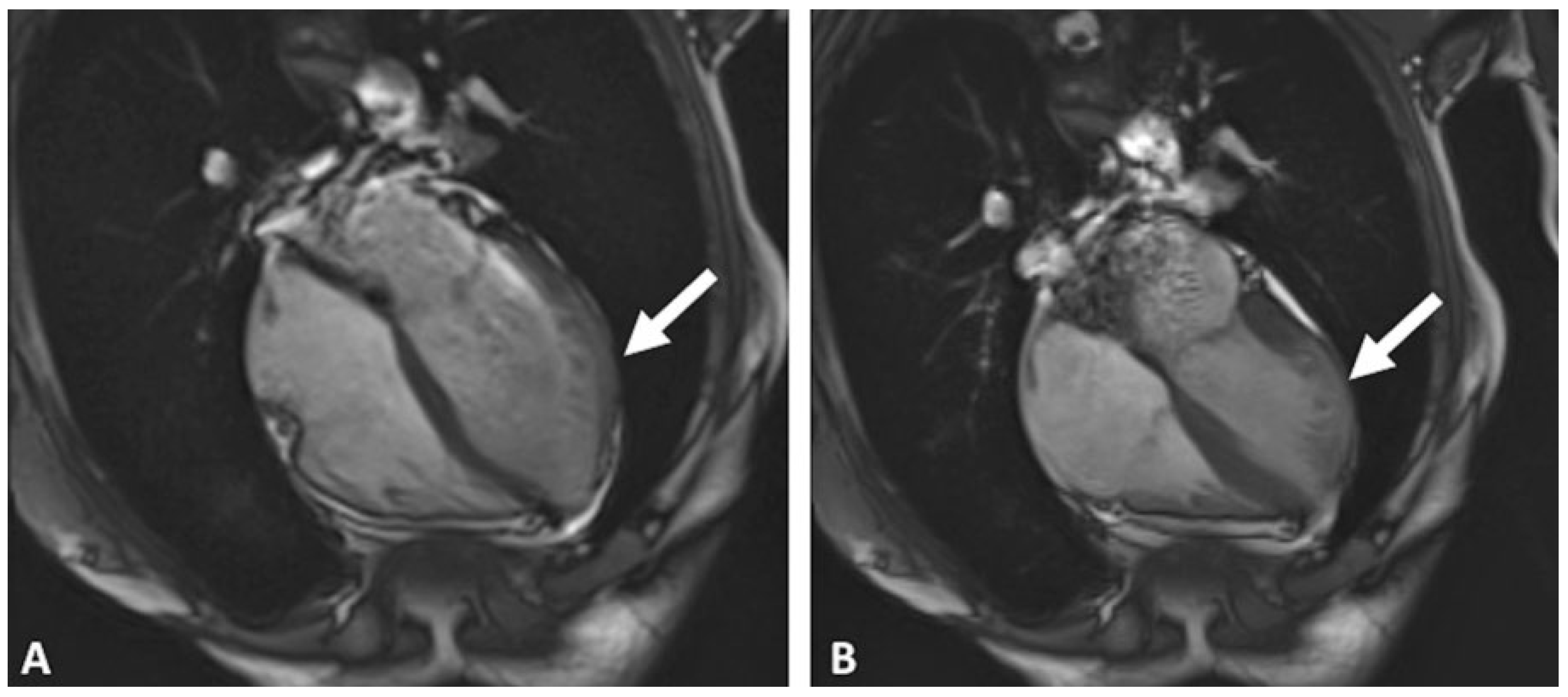
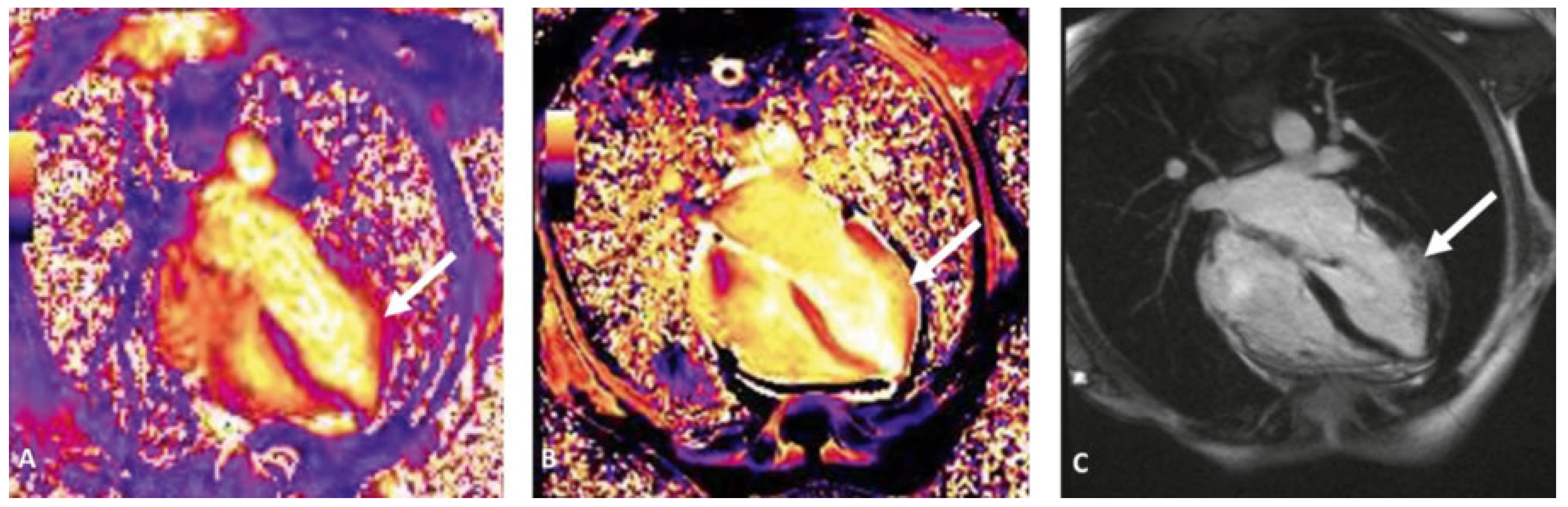
Case report
Discussion
Conclusion
Conflicts of Interest
References
- Sheikh, A.R.; Sidharta, S.; Worthley, M.I.; Yeend, R.; Di Fiore, D.P.; Beltrame, D.F. The importance of evaluating patients with MINOCA (myocardial infarction with non-obstructed coronary arteries). Int J Cardiol. 2015, 119, 386–388. [Google Scholar] [CrossRef] [PubMed]
- Ghosh Dastidar, A.; Jonathan CLRodrigues Baritussio, A.; Bucciarelli-Ducci, C. MRI in the assessment of ischaemic heart disesase. Heart. 2016, 102, 239–252. [Google Scholar] [CrossRef] [PubMed]
- Bulluck, H.; Maestrini, V.; Rosmini, S.; Abdel-Gadir, A.; Treibel, T.A.; Castelletti, S.; et al. Myocardial T1 mapping. Circ J. 2015, 79, 487–494. [Google Scholar] [CrossRef] [PubMed]
- Ghosh Dastidar, A.; Rodrigues, J.C.; Ahmed, N.; Baritussio, A.; Bucciarelli-Ducci, C. The Role of cardiac MRI in patient with troponinpositive chest pain and unobstructed coronary arteries. Curr Cardiovasc Imaging Rep. 2015, 8, 28. [Google Scholar] [CrossRef] [PubMed]

© 2017 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Paiocchia, V.L.; Leoa, L.A.; Marcona, S.; Moccettia, T.; Faletraa, F.F.; Bucciarelli-Duccia, C. The Diagnostic Dilemma of Myocardial Infarction with Unobstructed Coronary Arteries. Cardiovasc. Med. 2017, 20, 105. https://doi.org/10.4414/cvm.2017.00473
Paiocchia VL, Leoa LA, Marcona S, Moccettia T, Faletraa FF, Bucciarelli-Duccia C. The Diagnostic Dilemma of Myocardial Infarction with Unobstructed Coronary Arteries. Cardiovascular Medicine. 2017; 20(4):105. https://doi.org/10.4414/cvm.2017.00473
Chicago/Turabian StylePaiocchia, Vera Lucia, Laura Anna Leoa, Serena Marcona, Tiziano Moccettia, Francesco Fulvio Faletraa, and Chiara Bucciarelli-Duccia. 2017. "The Diagnostic Dilemma of Myocardial Infarction with Unobstructed Coronary Arteries" Cardiovascular Medicine 20, no. 4: 105. https://doi.org/10.4414/cvm.2017.00473
APA StylePaiocchia, V. L., Leoa, L. A., Marcona, S., Moccettia, T., Faletraa, F. F., & Bucciarelli-Duccia, C. (2017). The Diagnostic Dilemma of Myocardial Infarction with Unobstructed Coronary Arteries. Cardiovascular Medicine, 20(4), 105. https://doi.org/10.4414/cvm.2017.00473



