COPD Exacerbation and Prevention
Abstract
Introduction and definition
Epidemiology
Pathophysiology
Diagnosis and assessment
- -
- Pulse oxymetry is useful for monitoring and adjusting supplemental oxygen therapy.
- -
- The measurement of arterial blood gasses is vital if the coexistence of acute or acute-on-chronic respiratory failure is suspected: PaO2 <8.0 kPa (60 mm Hg) with or without PaCO2 >6.7 kPa (50 mm Hg) breathing ambient air.
- -
- Assessment of acid-base status is necessary before initiating mechanical ventilation.
- -
- Chest radiographs are useful for excluding alternative diagnoses.
- -
- An ECG may help for the diagnosis of coexisting cardiac problems.
- -
- The whole blood count may identify polycythaemia (haematocrit >55%), anaemia or leucocytosis. Moreover, eosinophilia has been associated with an increased risk of readmission in severe COPD exacerbations [63].
- -
- Spirometry is not recommended during an exacerbation because it can be difficult to perform, and measurements are considered not accurate enough.
- -
- The presence of purulent sputum can be a sufficient indication for starting empirical antibiotic treatment. A sputum culture with antibiotic sensitivity tests should be performed.
Differential diagnosis
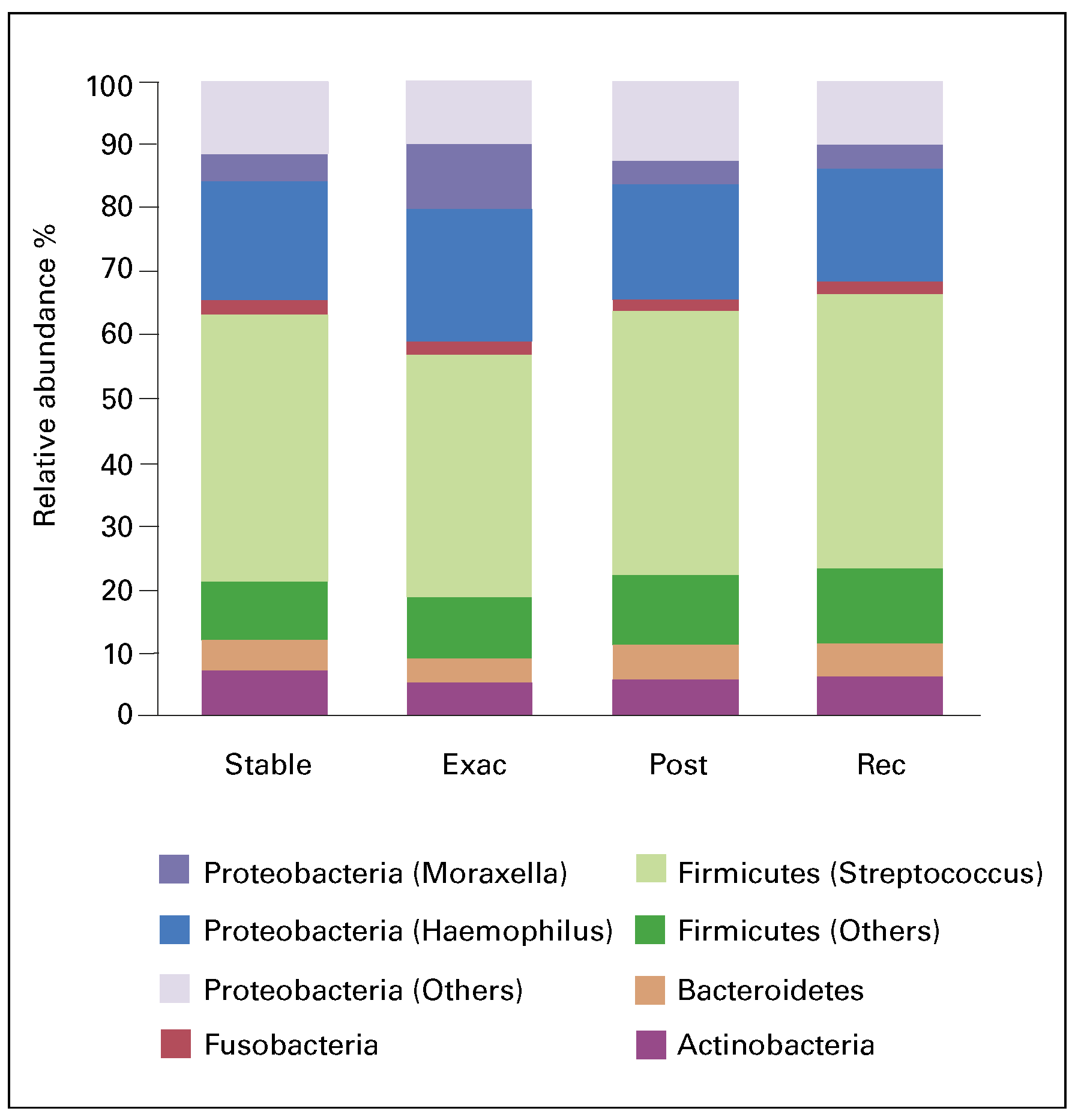
Aetiology, triggers and biomarkers
Cardiovasular consequences
Prevention
Influenza and pneumococcal vaccination
Smoking cessation
Pulmonary rehabilitation
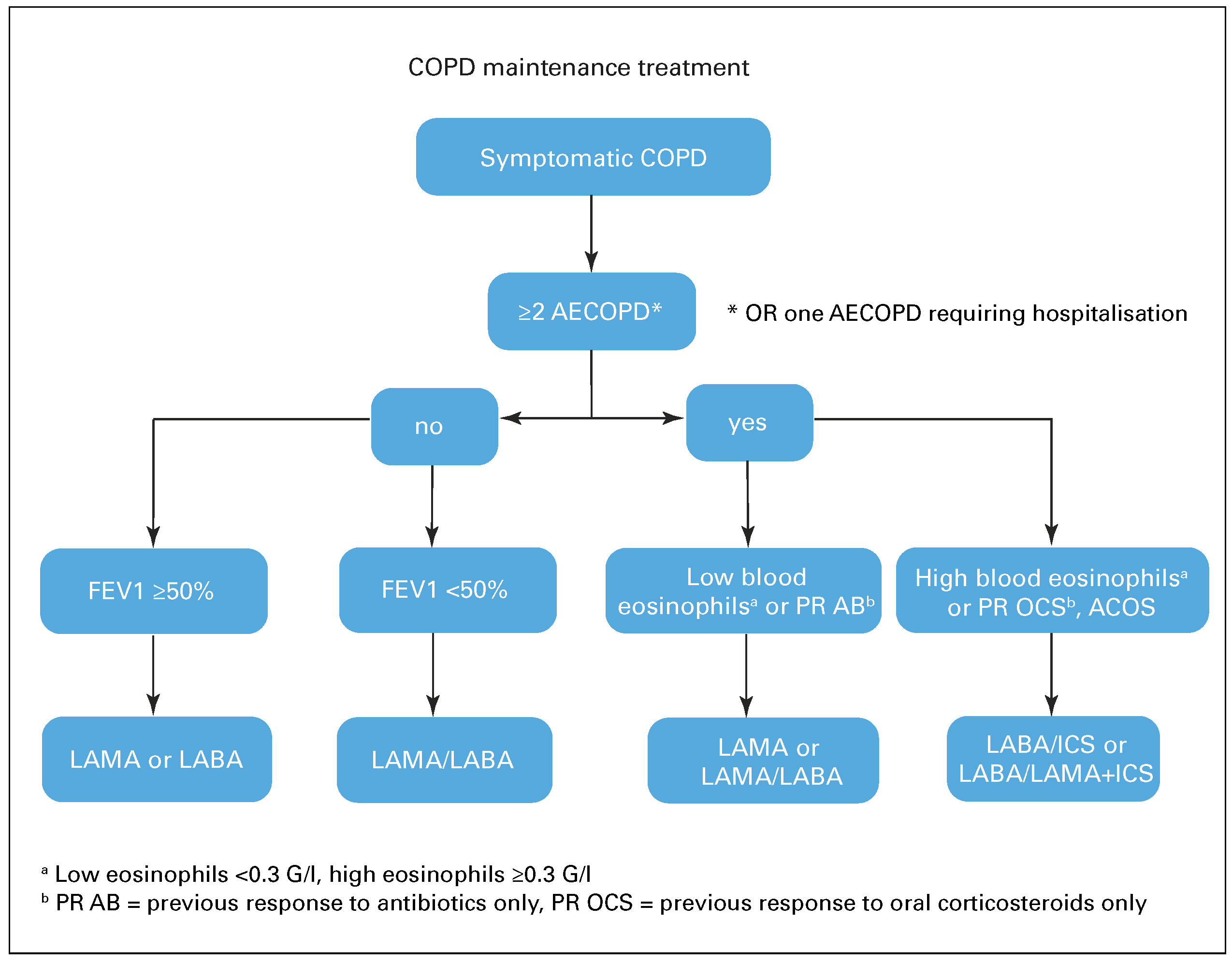
Pharmacological treatment
Long-acting bronchodilators
Long-acting bronchodilators and inhaled corticosteroids
Triple inhaled therapy (LABA/LAMA/ICS)
Phosphodiesterase-4 inhibitors
Macrolide antibiotics
N-acetylcysteine and other mucolytic agents
Beta-blockers
Conclusions
Disclosure statement
References
- Lopez, A.D. Chronic obstructive pulmonary disease: Current burden and future projections. Eur Respir J. 2006, 27, 397–412. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Flaxman, A.D.; Naghavi, M.; Lozano, R.; Michaud, C.; Ezzati, M.; et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012, 380, 2163–2196. [Google Scholar] [CrossRef] [PubMed]
- Soriano, J.B.; Rodriguez-Roisin, R. Chronic Obstructive Pulmonary Disease Overview: Epidemiology, Risk Factors, and Clinical Presentation. Proc Am Thorac Soc. 2011, 8, 363–367. [Google Scholar] [CrossRef]
- Rodriguez-Roisin, R. Toward a Consensus Definition for COPD Exacerbations. Chest. 2000, 117. [Google Scholar] [CrossRef]
- Vestbo, J.; Anderson, W.; Coxson, H.O.; Crim, C.; Dawber, F.; Edwards, L.; et al. Evaluation of COPD Longitudinally to Identify Predictive Surrogate End-points (ECLIPSE). Eur Respir J. 2008, 31, 869–873. [Google Scholar] [CrossRef]
- Hurst, J.R.; Vestbo, J.; Anzueto, A.; Locantore, N.; Müllerova, H.; Tal-Singer, R.; et al. Susceptibility to Exacerbation in Chronic Obstructive Pulmonary Disease. N Engl J Med. 2010, 363, 1128–1138. [Google Scholar] [CrossRef]
- Miravitlles, M.; Guerrero, T.; Mayordomo, C.; Sánchez-Agudo, L.; Nicolau, F.; Segú, J.L. Factors Associated with Increased Risk of Exacerbation and Hospital Admission in a Cohort of Ambulatory COPD Patients: A Multiple Logistic Regression Analysis. Respiration. 2000, 67, 495–501. [Google Scholar] [CrossRef]
- Rascon-Aguilar, I.E. Role of Gastroesophageal Reflux Symptoms in Exacerbations of COPD. Chest. 2006, 130, 1096. [Google Scholar] [CrossRef]
- Garcia-Pachon, E.; Padilla-Navas, I. Risk Indexes for COPD Exacerbations I. Chest. 2007, 131, 1986. [Google Scholar] [CrossRef]
- Niewoehner, D.E. Risk Indexes for COPD Exacerbations II. Chest. 2007, 131, 1987. [Google Scholar] [CrossRef]
- Burgel, P.; Nesme-Meyer, P.; Chanez, P.; Caillaud, D.; Carré, P.; Perez, T.; et al. Cough and Sputum Production Are Associated With Frequent Exacerbations and Hospitalizations in COPD Subjects. Chest. 2009, 135, 975–982. [Google Scholar] [CrossRef]
- Vedel-Krogh, S.; Nielsen, S.F.; Lange, P.; Vestbo, J.; Nordestgaard, B.G. Blood Eosinophils and Exacerbations in Chronic Obstructive Pulmonary Disease. The Copenhagen General Population Study. Am J Respir Crit Care Med. 2016, 193, 965–974. [Google Scholar] [CrossRef] [PubMed]
- Terada, K.; Muro, S.; Sato, S.; Ohara, T.; Haruna, A.; Marumo, S.; et al. Impact of gastro-oesophageal reflux disease symptoms on COPD exacerbation. Thorax. 2008, 63, 951–955. [Google Scholar] [CrossRef] [PubMed]
- Wells, J.M.; Washko, G.R.; Han, M.K.; Abbas, N.; Nath, H.; Mamary, A.J.; et al. Pulmonary Arterial Enlargement and Acute Exacerbations of COPD. N Engl J Med. 2012, 367, 913–921. [Google Scholar] [CrossRef]
- O’donnell, D.E. COPD exacerbations {middle dot} 3: Pathophysiology. Thorax. 2006, 61, 354–361. [Google Scholar] [CrossRef]
- Orozco-Levi, M.; Lloreta, J.; Minguella, J.; Serrano, S.; Broquetas, J.M.; Gea, J. Injury of the Human Diaphragm Associated with Exertion and Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2001, 164, 1734–1739. [Google Scholar] [CrossRef]
- Calverley, P. Respiratory failure in chronic obstructive pulmonary disease. Eur Respir J. 2003, 22 (Suppl. 47). [Google Scholar] [CrossRef]
- Anthonisen, N.R. Antibiotic Therapy in Exacerbations of Chronic Obstructive Pulmonary Disease. Ann Intern Med. 1987, 106, 196. [Google Scholar] [CrossRef]
- Global Strategy for the Dianosis. Management and Prevention of COPD, Global Initiative for Chronic Obstructive Lung Disease (GOLD) 2016. Available online: http://www.goldcopd.org (accessed on 20 October 2016).
- Zvezdin, B.; Milutinov, S.; Kojicic, M.; Hadnadjev, M.; Hromis, S.; Markovic, M.; et al. A Postmortem Analysis of Major Causes of Early Death in Patients Hospitalized With COPD Exacerbation. Chest. 2009, 136, 376–380. [Google Scholar] [CrossRef]
- Wedzicha, J.A.; Seemungal, T.A. COPD exacerbations: Defining their cause and prevention. Lancet. 2007, 370, 786–796. [Google Scholar] [CrossRef]
- Papi, A.; Bellettato, C.M.; Braccioni, F.; Romagnoli, M.; Casolari, P.; Caramori, G.; et al. Infections and Airway Inflammation in Chronic Obstructive Pulmonary Disease Severe Exacerbations. Am J Respir Crit Care Med. 2006, 173, 1114–1121. [Google Scholar] [CrossRef]
- Wang, Z.; Bafadhel, M.; Haldar, K.; Spivak, A.; Mayhew, D.; Miller, B.E.; et al. Lung microbiome dynamics in COPD exacerbations. Eur Respir J. 2016, 47, 1082–1092. [Google Scholar] [CrossRef] [PubMed]
- Bafadhel, M.; Mckenna, S.; Terry, S.; Mistry, V.; Reid, C.; Haldar, P.; et al. Acute Exacerbations of Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med. 2011, 184, 662–671. [Google Scholar] [CrossRef] [PubMed]
- Thomsen, M.; Ingebrigtsen, T.S.; Marott, J.L.; Dahl, M.; Lange, P.; Vestbo, J.; et al. Inflammatory Biomarkers and Exacerbations in Chronic Obstructive Pulmonary Disease. JAMA. 2013, 309, 2353. [Google Scholar] [CrossRef]
- Rothnie, K.J.; Yan, R.; Smeeth, L.; Quint, J.K. Risk of myocardial infarction (MI) and death following MI in people with chronic obstructive pulmonary disease (COPD): A systematic review and metaanalysis. BMJ Open. 2015, 5. [Google Scholar] [CrossRef]
- Donaldson, G.C.; Hurst, J.R.; Smith, C.J.; Hubbard, R.B.; Wedzicha, J.A. Increased Risk of Myocardial Infarction and Stroke Following Exacerbation of COPD. Chest. 2010, 137, 1091–1097. [Google Scholar] [CrossRef]
- Calverley, P.M.; Anderson, J.A.; Celli, B.; Ferguson, G.T.; Jenkins, C.; Jones, P.W.; et al. Salmeterol and Fluticasone Propionate and Survival in Chronic Obstructive Pulmonary Disease. N Engl J Med. 2007, 356, 775–789. [Google Scholar] [CrossRef]
- Chang, C.L.; Robinson, S.C.; Mills, G.D.; Sullivan, G.D.; Karalus, N.C.; Mclachlan, J.D.; et al. Biochemical markers of cardiac dysfunction predict mortality in acute exacerbations of COPD. Thorax. 2011, 66, 764–768. [Google Scholar] [CrossRef]
- Pizarro, C.; Herweg-Steffens, N.; Buchenroth, M.; Schulte, W.; Schaefer, C.; Hammerstingl, C.; et al. Invasive coronary angiography in patients with acute exacerbated COPD and elevated plasma troponin. Int J Chron Obstruct Pulmon Dis. 2016, 11, 2081–2089. [Google Scholar] [CrossRef]
- Poole, P.; Chacko, E.E.; Wood-Baker, R.; Cates, C.J. Influenza vaccine for patients with chronic obstructive pulmonary disease. Cochrane Database of Systematic Reviews Reviews. 2006. [Google Scholar] [CrossRef]
- González-Moro, J.M.; Menéndez, R.; Campins, M.; Lwoff, N.; Oyagüez, I.; Echave, M.; et al. Cost Effectiveness of the 13-Valent Pneumococcal Conjugate Vaccination Program in Chronic Obstructive Pulmonary Disease Patients Aged 50 Years in Spain. Clin Drug Investig. 2015, 36, 41–53. [Google Scholar] [CrossRef]
- Casaburi, R.; Zuwallack, R. Pulmonary Rehabilitation for Management of Chronic Obstructive Pulmonary Disease. N Engl J Med. 2009, 360, 1329–1335. [Google Scholar] [CrossRef] [PubMed]
- Moore, E.; Palmer, T.; Newson, R.; Majeed, A.; Quint, J.K.; Soljak, M.A. Pulmonary Rehabilitation as a Mechanism to Reduce Hospitalizations for Acute Exacerbations of COPD. Chest. 2016, 150, 837–859. [Google Scholar] [CrossRef] [PubMed]
- Du, Q.; Sun, Y.; Ding, N.; Lu, L.; Chen, Y. Beta-Blockers Reduced the Risk of Mortality and Exacerbation in Patients with COPD: A Meta-Analysis of Observational Studies. PLoS ONE. 2014, 9. [Google Scholar] [CrossRef] [PubMed]
- Du, Q.; Sun, Y.; Ding, N.; Lu, L.; Chen, Y. Beta-Blockers Reduced the Risk of Mortality and Exacerbation in Patients with COPD: A Meta-Analysis of Observational Studies. PLoS ONE. 2014, 9. [Google Scholar] [CrossRef]
- Calverley, P.M.; Anderson, J.A.; Celli, B.; Ferguson, G.T.; Jenkins, C.; Jones, P.W.; et al. Salmeterol and fluticasone propionate and survival in chronic obstructive pulmonary disease. N Engl J Med. 2007, 356, 775–789. [Google Scholar] [CrossRef]
- Tashkin, D.P.; Celli, B.; Senn, S.; Burkhart, D.; Kesten, S.; Menjoge, S.; et al. A 4-Year Trial of Tiotropium in Chronic Obstructive Pulmonary Disease. N Engl J Med. 2008, 359, 1543–1554. [Google Scholar] [CrossRef]
- Karner, C.; Chong, J.; Poole, P. Tiotropium versus placebo for chronic obstructive pulmonary disease. Cochrane Database Syst Rev. 2014, 7, CD009285. [Google Scholar] [CrossRef]
- Kerwin, E.; Hébert, J.; Gallagher, N.; Martin, C.; Overend, T.; Alagappan, V.K.; et al. Efficacy and safety of NVA237 versus placebo and tiotropium in patients with COPD: The GLOW2 study. Eur Respir J. 2012, 40, 1106–1114. [Google Scholar] [CrossRef]
- Bateman, E.D.; Chapman, K.R.; Singh, D.; D’Urzo, A.D.; Molins, E.; Leselbaum, A.; et al. Aclidinium bromide and formoterol fumarate as a fixed-dose combination in COPD: Pooled analysis of symptoms and exacerbations from two six-month, multicentre, randomised studies (ACLIFORM and AUGMENT). Respir Res. 2015, 16, 92. [Google Scholar] [CrossRef]
- Vogelmeier, C.; Hederer, B.; Glaab, T.; Schmidt, H.; Rutten-van Mölken, M.P.; Beeh, K.M.; et al. Tiotropium versus salmeterol for the prevention of exacerbations of COPD. N Engl J Med. 2011, 364, 1093–1103. [Google Scholar] [CrossRef] [PubMed]
- Decramer, M.L.; Chapman, K.R.; Dahl, R.; Frith, P.; Devouassoux, G.; Fritscher, C.; et al. Once-daily indacaterol versus tiotropium for patients with severe chronic obstructive pulmonary disease (INVIGO-RATE): A randomised, blinded, parallel-group study. Lancet Respir Med. 2013, 1, 524–533. [Google Scholar] [CrossRef]
- Zhong, N.; Wang, C.; Zhou, X.; Zhang, N.; Humphries, M.; Wang, C.; et al. LANTERN: A randomized study of QVA149 versus salmeterol/ fluticasone combination in patients with COPD. Int J COPD. 2015, 10, 1015–1026. [Google Scholar]
- Wedzicha, J.A.; Banerji, D.; Chapman, K.R.; Vestbo, J.; Roche, N.; Ayers, R.T.; et al. Indacaterol-glycopyrronium versus salmeterol-fluticasone for COPD. N Engl J Med. 2016. [Google Scholar] [CrossRef]
- Brightling, C.E.; McKenna, S.; Hargadon, B.; Birring, S.; Green, R.; Siva, R.; et al. Sputum eosinophilia and the short term response to inhaled mometasone in chronic obstructive pulmonary disease. Thorax. 2005, 60, 193–198. [Google Scholar] [CrossRef]
- Calverley, P.M.; Anderson, J.A.; Celli, B.; Ferguson, G.T.; Jenkins, C.; Jones, P.W.; et al. Salmeterol and fluticasone propionate andsurvival in chronic obstructive pulmonary disease. N Engl J Med. 2007, 356, 775–789. [Google Scholar] [CrossRef]
- Calverley, P.M.; Boonsawat, W.; Cseke, Z.; Zhong, N.; Peterson, S.; Olsson, H. Maintenance therapy with budesonide and formoterol in chronic obstructive pulmonary disease. Eur Respir J. 2003, 22, 912–919. [Google Scholar] [CrossRef]
- Magnussen, H.; Disse, B.; Rodriguez-Roisin, R.; Kirsten, A.; Watz, H.; Tetzlaff, K.; et al. Withdrawal of inhaled glucocorticoids and exacerbations of COPD. N Engl J Med. 2014, 371, 1285–1294. [Google Scholar] [CrossRef]
- Rossi, A.; van der Molen, T.; del Olmo, R.; Papi, A.; Wehbe, L.; Quinn, M.; et al. INSTEAD: A randomised switch trial of indacaterol versus salmeterol/fluticasone in moderate COPD. Eur Respir J. 2014, 44, 1548–1556. [Google Scholar] [CrossRef]
- Singh, D.; Papi, A.; Corradi, M.; Pavlišová, I.; Montagna, I.; Francisco, C.; et al. Single Inhaler Triple Therapy versus Inhaled Corticosteroid plus Long-acting β2-agonist Therapy for Chronic Obstructive Pulmonary Disease (TRILOGY): A Double-blind, Parallel Group, Randomised Controlled Trial. Lancet. 2016, 388, 963–973. [Google Scholar] [CrossRef]
- Calverley, P.M.; Rabe, K.F.; Goehring, U.M.; Kristiansen, S.; Fabbri, L.M.; Martinez, F.J. Roflumilast in symptomatic chronic obstructive pulmonary disease: Two randomised clinical trials. Lancet. 2009, 374, 685–694. [Google Scholar] [CrossRef]
- Martinez, F.J.; Calverley, P.M.; Goehring, U.M.; Brose, M.; Fabbri, L.M.; Rabe, K.F. Effect of roflumilast on exacerbations in patients with severe chronic obstructive pulmonary disease uncontrolled by combination therapy (REACT): A multicentre randomised controlled trial. Lancet. 2015, 385, 857–866. [Google Scholar] [CrossRef]
- Martinez, F.J.; Rabe, K.F.; Sethi, S.; Pizzichini, E.; Mcivor, A.; Anzueto, A.; et al. Effect of Roflumilast and Inhaled Corticosteroid/Long-Acting β2-Agonist on Chronic Obstructive Pulmonary Disease Exacerbations (RE 2 SPOND). A Randomized Clinical Trial. Am J Respir Crit Care Med. 2016, 194, 559–567. [Google Scholar] [CrossRef] [PubMed]
- Wedzicha, J.A.; Calverley, P.M.; Rabe, K.F. Roflumilast: A review of its use in the treatment of COPD. Int J Chron Obstruct Pulmon Dis. 2016, 11, 81–90. [Google Scholar] [CrossRef] [PubMed]
- Herath, S.C.; Poole, P. Prophylactic antibiotic therapy for chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2013, 11, CD009764. [Google Scholar] [CrossRef]
- Albert, R.K.; Connett, J.; Bailey, W.C.; Casaburi, R.; Cooper, J.A.; Jr Criner, G.J.; et al. zithromycin for prevention of exacerbations of COPD. N Engl J Med. 2011, 365, 689–698. [Google Scholar] [CrossRef]
- Han, M.K.; Tayob, N.; Murray, S.; Dransfield, M.T.; Washko, G.; Scanlon, P.D.; et al. Predictors of Chronic Obstructive Pulmonary Disease Exacerbation Reduction in Response to Daily Azithromycin Therapy. Am J Respir Crit Care Med. 2014, 189, 1503–1508. [Google Scholar] [CrossRef]
- Sanguinetti, C.M. «N-acetylcysteine in COPD: Why, How, and When?». Multidiscip Respir Med 2015, 11. [Google Scholar] [CrossRef]
- Poole, P.; Sathananthan, K.; Fortescue, R. «Mucolytic Agents versus Placebo for Chronic Bronchitis or Chronic Obstructive Pulmonary Disease.». Cochrane Database of Systematic Reviews Reviews 2019, CD001287. [Google Scholar] [CrossRef]
- Cazzola, M.; Calzetta, L.; Page, C.; Jardim, J.; Chuchalin, A.G.; Rogliani, P.; et al. Influence of N -acetylcysteine on Chronic Bronchitis or COPD Exacerbations: A Meta-analysis. Eur Respir Rev. 2015, 24, 451–461. [Google Scholar] [CrossRef]
- Dal Negro, R.I.M.; Calverly, P. Efficacy and safety of erdosteine in COPD: Results of a 12-month prospective, multinational study. Presented at the European Respiratory Society Annual Congress 2015, (Abstract PA1495), 2015. Amsterdam, The Netherlands, 26–30 September 2015. [Google Scholar]
- Couillard, S.; Larivée, P.; Courteau, J.; Vanasse, A. Eosinophils in chronic obstructive pulmonary disease exacerbations are associated with increased readmissions. Chest. 2016. [Google Scholar] [CrossRef]
- Aleva, F.E.; Voets, L.W.L.M.; Simons, S.O.; de Mast, Q.; van der Ven, A.J.A.M.; Heijdra, Y.F. Prevalence and Localization of Pulmonary Embolism in Unexplained Acute Exacerbations of COPD: A systematic review and meta-analysis. Chest. 2016. [Google Scholar] [CrossRef]
- Stolz, D.; Christ-Crain, M.; Bingisser, R.; et al. Antibiotic treatment of exacerbations of COPD: A randomized, controlled trial comparing procalcitonin-guidance with standard therapy. Chest. 2007, 131, 9–19. [Google Scholar] [CrossRef]
- Daniels, M.A.; Schoorl, M.; Snijders, D.; et al. Procalcitonin vs C-reactive protein as predictive markers of response to antibiotic therapy in acute exacerbations of COPD. Chest. 2010, 138, 1108–1115. [Google Scholar] [CrossRef]

| Medical history | Severity of COPD based on degree of airflow limitation |
| Duration of worsening or new symptoms Number of previous episodes (total/hospitalisations) | |
| Comorbidities Present treatment regimen | |
| Previous use of mechanical ventilation | |
| Signs of severity | Use of accessory respiratory muscles |
| Paradoxical chest wall movements | |
| Worsening or new onset central cyanosis | |
| Development of peripheral oedema | |
| Haemodynamic instability Deteriorated mental status |
| Bacteria | Haemophilus influenzae |
| Moraxella catarrhalis | |
| Streptococcus pneumoniae | |
| Pseudomonas aeruginosa | |
| Viruses | Rhinovirus |
| Coronavirus | |
| Influenza | |
| Parainfluenza | |
| Adenovirus | |
| Respiratory syncytial virus |
© 2017 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Valdés, C.R.P.; Lenoir, A.; Nicod, L. COPD Exacerbation and Prevention. Cardiovasc. Med. 2017, 20, 38. https://doi.org/10.4414/cvm.2017.00461
Valdés CRP, Lenoir A, Nicod L. COPD Exacerbation and Prevention. Cardiovascular Medicine. 2017; 20(2):38. https://doi.org/10.4414/cvm.2017.00461
Chicago/Turabian StyleValdés, Carlos Roberto Pérez, Alexandra Lenoir, and Laurent Nicod. 2017. "COPD Exacerbation and Prevention" Cardiovascular Medicine 20, no. 2: 38. https://doi.org/10.4414/cvm.2017.00461
APA StyleValdés, C. R. P., Lenoir, A., & Nicod, L. (2017). COPD Exacerbation and Prevention. Cardiovascular Medicine, 20(2), 38. https://doi.org/10.4414/cvm.2017.00461




