Current Trends in Dual Antiplatelet Therapy: A 2017 Update
Abstract
Introduction
Historical background
Available drugs
Clopidogrel
Prasugrel
Ticagrelor
Cangrelor
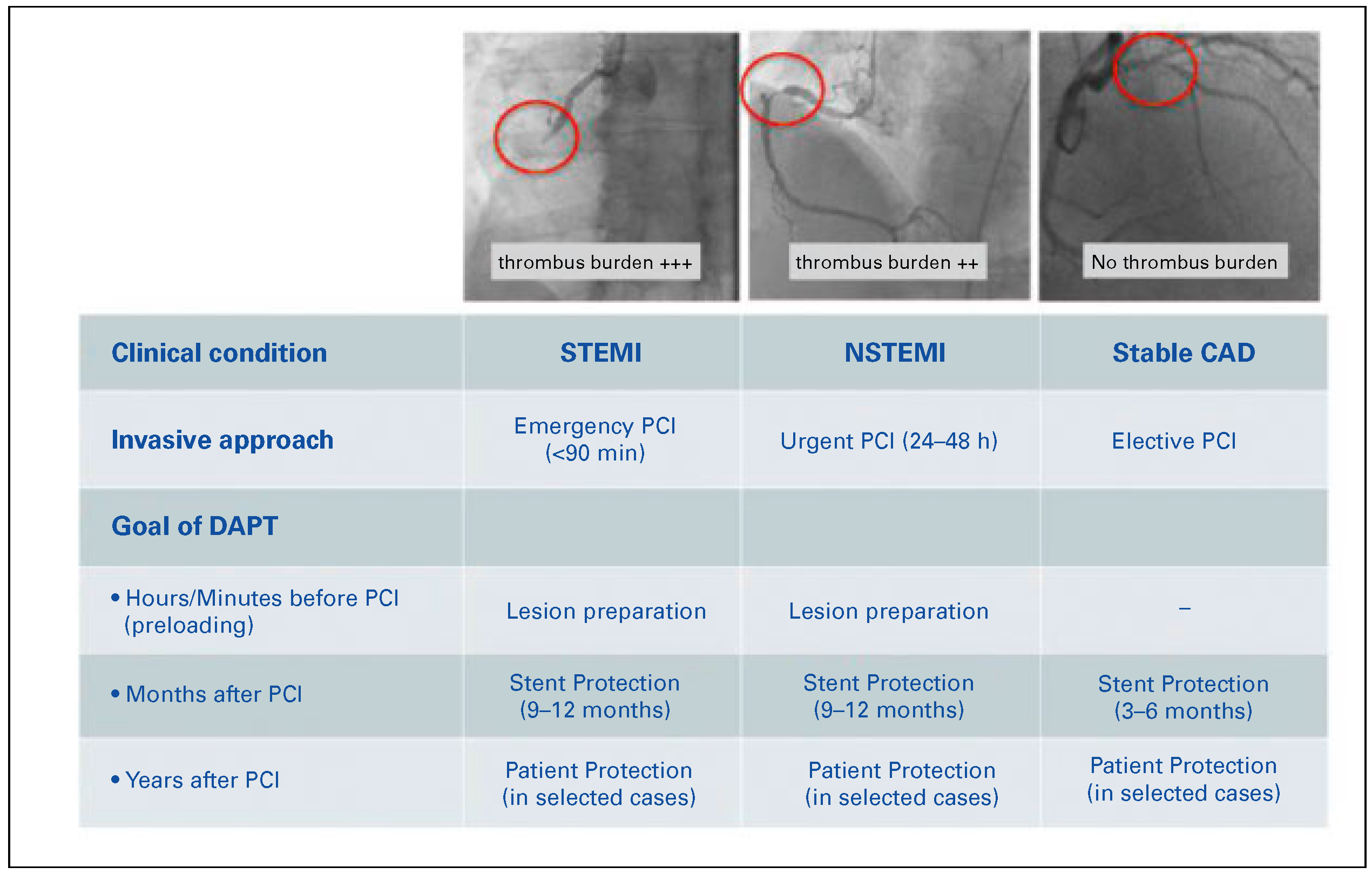
Current role of dual antiplatelet therapy
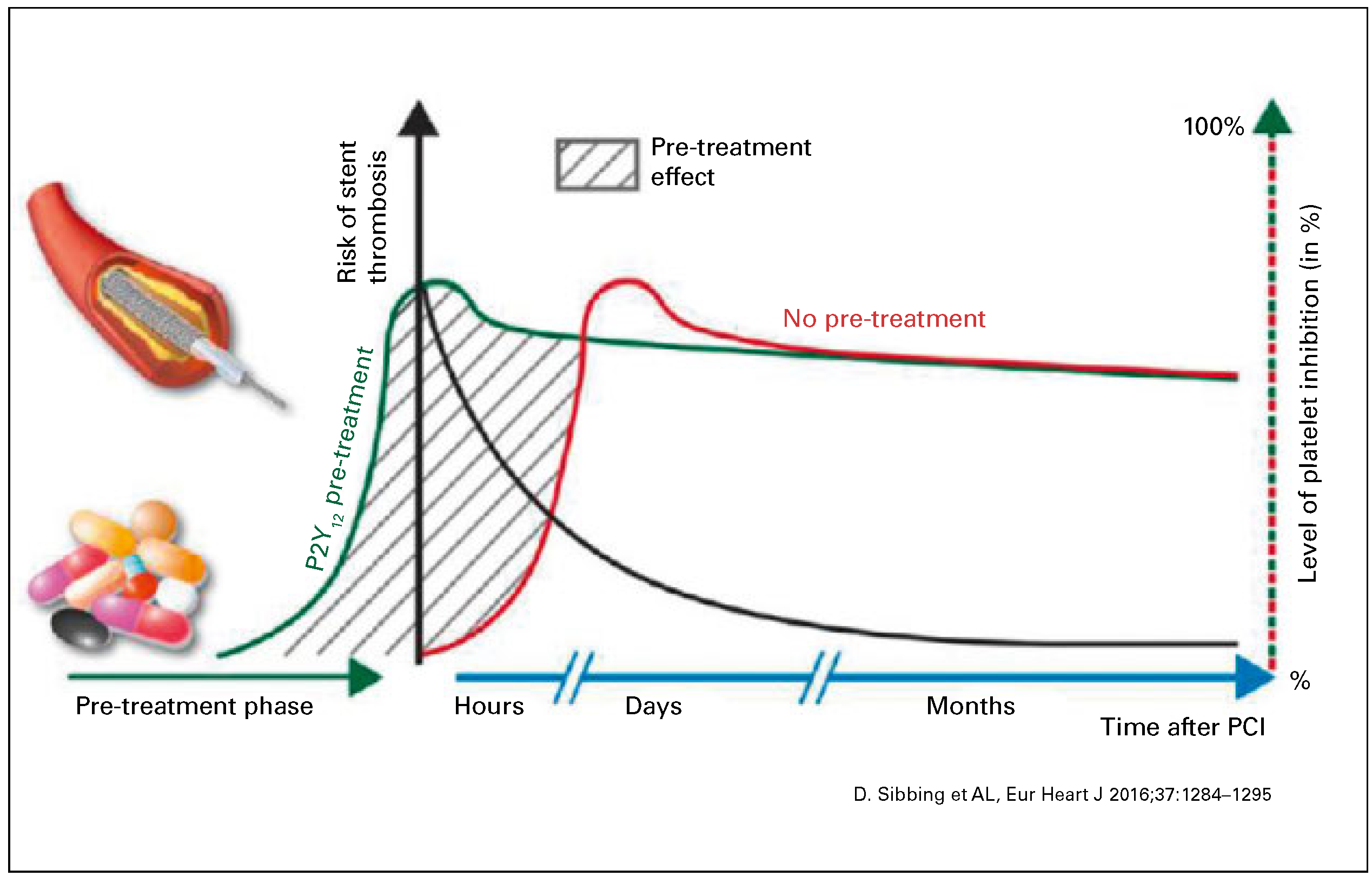
Preloading in acute coronary syndromes
ST-segment elevation ACS
Non-ST-segment elevation-ACS
Optimal length of DAPT after stent implantation
DAPT beyond 12 months
DAPT and oral anticoagulation
Open questions and future perspectives
Platelet inhibition following structural interventions
Conclusions
Disclosure Statement
References
- Steg, P.G.; James, S.K.; Atar, D.; Badano, L.P.; Blömstrom-Lundqvist, C.; Borger, M.A.; Task Force on the management of ST-segment elevation acute myocardial infarction of the European Society of Cardiology (ESC); et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012, 33, 2569–2619. [Google Scholar] [CrossRef]
- Windecker, S.; Kolh, P.; Alfonso, F.; Collet, J.P.; Cremer, J.; Falk, V.; et al. Authors/Task Force members 2014 ESC/EACTSGuidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J. 2014, 35, 2541–2619. [Google Scholar] [CrossRef]
- Roffi, M.; Patrono, C.; Collet, J.P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: Task Force for the Management of Acute Coronary Syndromes in Patients Presenting without Persistent ST-Segment Elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016, 37, 267–315. [Google Scholar] [CrossRef] [PubMed]
- Andrews, R.K.; LɃpez, J.A.; Berndt, M.C. Molecular mechanisms of platelet adhesion and activation. Int J Biochem Cell Biol. 1997, 29, 91–105. [Google Scholar] [CrossRef]
- CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet. 1996, 348, 1329–1339. [Google Scholar] [CrossRef] [PubMed]
- SchɆmig, A.; Neumann, F.J.; Kastrati, A.; Schɒhlen, H.; Blasini, R.; Hadamitzky, M.; et al. A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N Engl J Med. 1996, 334, 1084–1089. [Google Scholar] [CrossRef]
- Yusuf, S.; Zhao, F.; Mehta, S.R.; Chrolavicius, S.; Tognoni, G.; Fox, K.K.; Clopidogrel in Unstable Angina to Prevent Recurrent Events Trial Investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without ST-segment elevation. N Engl J Med. 2001, 345, 494–502. [Google Scholar] [CrossRef]
- Mehta, S.R.; Yusuf, S.; Peters, R.J.; Bertrand, M.E.; Lewis, B.S.; Natarajan, M.K.; Clopidogrel in Unstable angina to prevent Recurrent Events trial (CURE) Investigators; et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: The PCI-CURE study. Lancet. 2001, 358, 527–533. [Google Scholar] [CrossRef] [PubMed]
- Steinhubl, S.R.; Berger, P.B.; Mann, J.T.; Fry, E.T., 3rd; DeLago, A.; Wilmer, C.; CREDO Investigators; et al. Early and sustained dual oral antiplatelet therapy following percutaneous coronary intervention: A randomized controlled trial. JAMA 2002, 288, 2411–2420. [Google Scholar] [CrossRef]
- Moses, J.W.; Leon, M.B.; Popma, J.J.; Fitzgerald, P.J.; Holmes, D.R.; O’Shaughnessy, C.; SIRIUS Investigators; et al. Sirolimus-eluting stents versus standard stents in patients with stenosis in a native coronary artery. N Engl J Med. 2003, 349, 1315–1323. [Google Scholar] [CrossRef]
- Bavry, A.A.; Kumbhani, D.J.; Helton, T.J.; Bhatt, D.L. What is the risk of stent thrombosis associated with the use of paclitaxel-eluting stents for percutaneous coronary intervention?: A meta-analysis. J Am Coll Cardiol. 2005, 45, 941–946. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Moreno, R.; Fernández, C.; Hernández, R.; Alfonso, F.; Angiolillo, D.J.; Sabaté, M.; et al. Drug-eluting stent thrombosis: Results from a pooled analysis including 10 randomized studies. J Am Coll Cardiol. 2005, 45, 954–959. [Google Scholar] [CrossRef]
- Bavry, A.A.; Kumbhani, D.J.; Helton, T.J.; Borek, P.P.; Mood, G.R.; Bhatt, D.L. Late thrombosis of drug-eluting stents: A meta-analysis of randomized clinical trials. Am J Med. 2006, 119, 1056–1061. [Google Scholar] [CrossRef]
- Berger, P.B.; Bhatt, D.L.; Fuster, V.; Steg, P.G.; Fox, K.A.; Shao, M.; CHARISMA Investigators; et al. Bleeding complications with dual antiplatelet therapy among patients with stable vascular disease or risk factors for vascular disease: Results from the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) trial. Circulation. 2010, 121, 2575–2583. [Google Scholar] [CrossRef]
- Wiviott, S.D.; Braunwald, E.; McCabe, C.H.; Montalescot, G.; Ruzyllo, W.; Gottlieb, S.; TRITON-TIMI 38 Investigators; et al. Prasugrel versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2007, 357, 2001–2015. [Google Scholar] [CrossRef]
- Wallentin, L.; Becker, R.C.; Budaj, A.; Cannon, C.P.; Emanuelsson, H.; Held, C.; PLATO Investigators; et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes. N Engl J Med. 2009, 361, 1045–1057. [Google Scholar] [CrossRef]
- Motovska, Z.; Hlinomaz, O.; Miklik, R.; Hromadka, M.; Varvarovsky, I.; Dusek, J.; PRAGUE-18 Study Group; et al. Prasugrel Versus Ticagrelor in Patients With Acute Myocardial Infarction Treated With Primary Percutaneous Coronary Intervention: Multicenter Randomized PRAGUE-18 Study. Circulation. 2016, 134, 1603–1612. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.L.; Stone, G.W.; Mahaffey, K.W.; Gibson, C.M.; Steg, P.G.; Hamm, C.W.; CHAMPION PHOENIX Investigators; et al. Effect of platelet inhibition with cangrelor during PCI on ischemic events. N Engl J Med. 2013, 368, 1303–1313. [Google Scholar] [CrossRef]
- Van de Werf, F.; Bax, J.; Betriu, A.; Blomstrom-Lundqvist, C.; Crea, F.; Falk, V.; ESCCommittee for Practice Guidelines (CPG); et al. Management of acute myocardial infarction in patients presenting with persistent ST-segment elevation: The Task Force on the Management of ST-Segment Elevation Acute Myocardial Infarction of the European Society of Cardiology. Eur Heart J. 2008, 29, 2909–2945. [Google Scholar] [CrossRef]
- Bassand, J.P.; Hamm, C.W.; Ardissino, D.; Boersma, E.; Budaj, A.; Fernȥndez-Avilȳs, F.; Task Force for Diagnosis and Treatment of Non-ST-Segment Elevation Acute Coronary Syndromes of European Society of Cardiology; et al. Guidelines for the diagnosis treatment of non-ST-segment elevation acute coronary syndromes. Eur Heart J. 2007, 28, 1598–1660. [Google Scholar] [CrossRef]
- Montalescot, G.; van’t Hof, A.W.; Lapostolle, F.; Silvain, J.; Lassen, J.F.; Bolognese, L.; ATLANTIC Investigators; et al. Prehospital ticagrelor in ST-segment elevation myocardial infarction. N Engl J Med. 2014, 371, 1016–1027. [Google Scholar] [CrossRef]
- Montalescot, G.; Bolognese, L.; Dudek, D.; Goldstein, P.; Hamm, C.; Tanguay, J.F.; ACCOAST Investigators; et al. Pretreatment with prasugrel in non-ST-segment elevation acute coronary syndromes. N Engl J Med. 2013, 369, 999–1010. [Google Scholar] [CrossRef]
- Gwon, H.C.; Hahn, J.Y.; Park, K.W.; Song, Y.B.; Chae, I.H.; Lim, D.S.; et al. Six-month versus 12-month dual antiplatelet therapy after implantation of drug-eluting stents: The Efficacy of Xience/Promus Versus Cypher to Reduce Late Loss After Stenting (EXCELLENT) randomized, multicenter study. Circulation. 2012, 125, 505–513. [Google Scholar] [CrossRef] [PubMed]
- Valgimigli, M.; Campo, G.; Monti, M.; Vranckx, P.; Percoco, G.; Tumscitz, C.; Prolonging Dual Antiplatelet Treatment After Grading Stent-Induced Intimal Hyperplasia Study (PRODIGY) Investigators; et al. Short- versus long-term duration of dual-antiplatelet therapy after coronary stenting: A randomized multicenter trial. Circulation. 2012, 125, 2015–2026. [Google Scholar] [CrossRef] [PubMed]
- Kim, B.K.; Hong, M.K.; Shin, D.H.; Nam, C.M.; Kim, J.S.; Ko, Y.G.; RESET Investigators; et al. A new strategy for discontinuation of dual antiplatelet therapy: The RESET Trial (REal Safety and Efficacy of 3-month dual antiplatelet Therapy following Endeavor zotarolimus-eluting stent implantation). J Am Coll Cardiol. 2012, 60, 1340–1348. [Google Scholar] [CrossRef]
- Feres, F.; Costa, R.A.; Abizaid, A.; Leon, M.B.; Marin-Neto, J.A.; Botelho, R.V.; OPTIMIZETrial Investigators; et al. Three vs twelve months of dual antiplatelet therapy after zotarolimus-eluting stents: The OPTIMIZErandomized trial. JAMA 2013, 310, 2510–2522. [Google Scholar] [CrossRef]
- Colombo, A.; Chieffo, A.; Frasheri, A.; Garbo, R.; Masotti-Centol, M.; Salvatella, N.; et al. Second-generation drug-eluting stent implantation followed by 6- versus 12-month dual antiplatelet therapy: The SECURITY randomized clinical trial. J Am Coll Cardiol. 2014, 64, 2086–2097. [Google Scholar] [CrossRef]
- Giustino, G.; Baber, U.; Sartori, S.; Mehran, R.; Mastoris, I.; Kini, A.S.; et al. Duration of dual antiplatelet therapy after drug-eluting stent implantation: A systematic review and meta-analysis of randomized controlled trials. J Am Coll Cardiol. 2015, 65, 1298–1310. [Google Scholar] [CrossRef] [PubMed]
- Urban, P.; Meredith, I.T.; Abizaid, A.; Pocock, S.J.; Carriȳ, D.; Naber, C.; LEADERS FREE Investigators; et al. Polymer-free Drug-Coated Coronary Stents in Patients at High Bleeding Risk. N Engl J Med. 2015, 373, 2038–2047. [Google Scholar] [CrossRef]
- Mauri, L.; Kereiakes, D.J.; Yeh, R.W.; Driscoll-Shempp, P.; Cutlip, D.E.; Steg, P.G.; DAPT Study Investigators; et al. Twelve or 30 months of dual antiplatelet therapy after drug-eluting stents. N Engl J Med. 2014, 371, 2155–2166. [Google Scholar] [CrossRef]
- Collet, J.P.; Silvain, J.; Barthȳlȳmy, O.; Rangȳ, G.; Cayla, G.; Van Belle, E.; ARCTIC investigators; et al. Dual-antiplatelet treatment beyond 1 year after drug-eluting stent implantation (ARCTIC-Interruption): A randomised trial. Lancet. 2014, 384, 1577–1585. [Google Scholar] [CrossRef]
- Lee, C.W.; Ahn, J.M.; Park, D.W.; Kang, S.J.; Lee, S.W.; Kim, Y.H.; et al. Optimal duration of dual antiplatelet therapy after drug-eluting stent implantation: A randomized, controlled trial. Circulation. 2014, 129, 304–312. [Google Scholar] [CrossRef]
- Bonaca, M.P.; Bhatt, D.L.; Cohen, M.; Steg, P.G.; Storey, R.F.; Jensen, E.C.; PEGASUS-TIMI 54 Steering Committee and Investigators; et al. Long-term use of ticagrelor in patients with prior myocardial infarction. N Engl J Med. 2015, 372, 1791–1800. [Google Scholar] [CrossRef]
- Valgimigli, M.; Campo, G.; Monti, M.; Vranckx, P.; Percoco, G.; Tumscitz, C. Prolonging Dual Antiplatelet Treatment After Grading Stent-Induced Intimal Hyperplasia Study (PRODIGY) Investigators. Short- versus long-term duration of dual-antiplatelet therapy after coronary stenting: A randomized multicenter trial. Circulation. 2012, 125, 2015–2026. [Google Scholar] [CrossRef]
- Navarese, E.P.; Andreotti, F.; Schulze, V.; Kołodziejczak, M.; Buffon, A.; Brouwer, M.; et al. Optimal duration of dual antiplatelet therapy after percutaneous coronary intervention with drug eluting stents: Meta-analysis of randomised controlled trials. BMJ. 2015, 350, h1618. [Google Scholar] [CrossRef]
- Hansen, M.L.; Sørensen, R.; Clausen, M.T.; Fog-Petersen, M.L.; Raunsø, J.; Gadsbøll, N.; et al. Risk of bleeding with single, dual, or triple therapy with warfarin, aspirin, and clopidogrel in patients with atrial fibrillation. Arch Intern Med. 2010, 170, 1433–1441. [Google Scholar] [CrossRef]
- Dewilde, W.J.; Oirbans, T.; Verheugt, F.W.; Kelder, J.C.; De Smet, B.J.; Herrman, J.P.; WOEST study investigators; et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: An open-label, randomised, controlled trial. Lancet. 2013, 381, 1107–1115. [Google Scholar] [CrossRef] [PubMed]
- Fiedler, K.A.; Maeng, M.; Mehilli, J.; Schulz-Schüpke, S.; Byrne, R.A.; Sibbing, D.; et al. Duration of Triple Therapy in Patients Requiring Oral Anticoagulation After Drug-Eluting Stent Implantation: The ISAR-TRIPLE Trial. J Am Coll Cardiol. 2015, 65, 1619–1629. [Google Scholar] [CrossRef]
- Lip, G.Y.; Windecker, S.; Huber, K.; Kirchhof, P.; Marin, F.; Ten Berg, J.M.; Document Reviewers; et al. Management of antithrombotic therapy in atrial fibrillation patients presenting with acute coronary syndrome and/or undergoing percutaneous coronary or valve interventions: A joint consensus document of the European Society of Cardiology Working Group on Thrombosis European Heart Rhythm Association (EHRA), European Association of Percutaneous Cardiovascular Interventions (EAPCI) and European Association of Acute Cardiac Care (ACCA) endorsed by the Heart Rhythm Society (HRS), Asia-Pacific Heart Rhythm Society (APHRS). Eur Heart J. 2014, 35, 3155–3179. [Google Scholar] [CrossRef] [PubMed]
- Kirchhof, P.; Benussi, S.; Kotecha, D.; Ahlsson, A.; Atar, D.; Casadei, B.; et al. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016, 37, 2893–2962. [Google Scholar] [CrossRef] [PubMed]
- Sarafoff, N.; Martischnig, A.; Wealer, J.; Mayer, K.; Mehilli, J.; Sibbing, D.; et al. Triple therapy with aspirin, prasugrel, and vitamin K antagonists in patients with drug-eluting stent implantation and an indication for oral anticoagulation. J Am Coll Cardiol. 2013, 61, 2060–2066. [Google Scholar] [CrossRef]
- Gibson, C.M.; Mehran, R.; Bode, C.; Halperin, J.; Verheugt, F.W.; Wildgoose, P.; et al. Prevention of Bleeding in Patients with Atrial Fibrillation Undergoing PCI. N Engl J Med. 2016, 375, 2423–2434. [Google Scholar] [CrossRef]
- Vranckx, P.; Valgimigli, M.; Windecker, S.; Steg, P.G.; Hamm, C.; Jüni, P.; et al. Long-term ticagrelor monotherapy versus standard dual antiplatelet therapy followed by aspirin monotherapy in patients undergoing biolimus-eluting stent implantation: Rationale and design of the GLOBAL LEADERS trial. EuroIntervention. 2016, 12, 1239–1245. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://clinicaltrials.gov/ct2/show/NCT01776424.
- Otto, C.M.; Kumbhani, D.J.; Alexander, K.P.; Calhoon, J.H.; Desai, M.Y.; Kaul, S.; et al. 2017 ACC Expert Consensus Decision Pathway for Transcatheter Aortic Valve Replacement in the Management of Adults With Aortic Stenosis: A Report of the American College of Cardiology Task Force on Clinical Expert Consensus Documents. J Am Coll Cardiol. 2017, 69, 1313–1346. [Google Scholar] [CrossRef]
- Cerrato, E.; Nombela-Franco, L.; Nazif, T.M.; Eltchaninoff, H.; Søndergaard, L.; Ribeiro, H.B.; et al. Evaluation of current practices in transcatheter aortic valve implantation: The WRITTEN (WoRldwIde TAVI ExperieNce) survey. Int J Cardiol. 2017, 228, 640–647. [Google Scholar] [CrossRef] [PubMed]
- Ussia, G.P.; Scarabelli, M.; MulȲ, M.; Barbanti, M.; Sarkar, K.; Cammalleri, V.; et al. Dual antiplatelet therapy versus aspirin alone in patients undergoing transcatheter aortic valve implantation. Am J Cardiol. 2011, 108, 1772–1776. [Google Scholar] [CrossRef] [PubMed]
- Rodés-Cabau, J.; Masson, J.B.; Welsh, R.C.; Garcia Del Blanco, B.; Pelletier, M.; Webb, J.G.; et al. Aspirin Versus Aspirin Plus Clopidogrel as Antithrombotic Treatment Following Transcatheter Aortic Valve Replacement With a Balloon-Expandable Valve: The ARTE (Aspirin Versus Aspirin + Clopidogrel Following Transcatheter Aortic Valve Implantation) Randomized Clinical Trial. JACC Cardiovasc Interv. 2017, 10, 1357–1365. [Google Scholar] [CrossRef]
- Windecker, S.; Tijssen, J.; Giustino, G.; Guimarȧes, A.H.; Mehran, R.; Valgimigli, M.; et al. Trial design: Rivaroxaban for the prevention of major cardiovascular events after transcatheter aortic valve replacement: Rationale and design of the GALILEO study. Am Heart J. 2017, 184, 81–87. [Google Scholar] [CrossRef]

| Oral administration | Intravenous administration | |||
| Clopidogrel | Prasugre! | Ticagrelor | Cangrelor | |
| Drug class—antiplatelet mechanism | Thienopyridine P2Y12 inhibitor | Thienopyridine P2Y12 inhibitor | Cyclopentyltriazolopyrimidine P2Y12 inhibitor | ATP analogue— ADP P2Y12 inhibitor |
| Loading/maintenance dose | 300–600 mg / 75 mg once daily | 60 mg / 10 mg once daily | 180 mg / 90 mg twice daily | 30 pg/kg bolus / 4 pg/kg/min infusion |
| Reversibility | Irreversible | Irreversible | Reversible | Reversible |
| Bio-activation | prodrug, variable cytochrome P450 metabolism | prodrug, predictable cytochrome P450 metabolism | Active drug | Active drug |
| Onset of action | 2–6 hours | 30 min. | 30 min. | 2 min. |
| Duration of action | 3–10 days | 7–10 days | 3–5 days | 1–2 hours |
| Withdrawal before surgery | 5 days | 7 days | 5 days | 1 hour |
| Cost | 740 CHF/year | 1135 CHF/year | 1354 CHF/year | Hospital administration only |
| STEMI |
|---|
| Routine pre-hospital pretreatment cannot be recommended for patients with STEMI over the in-lab administration of the drug since the two strategies had similar outcomes. |
| It can be advisable to administer potent and rapidly acting antiplatelet agents (prasugrel or ticagrelor) in the emergency department (i.e., ambulance) once the diagnosis of STEMI is confirmed and the patient proceeds to primary PCI. |
| NSTEMI |
| It is advisable to administer a potent and rapidly acting antiplatelet agent (prasugrel or ticagrelor) once the coronary anatomy is known (and the patient proceeds to immediate PCI). |
| If prasugrel or ticagrelor are contraindicated, pretreatment with clopidogrel before coronary angiography may be advisable for patients with low bleeding risk and a high likelihood for immediate PCI, especially if radial access is planned. |
| DAPT 3–6 months | DAPT 12 months | RR | |
|---|---|---|---|
| ST* rate (%) | 0.5 | 0.4 | 0.1 |
| Pooled MI+ (%) | 1.7 | 1.5 | 0.2 |
| Major bleeding (%) | 0.4 | 0.8 | 0.4 |
| Death rate (%) | 1.7 | 1.9 | 0.2 |
| Increased ischaemic risk or risk of stent thrombosis (may favour longer-duration DAPT) |
|---|
| Recurrent ischaemic episode on DAPT |
| ACS presentation in young patients |
| LV dysfunction |
| High vascular burden |
| Chronic stable kidney disease |
| Additional stent factors |
| First-generation DES |
| Stent undersizing |
| Bifurcation stent |
| Stent-in-stent |
| Increased bleeding risk (may favor shorter-duration DAPT) |
| Very old patients |
| Short life expectancy |
| Poor DAPT adherence |
| End-stage renal failure |
| Malignancy |
| Short term candidates for high risk surgery |
| Severe anaemia |
| History of prior bleeding |
| Major haematological disorders |
| Oral anticoagulation |
| Low body weight |
© 2017 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Biasco, L.; Montrasio, G.; Moccetti, M.; Pedrazzini, G. Current Trends in Dual Antiplatelet Therapy: A 2017 Update. Cardiovasc. Med. 2017, 20, 0499. https://doi.org/10.4414/cvm.2017.00499
Biasco L, Montrasio G, Moccetti M, Pedrazzini G. Current Trends in Dual Antiplatelet Therapy: A 2017 Update. Cardiovascular Medicine. 2017; 20(7-8):0499. https://doi.org/10.4414/cvm.2017.00499
Chicago/Turabian StyleBiasco, Luigi, Giulia Montrasio, Marco Moccetti, and Giovanni Pedrazzini. 2017. "Current Trends in Dual Antiplatelet Therapy: A 2017 Update" Cardiovascular Medicine 20, no. 7-8: 0499. https://doi.org/10.4414/cvm.2017.00499
APA StyleBiasco, L., Montrasio, G., Moccetti, M., & Pedrazzini, G. (2017). Current Trends in Dual Antiplatelet Therapy: A 2017 Update. Cardiovascular Medicine, 20(7-8), 0499. https://doi.org/10.4414/cvm.2017.00499




