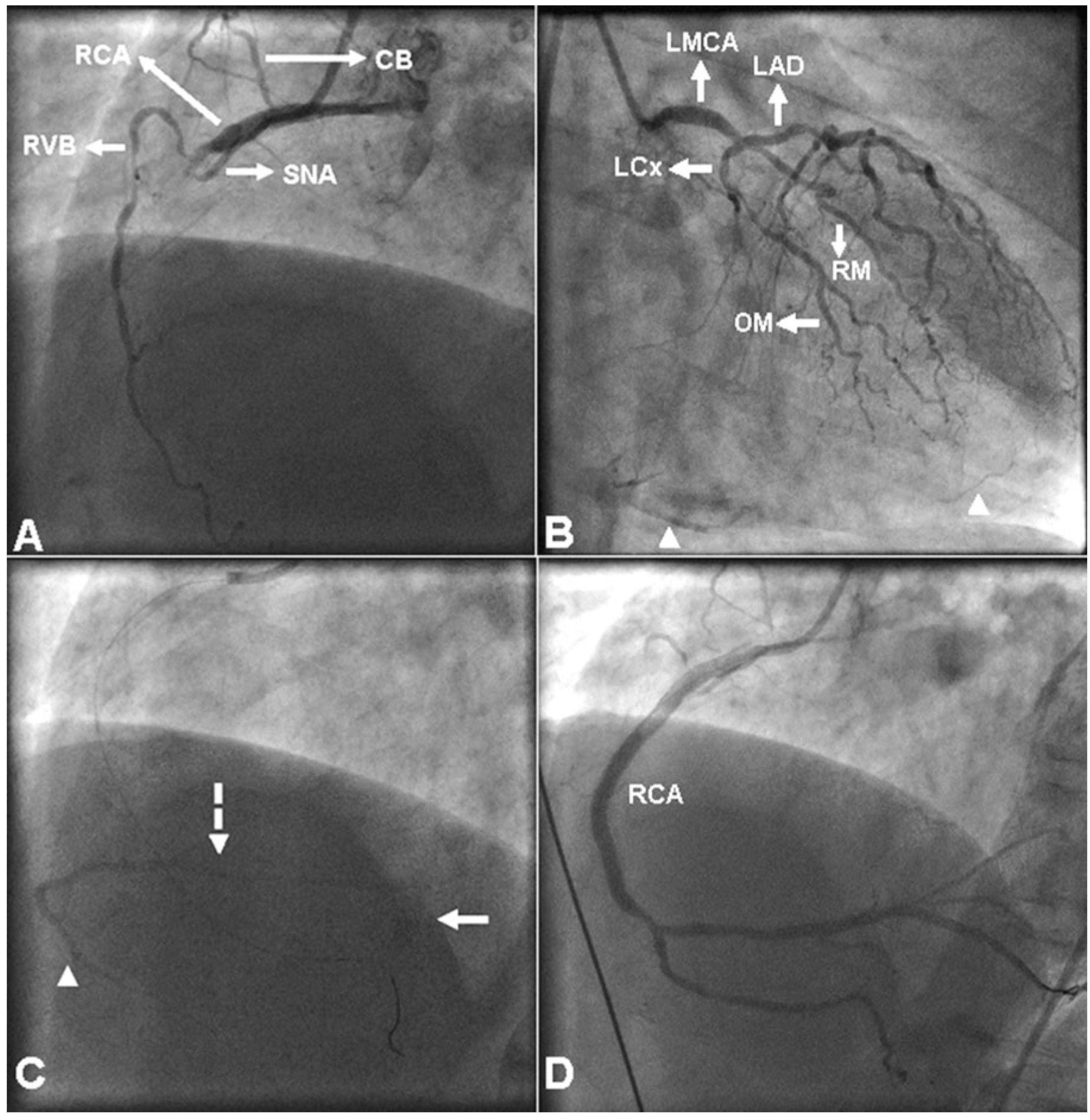
A 66-year-old man presented with substernal chest pain of one hour’s duration and electrocardiographic evidence of acute inferior wall ST-segment elevation myocardial infarction. He underwent emergency coronary angiography that showed total occlusion of the mid right coronary artery (RCA) (
Figure 1A) just beyond the origins of a right ventricular branch (RVB) and the sinus node artery (SNA), and significantly obstructive lesions in the distal left main coronary artery, the proximal left anterior descending artery and the obtuse marginal artery. Collateral circulation (Rentrop grade II) to the distal RCA branches from the left coronary artery was also noted (
Figure 1B). Initial angiography of the RCA also showed a peculiar, faintly visualised vessel in an area corresponding to the acute margin of the heart, which was initially assumed to be the distal RCA being collateralised from the RVB (moving image 1) (You will find the videos the website www. cardiovascmed.ch in the section «Online only».). During subsequent percutaneous coronary intervention, the guide wire tracked up the distal RCA outside the faintly visualised vessel, which was seen as comprising two branches and a drain point (
Figure 1C; moving image 2 and moving image 3); it was thus recognised as a coronary vein. Percutaneous coronary intervention was completed with delivery of three bare-metal stents across the mid RCA lesion and two bare-metal stents across a lesion from the distal RCA to posterior left ventricular branch. Final RCA angiography disclosed Thrombolysis in Myocardial Infarction (TIMI) grade III flow, occlusion of the RVB, subocclusion of the SNA and disappearance of the previously seen coronary vein (
Figure 1D and moving image 4). The patient had an uneventful hospital course and was referred for surgical revascularisation of the left coronary artery lesions.
Demonstration of a coronary vein in the distribution of an acutely occluded coronary artery is, in our experience, an unexpected and potentially misleading finding. To the best of our knowledge, there has to date been only one similar publication, by Anzai et al. [
1], who reported a coronary vein following a course parallel to a proximally occluded RCA, giving the false impression of spontaneous reperfusion; the vein was no longer visible after recanalisation of the RCA. Scrutiny of the angiographic presentation of the portion of the coronary venous system described here, revealed that the trunk coursing parallel to the distal RCA in the right atrioventricular sulcus corresponded to the small cardiac vein, which received the right marginal vein at the area of the acute margin of the heart and terminated in the coronary sinus [
2]. Like Anzai et al. [
1], we initially misidentified the coronary vein as the distal RCA being collateralised from the RVB, and what made us recognise it was the observation of its draining point. The conus artery supplying the right ventricular infundibulum, the SNA supplying the sinus node and adjacent right atrial wall and a RVB supplying the anterior right ventricular wall arose proximal to the occlusion site of the RCA, thereby allowing uninterrupted perfusion of their dependent myocardial areas. The small cardiac vein drains most of the walls of the right atrium and the diaphragmatic surface of the right ventricle, whereas the right marginal vein drains the anterior wall of the right ventricle [
2]. Furthermore, coronary sinus flow has been shown to decrease during acute RCA occlusion [
3]; therefore, we presumed that clearance of contrast material from the small cardiac vein that drained the venous return from the walls of the right atrium and the anterior wall of the right ventricle being supplied by the patent proximal RCA branches was delayed, thereby facilitating its opacification. In addition to being an angiographic peculiarity, a coronary vein seen downstream of an acutely occluded coronary artery should not be misidentified as a collateralised culprit artery or lead to confusion regarding the position of the guiding wire.