Clinical Determinants of Adrenal Vein Sampling Success
Summary
Background
Methods
Radiological imaging
Adrenal vein sampling
Samples
Selectivity and lateralisation indexes
Statistic analysis
Results
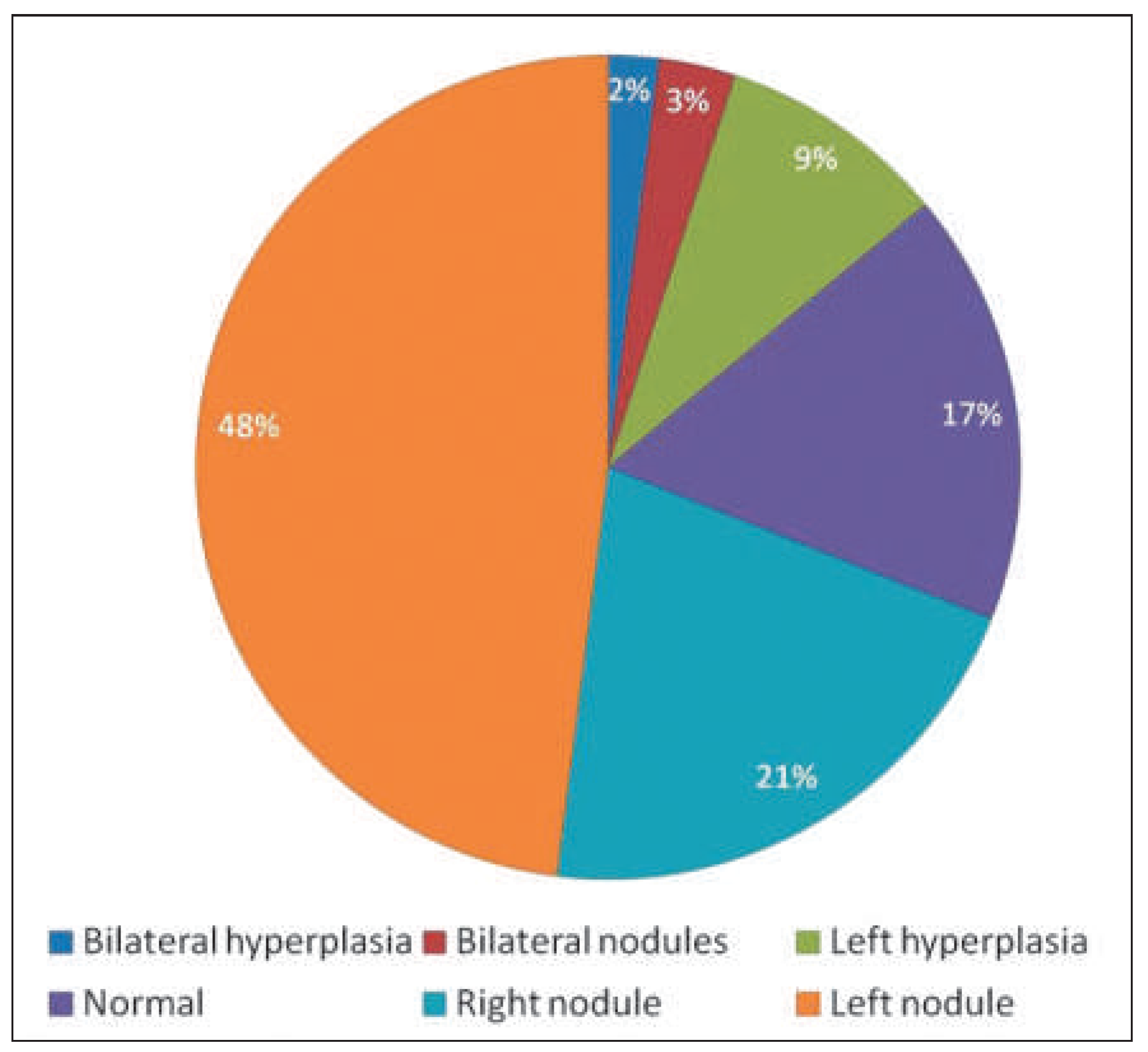
CT and MRI results
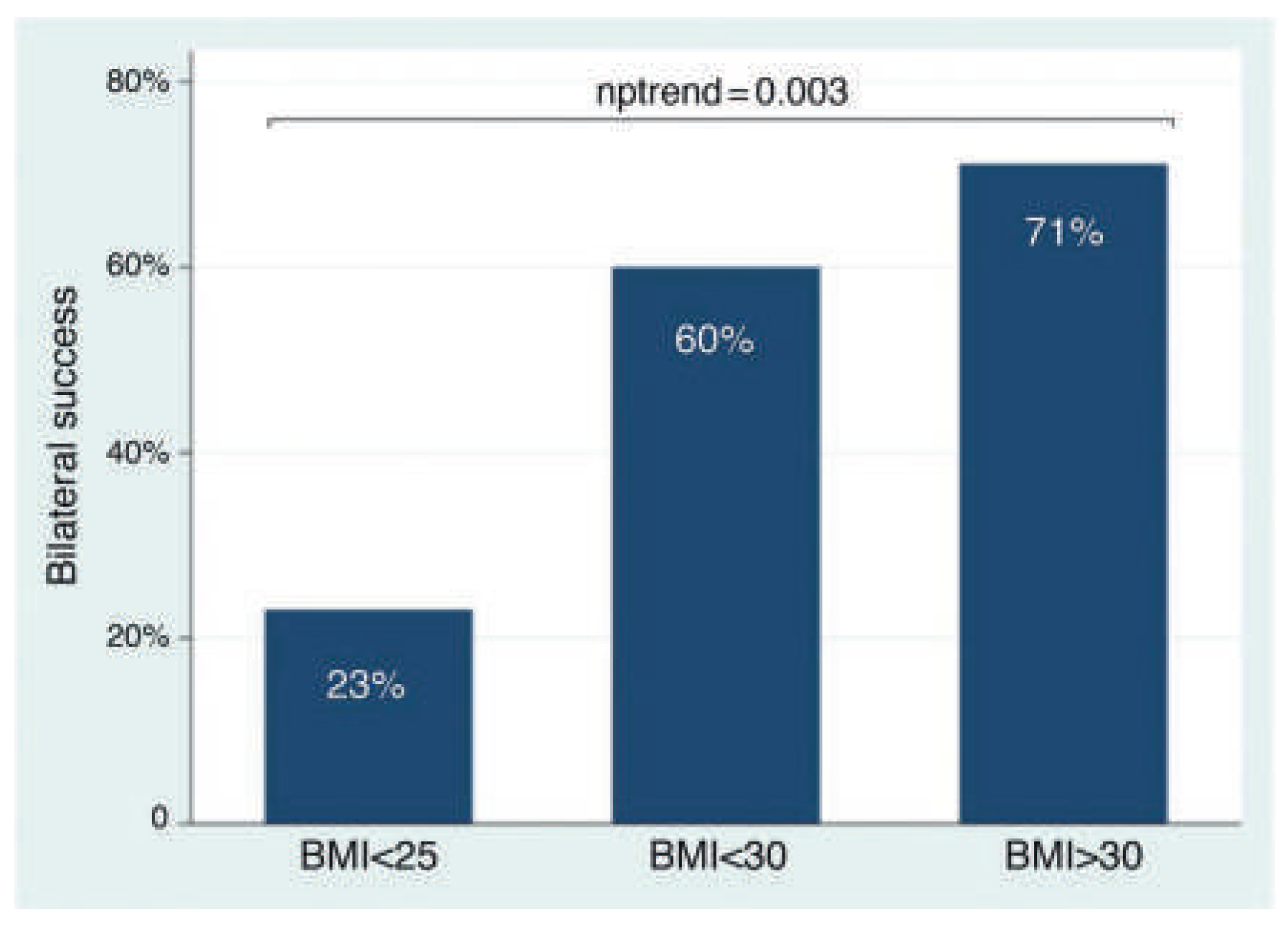
AVS success rate and clinical determinants
Comparison between AVS and adrenal imaging
Surgery and histopathological results (Table 4)
| Adrenalectomy (n) | 48% (30/68) |
| Right adrenalectomy | 40%(12/30) |
| Left adrenalectomy | 60% (18/30) |
| Histology reports (n) | 30/30 |
| Adrenal adenoma | 74% |
| Adrenal hyperplasia | 20% |
| Normal adrenal | 7% |
Discussion
AVS and CT/MRI adrenal imaging discrepancies
Limitations
Conclusion
Disclosure statement
References
- Rossi, G.P.G.; Bernini, C.; Caliumi, G.; Desideri, B.; Fabris, C. ; Ferri; et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006, 48(11), 2293–300. [Google Scholar] [PubMed]
- Calhoun, D.A.; Nishizaka, M.K.; Zaman, M.A.; Thakkar, R.B.; Weissmann, P. Hyperaldosteronism among black and white subjects with resistant hypertension. Hypertension. 2002, 40(6), 892–6. [Google Scholar]
- Strauch, B.; Zelinka, T.; Hampf, M.; Bernhardt, R.; Widimsky Jr, J. Prevalence of primary hyperaldosteronism in moderate to severe hypertension in the Central Europe region. J Hum Hypertens. 2003, 17(5), 349–52. [Google Scholar] [CrossRef]
- Savard, S.; Amar, L.; Plouin, P.-F.; Steichen, O. Cardiovascular Complications Associated With Primary Aldosteronism: A Controlled Cross-Sectional Study. Hypertension. 2013, 62(2), 331–6. [Google Scholar] [PubMed]
- Sawka, A.M.; Young, W.F.; Thompson, G.B.; Grant, C.S.; Farley, D.R.; Leibson, C.; et al. Primary aldosteronism: factors associated with normalization of blood pressure after surgery. Ann Intern Med. 2001, 135(4), 258–61. [Google Scholar] [CrossRef]
- van der Linden, P.; Steichen, O.; Zinzindohoue, F.; Plouin, PF. Blood pressure and medication changes following adrenalectomy for unilateral primary aldosteronism: a follow-up study. J Hypertens. 2012, 30(4), 761–9. [Google Scholar] [CrossRef]
- Rossi, G.P.; Cesari, M.; Cuspidi, C.; Maiolino, G.; Cicala, M.V.; Bisogni, V.; et al. Long-Term Control of Arterial Hypertension and Regression of Left Ventricular Hypertrophy With Treatment of Primary Aldosteronism. Hypertension. 2013, 62(1), 62–9. [Google Scholar] [CrossRef]
- Ishidoya, S.; Kaiho, Y.; Ito, A.; Morimoto, R.; Satoh, F.; Ito, S.; et al. Singlecenter outcome of laparoscopic unilateral adrenalectomy for patients with primary aldosteronism: lateralizing disease using results of adrenal venous sampling. Urology. 2011, 78(1), 68–73. [Google Scholar] [CrossRef]
- Rossi, G.P.; Auchus, R.J.; Brown, M.; Lenders, J.W.; Naruse, M.; Plouin, P.F.; et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension 2014, 63(1), 151–60. [Google Scholar] [CrossRef]
- Daunt, N. Adrenal vein sampling: how to make it quick, easy, and successful. Radiographics. 2005, 25 Suppl1, S143–58. [Google Scholar] [CrossRef] [PubMed]
- Harvey, A.; Pasieka, J.L.; Kline, G.; So, B. Modification of the protocol for selective adrenal venous sampling results in both a significant increase in the accuracy and necessity of the procedure in the management of patients with primary hyperaldosteronism. Surgery. 2012, 152(4), 643–9, discussion 649–51. [Google Scholar] [CrossRef]
- Mulatero, P.C.; Bertello, N.; Sukor, R.; Gordon, D.; Rossato, N.; Daunt; et al. Impact of different diagnostic criteria during adrenal vein sampling on reproducibility of subtype diagnosis in patients with primary aldosteronism. Hypertension 2010, 55(3), 667–73. [Google Scholar] [CrossRef]
- Young, W.F.; Stanson, A.W. What are the keys to successful adrenal venous sampling (AVS) in patients with primary aldosteronism? Clin Endocrinol. (Oxf), 2009, 70(1), 14–7. [Google Scholar]
- Lambert, D.M.; Marceau, S.; Forse, R.A. Intra-abdominal pressure in the morbidly obese. Obes Surg. 2005, 15(9), 1225–32. [Google Scholar] [CrossRef]
- Sugerman, H.J. Effects of increased intra-abdominal pressure in severe obesity. Surg Clin North Am. 2001, 81(5), 1063–75, vi. [Google Scholar]
- Barnes, G.E.; Laine, G.A.; Giam, P.Y.; Smith, E.E.; Granger, H.J. Cardiovascular responses to elevation of intra-abdominal hydrostatic pressure. Am J Physiol. 1985, 248(2Pt2), R208–13. [Google Scholar] [CrossRef] [PubMed]
- Vonend, O.N.; Ockenfels, X.; Gao, B.; Allolio, K.; Lang, K. ; Mai ; et al. Adrenal venous sampling: evaluation of the German Conn’s registry. Hypertension. 2011, 57(5), 990–5. [Google Scholar] [CrossRef]
- Lethielleux, G.; Amar, L.; Raynaud, A.; Plouin, P.F.; Steichen, O. Influence of diagnostic criteria on the interpretation of adrenal vein sampling. Hypertension. 2015, 65(4), 849–54. [Google Scholar] [CrossRef] [PubMed]
- Rossi, G.P.; Barisa, M.; Allolio, B.; Auchus, R.J.; Amar, L.; Cohen, D.; et al. The Adrenal Vein Sampling International Study (AVIS) for identifying the major subtypes of primary aldosteronism. J Clin Endocrinol Metab. 2012, 97(5), 1606–14. [Google Scholar]
- Reardon, M.A.; Angle, J.F.; Abi-Jaoudeh, N.; Bruns, D.E.; Haverstick, D.M.; Matsumoto, A.H.; et al. Intraprocedural cortisol levels in the evaluation of proper catheter placement in adrenal venous sampling. J Vasc Interv Radiol. 2011, 22(11), 1575–80. [Google Scholar]
- Rossi, E.; Regolisti, G.; Perazzoli, F.; Negro, A.; Grasselli, C.; Santi, R.; et al. Intraprocedural cortisol measurement increases adrenal vein sampling success rate in primary aldosteronism. Am J Hypertens. 2011, 24(12), 1280–5. [Google Scholar] [CrossRef] [PubMed]
- Dekkers, T.; Deinum, J.; Schultzekool, L.J.; Blondin, D.; Vonend, O.; Hermus, A.R.; et al. Plasma metanephrine for assessing the selectivity of adrenal venous sampling. Hypertension. 2013, 62(6), 1152–7. [Google Scholar] [CrossRef] [PubMed]
- Onozawa, S.; Murata, S.; Tajima, H.; Yamaguchi, H.; Mine, T.; Ishizaki, A.; et al. Evaluation of right adrenal vein cannulation by computed tomography angiography in 140 consecutive patients undergoing adrenal venous sampling. Eur J Endocrinol. 2014, 170(4), 601–8. [Google Scholar] [CrossRef]
- Kempers, M.J.; Lenders, J.W.; van Outheusden, L.; van der Wilt, G.J.; Schultze Kool, L.J.; Hermus, A.R.; et al. Systematic review: diagnostic procedures to differentiate unilateral from bilateral adrenal abnormality in primary aldosteronism. Ann Intern Med. 2009, 151(5), 329–37. [Google Scholar] [CrossRef] [PubMed]


| n (found) | ||
| Gender, male/female | 35/33 | 68 |
| Age, years | 47.2 ± 12.1 | 68 |
| BMI, kg/m2 | 29 ± 5.6 | 66 |
| Potassium, mmol/l | 3.26 ± 0.55 | 66 |
| Creatinine, mmol/l | 75.5 ± 18.1 | 63 |
| Office SBP, mm Hg | 169 ± 28 | 25 |
| Office DBP, mm Hg | 105 ± 14 | 25 |
| Number of antihypertensive drugs | 2.1 ± 1.2 | 68 |
| PRA, ng/ml/h | 0.06 [0.04; 0.24] | 44 |
| PAC, pg/ml | 250 [190; 442] | 39 |
| Success | |
| Age | 0.18 (0.15) |
| Sex | 0.36 (0.0039) |
| BMI | 0.54 (0.0001) |
| Office SBP | 0.17 (0.42) |
| Office DBP | 0.026 (0.90) |
| Creatinine | 0.25 (0.048) |
| Potassium | 0.22 (0.080) |
| ARR | 0.24 (0.13) |
| Dependant variable | Predictor variables | Coefficient | (95% confidence interval) | p-value |
| Bilateral AVS success rate (%) | BMI | 0.048 | (0.016; 0.081) | 0.04 |
| Age | –0.0049 | (–0.020; 0.010) | 0.52 | |
| Sex | 0.14 | (–0.27; 0.55) | 0.49 | |
| Creatinine | 0.0047 | (–0.0057; 0.015) | 0.37 | |
| Adjusted R2 = 0.22 |
© 2015 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Berney, M.; Maillard, M.; Doenz, F.; Matter, M.; Pechère-Bertschi, A.; Burnier, M.; Wuerzner, G. Clinical Determinants of Adrenal Vein Sampling Success. Cardiovasc. Med. 2015, 18, 246. https://doi.org/10.4414/cvm.2015.00352
Berney M, Maillard M, Doenz F, Matter M, Pechère-Bertschi A, Burnier M, Wuerzner G. Clinical Determinants of Adrenal Vein Sampling Success. Cardiovascular Medicine. 2015; 18(9):246. https://doi.org/10.4414/cvm.2015.00352
Chicago/Turabian StyleBerney, Maxime, Marc Maillard, Francesco Doenz, Maurice Matter, Antoinette Pechère-Bertschi, Michel Burnier, and Gregoire Wuerzner. 2015. "Clinical Determinants of Adrenal Vein Sampling Success" Cardiovascular Medicine 18, no. 9: 246. https://doi.org/10.4414/cvm.2015.00352
APA StyleBerney, M., Maillard, M., Doenz, F., Matter, M., Pechère-Bertschi, A., Burnier, M., & Wuerzner, G. (2015). Clinical Determinants of Adrenal Vein Sampling Success. Cardiovascular Medicine, 18(9), 246. https://doi.org/10.4414/cvm.2015.00352




