Case report
A 16-year-old girl presented with a history of three episodes of syncope during physical activity. She was in full-time ballet training at a specialised ballet school and trained several hours per day. These three episodes of syncope happened around 15 to 20 minutes after starting medium to high-impact training, and were preceded by prodromal symptoms like fatigue, lightheadedness, blurred vision and nausea, without chest pain or palpitations. The loss of consciousness lasted less than 1 minute. She denied any injury as a consequence of syncope. No tonic clonic activity or postictal phase was observed.
The patient denied the use of drugs and was not taking any medication. She reported having had gastroenteritis 1 month before the episodes started. She had occasionally felt the same prodromal symptoms during training, with disappearance of these symptoms without interrupting her training. Although she reported a clearly small daily fluid intake (often as little as 1 L), she denied any past or present associated eating disorder, which was confirmed by her parents. Her weight was stable during the last year. She also denied amenorrhoea, which should have raised the question of a “female athlete triad”. There was no past history of syncope. Her family history was negative for syncope or cardiovascular disease.
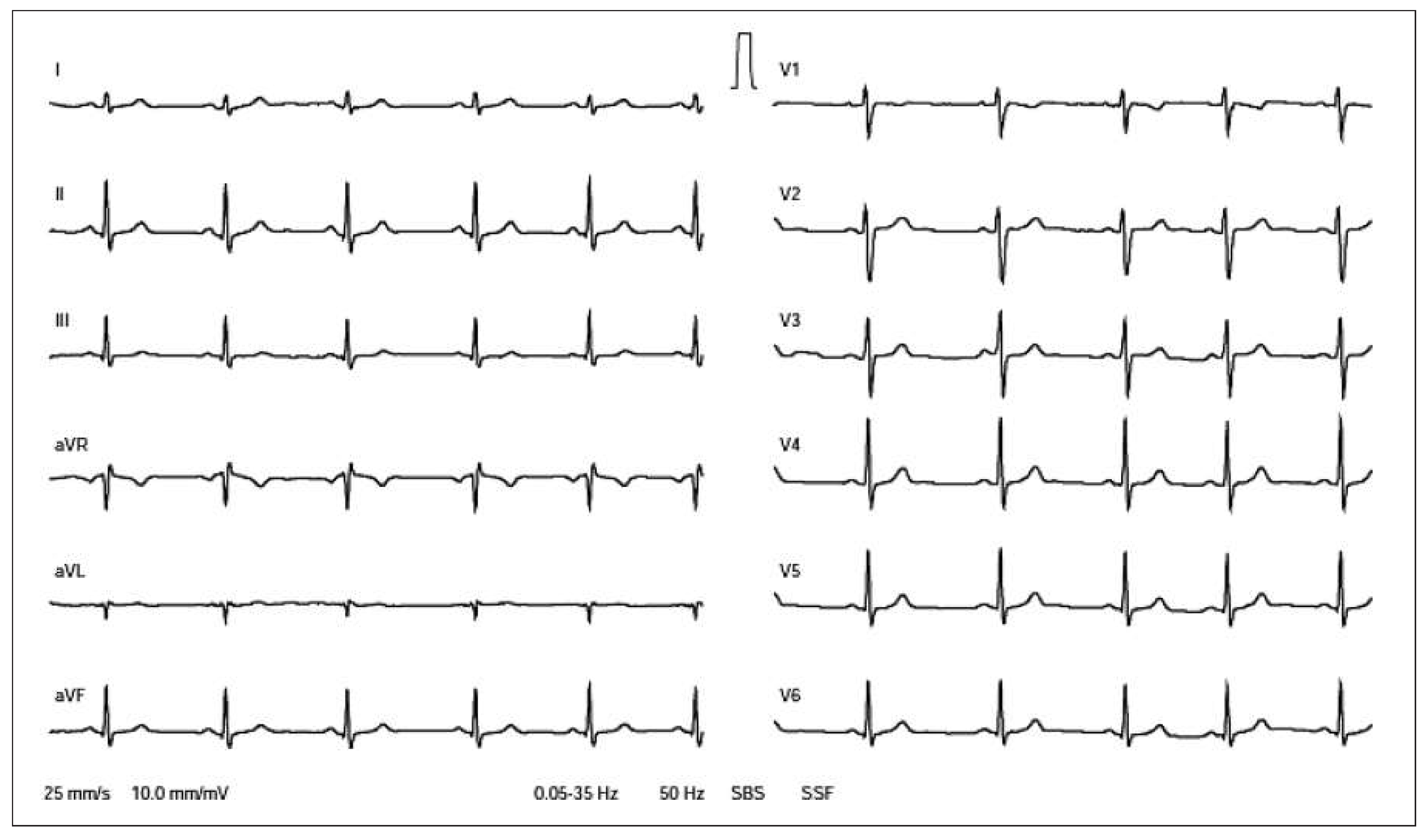
Physical examination was normal, except for a low Body Mass Index of 17.2 kg/m2, with a height of 158 cm and weight of 43 kg. The ECG showed a normal sinus rhythm with a heart rate of 68 bpm (
Figure 1). Transthoracic echocardiography showed normal biventricular morphology and function, no valvular disease, and no signs of left ventricular outflow tract or supra-aortic obstruction. A treadmill test was performed (
Figure 2), which showed a normal rise in heart rate and blood pressure during the first 8 minutes. After 12 minutes, at a velocity of 5.5 km/h and slope of 10% (8.4 METs), the typical prodromal symptoms occurred. This was associated with a drop in blood pressure from 166/80 to 89/64 mm Hg and a increase of the heart rate to 166 bpm. Exercise was stopped after 13 minutes and during a recovery phase (velocity 2 km/h; no slope) with a duration of 5 minutes, her blood pressure gradually recovered with improvement of her symptoms. There were no significant electrocardiographic changes during treadmill testing.
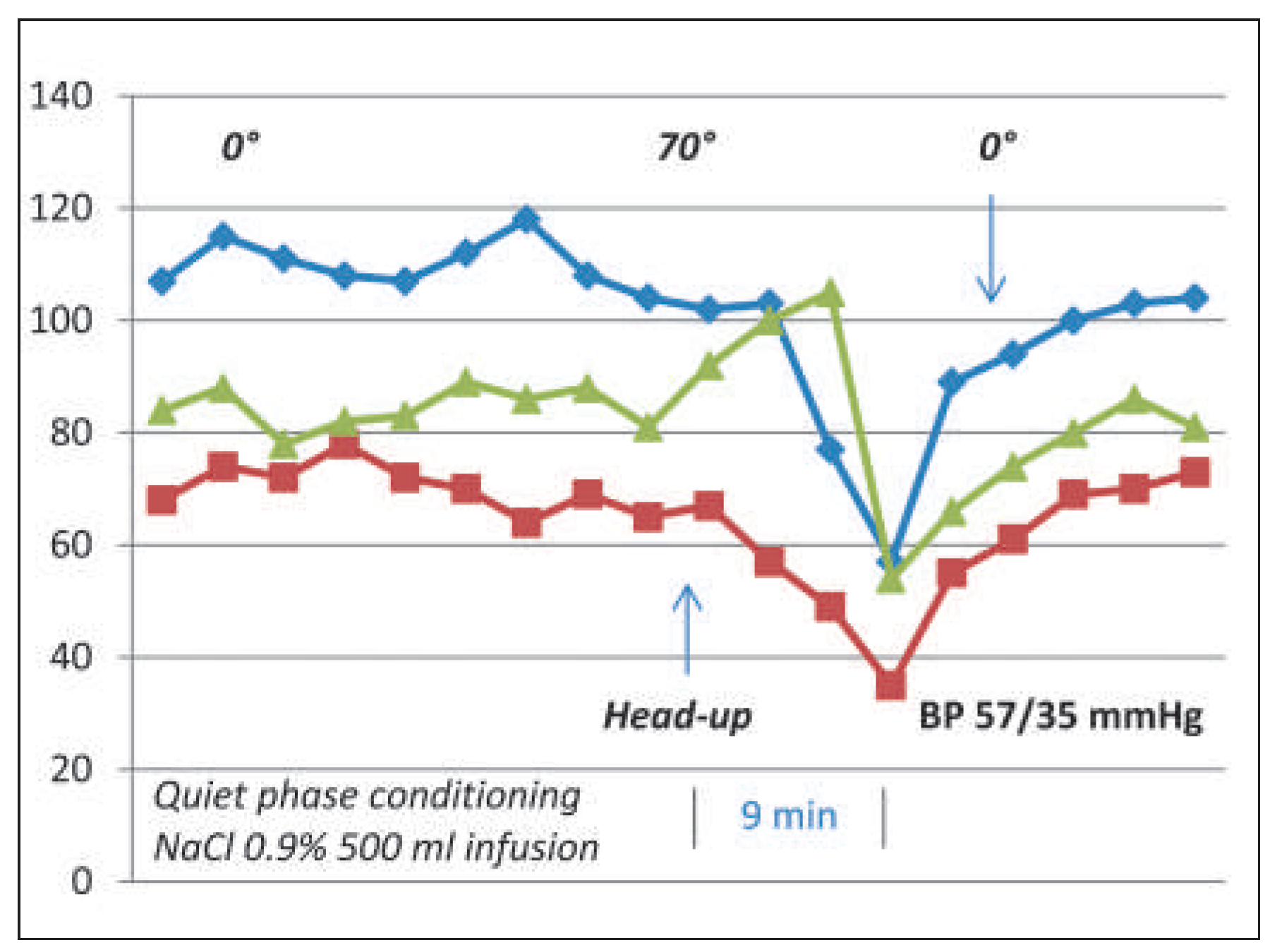
Cardiac magnetic resonance imaging was then performed and confirmed the normal dimensions and function of the heart, including a normal coronary artery origin and course. There was no late gadolinium enhancement as a sign of a postmyocarditis or ischaemic scar. Head-up tilt-test (HUTT) was then performed (
Figure 3). After 9 minutes in an upright position, a drop in blood pressure from 103/57 to 57/35 mm Hg and, after an increase in heart rate, sinus bradycardia (54 bpm) were observed, again provoking the prodromal symptoms of the patient, followed by a brief syncopal spell with rapid recovery after returning to a flat position. This pattern was consistent with a mixed vasodepressor and cardio-inhibitory vasovagal reaction.
Based on the abovementioned findings, exerciseinduced vasodepressor syncope was diagnosed. An increase was recommended in daily fluid and salt intake, which had certainly been inadequate considering her strenuous training programme. During follow-up, the patient still occasionally experienced her typical prodromal symptoms during exercice, but no more syncopal episodes occurred.
Short review and discussion
This case illustrates a diagnosis that may be hard to demonstrate in clinical practice because of the potential poor reproducibility of the exercise test to provoke hypotension [5]. Although most of the potentially fatal causes of exercise-induced syncope are usually well known and have a well-defined standard of care based on guidelines, vasodepressor type reflex syncope has only been described in a few case reports since 1993 [5,6,7,8,9], and, maybe because of its good prognosis and low prevalence, no standard management recommandations can be found about this topic.
Definitions and prevalence
Exercise-related syncope is a general term used to describe post-exercise syncope as well as syncope occurring during exercise. Although the clinical distinction between these two forms of presentation is critical, they are often mixed in the medical literature (as in some references used for this manuscript). This can be explained by the fact that both forms may share some identical physiopathological mechanisms. Syncope occuring during exercise is and should always be feared by the clinician because it is known to be linked with significant and life-threatening pathology that should always be ruled out (
Table 1) [1].
Aher these serious causes have been ruled out, it should be considered that the syncope may be “neurally” mediated, or “neurocardiogenic”, in analogy to vasovagal syncope (
Figure 4). Two different types have been described: a vasodepressor type and a cardioinhibitory type. Exercise-induced vasodepressor syncope (EIVS) has been described in case series published between 1993 and 2002 [4,5,6,7,8,9]. A cardioinhibitory type with prolonged asystole has also been reported, with a first case described as early as 1947 [12].
A third entity named “exercise-associated collapse” is also found in the sport literature [2]. It occurs immediately after completing a race or stopping exercise and is commonly observed at endurance events. The athlete is unable to stand or walk as a result of lightheadedness, faintness, dizziness or syncope. The mechanism postulated is an abrupt decrease in venous return owing to the relaxation of the muscular pump when activity is stopped, with lower extremity pooling of blood and impairment of cardiac baroreflexes. Training-related expansion of vascular volume is associated with a decreased heart rate response to baroreceptor stimulation and an exercise-induced change in cardiac filling volume and output may lead to a resetting of the cardiopulmonary baroreflex. For these reasons, trained individuals may depend more on maintenance of venous return to maintain upright body position [1,2].
The exact prevalence of EIVS is unknown, but seems to be low, probably accounting for fewer than 2% of healthy young patients referred for unexplained syncope [3]. Most reported cases are seen in trained individuals (young athletes) and the typical patient is the young, female athlete.
Physiopathology
A few hypotheses have been described to account for EIVS, which are summarised in
Figure 5. These mechanisms have only been partially demonstrated [3] and there is no clear discriminator between exercise or post-exercise vasodepressor response.
The main mechanism seems to be an inappropriate peripheral vasodilation (or lack of vasoconstriction), which could be triggered by the activation of intraventricular mechanoreceptors sensitised by high circulating catecholamines in susceptible individuals [3,5,6,8,9]. A blunted vasoconstriction during exercise has also been described and could be responsible for supplementary venous pooling in non-exercising regions [5]. The final result of these mechanisms is a profound hypotension with cerebral hypoperfusion, and, as a result, the occurence of syncope.
In the post-exercise situation, the loss of the muscle pump with venous pooling implies also a sudden reduction in venous return to the heart, with forceful ventricular contraction and activation of c-fibre mechanoreceptors which trigger the vagal afferent pathway to the brainstem (this belongs to the ancient “BezoldJarisch reflex”), responsible for vasodilatation and the (sometimes) associated bradycardia [3,5,10].
A major part of the patients suffering from this condition seem also to demonstrate a positive head-up tilt response [4].
Investigations
Although no standard recommendations exist for this specific condition, the initial work-up should be the same as for any syncope. A cardiological work-up with a 12-lead ECG, echocardiography and a treadmill test should be performed to rule out structural heart disease responsible for a potentially life-threatening condition. The poor reproductibility of exercise-induced hypotension observed during a treadmill test may encourage repetition of the exercise test if initially normal [5]. A head-up tilt-test (HUTT) with pharmacological provocation should be considered to assess susceptibility to neurally mediated hypotension or bradycardia, which is a common finding in such patients. In our case, we decided to also perform cardiac MRI to rule out a coronary anomaly. Whether cardiac MRI should be performed without the presence of chest pain or ischaemic ECG changes observed during the treadmill test is debatable. In the absence of structural heart disease or ECG abnormalities, an electrophysiologic study does not add any information [9].
Treatment and prognosis
Adequate fluid intake should be recommended. A fluid “loading dose” (1 L of fluids prior to exercise) may improve symptoms [13], but may be inconvenient. As in neurocardiogenic syncope, several medical treatments have been suggested, such as beta-blockers or disopyramide, with the idea of blocking inotropy and stimulation of ventricular mechanoreceptors. These two drugs have been shown to be beneficial in some case series, with reduction of syncope episodes in patients with documented vasodepressor response to HUTT [4]. However, no randomised study has been conducted to demonstrate this benefit. Because these same drugs have not been proven to have any beneficial effect in randomised controlled trials in vasovagal syncope, caution should be advised. For Swiss competition athletes, please refer to antidoping.ch.
The clinical course of patients suffering from exercise-induced vasodepressive syncope was favourable in the aforementioned case series, with symptom control most of the time. The only independent predictor of syncope recurrence was the number of exerciserelated syncopal events in the clinical history [4].
Patients can safely continue to participate in recreational or competitive athletic activities, with the exception of athletes in whom hypotension or syncope could be life threatening for themselves or others (e.g., climbing, swimming, diving, etc.). The patient should be made aware of these dangers and possibly advised to take appropriate additional safety measures, or, if not feasible, stop the activity associated with syncope.
Key points
− Exercise-induced vasodepressor syncope is a relatively rare pathology among patients suffering from exercise-induced syncope.
− Exercise-induced vasodepressor syncope should always remain a diagnosis of exclusion.
− Basic noninvasive tests should be performed (ECG, echocardiography, treadmill test, head-up tilt-test, and possibly imaging of the coronary arteries) to rule out a structural heart disease responsible for a potentially life-threatening condition.
− The supposed physiopathological mechanism of EIVS is an inappropriate peripheral vasodilation from the vagal afferent pathway triggered by the activation of intraventricular mechanoreceptors in susceptible subjects.
− The prognosis of EIVS remains favourable and symptoms can be controlled most of the time, with no need of prolonged interruption of the activity associated with syncope. The exception is the cardioinhibitory form with prolonged asystole, in case of which pacemaker implantation should be considered.
Disclosures
No financial support and no other potential conflict of interest relevant to this article was reported.

 Systolic BP (mmHg)
Systolic BP (mmHg)
 Diastolic BP (mmHg)
Diastolic BP (mmHg)  Heart Rate (/min)
Heart Rate (/min)