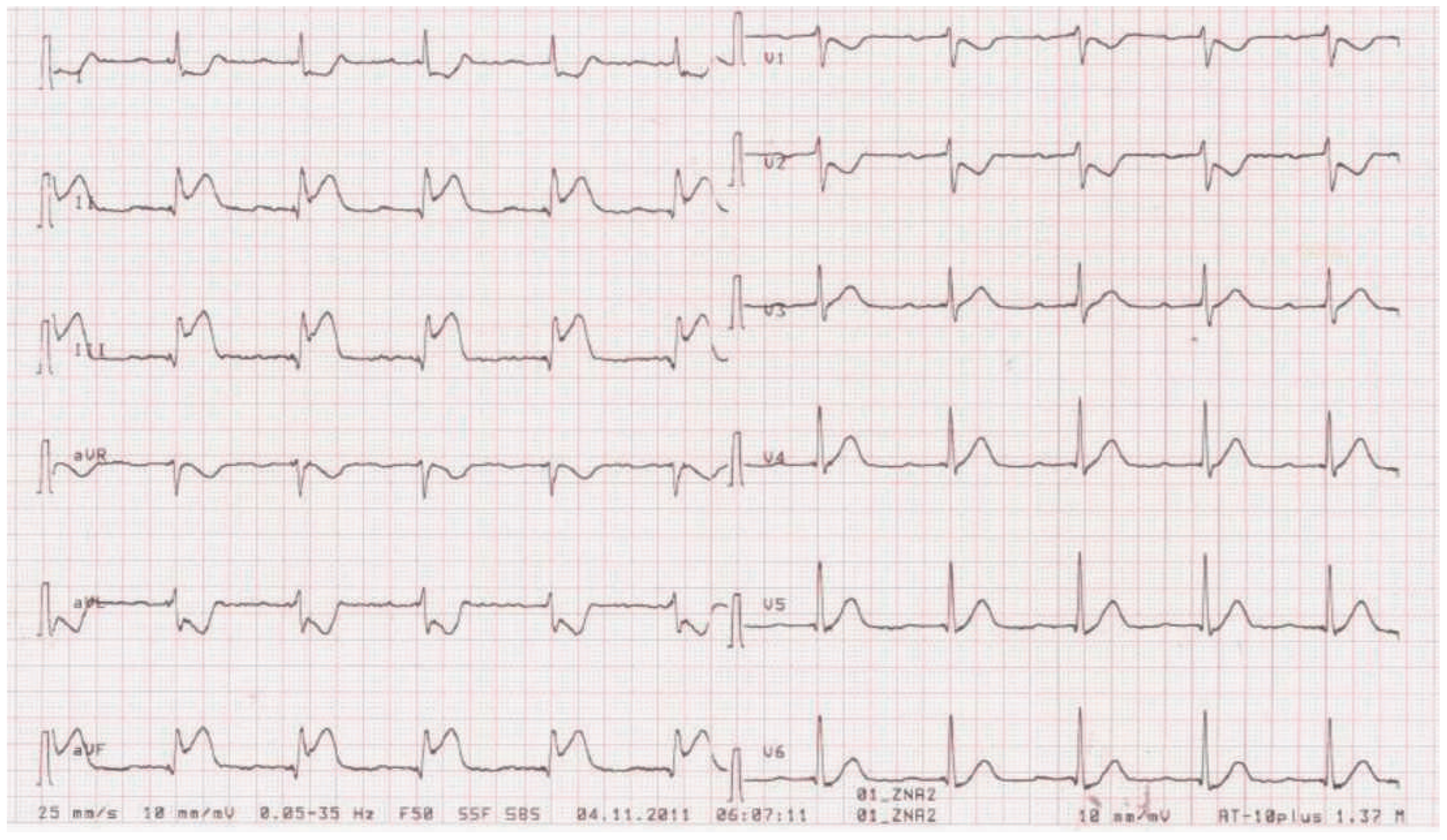
Figure 1.
Twelve-lead ECG of the patient on admission.
Figure 2.
Twelve-lead ECG of another patient with inferior ST-segment elevation myocardial infarction due to acute occlusion of the right coronary artery (RCA) and otherwise normal coronary arteries, showing a typical ECG pattern of an acute RCA infarct.
Figure 2.
Twelve-lead ECG of another patient with inferior ST-segment elevation myocardial infarction due to acute occlusion of the right coronary artery (RCA) and otherwise normal coronary arteries, showing a typical ECG pattern of an acute RCA infarct.
Figure 3.
Twelve-lead ECG of a patient with acute pericarditis, with widespread PQ segment depression and ST-segment elevation except in aVR.
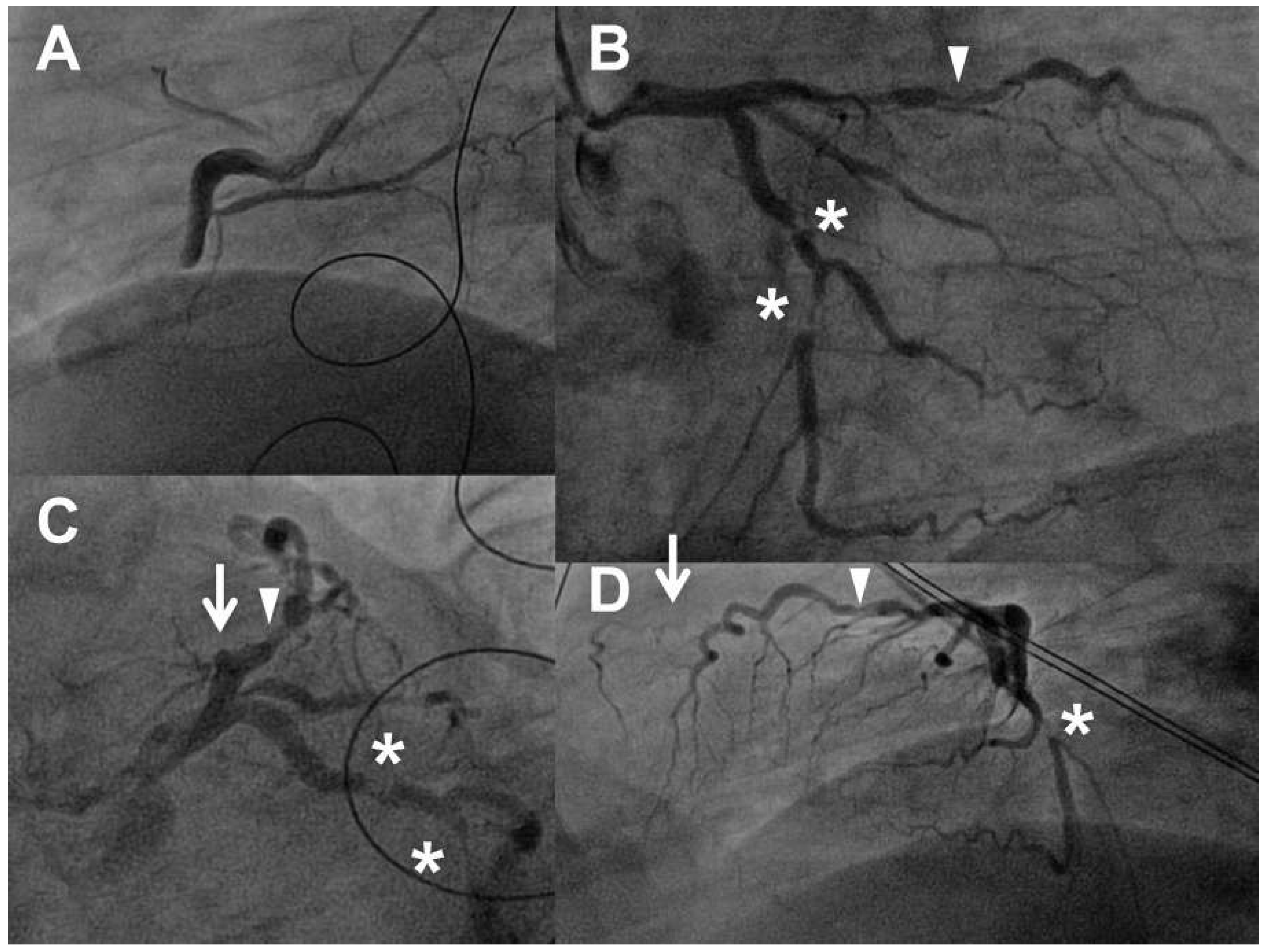
Figure 4.
Angiogram before percutaneous coronary intervention. Panel A, left anterior oblique (LAO) 60°: acute occlusion of the mid-right coronary artery (RCA). Panel B, right anterior oblique (RAO) 30%, caudal 20%: left circumflex artery (LCX) with two significant stenoses (asterisks), first diagonal branch with significant lesions (triangle), the left anterior descending artery (LAD) in its typical course is not visible as it is occluded. Panel C, LAO 40%, caudal 30% (“spider view”): chronic occlusion of the mid LAD (triangle), significant stenosis of the first diagonal branch (triangle), two severe stenoses of the LCX (asterisks). Panel D, LAO 90%: the typical clinical course of the LAD is not visible (arrow), i.e. the vessel is occluded, severe LCX stenosis (asterisk).
Figure 4.
Angiogram before percutaneous coronary intervention. Panel A, left anterior oblique (LAO) 60°: acute occlusion of the mid-right coronary artery (RCA). Panel B, right anterior oblique (RAO) 30%, caudal 20%: left circumflex artery (LCX) with two significant stenoses (asterisks), first diagonal branch with significant lesions (triangle), the left anterior descending artery (LAD) in its typical course is not visible as it is occluded. Panel C, LAO 40%, caudal 30% (“spider view”): chronic occlusion of the mid LAD (triangle), significant stenosis of the first diagonal branch (triangle), two severe stenoses of the LCX (asterisks). Panel D, LAO 90%: the typical clinical course of the LAD is not visible (arrow), i.e. the vessel is occluded, severe LCX stenosis (asterisk).
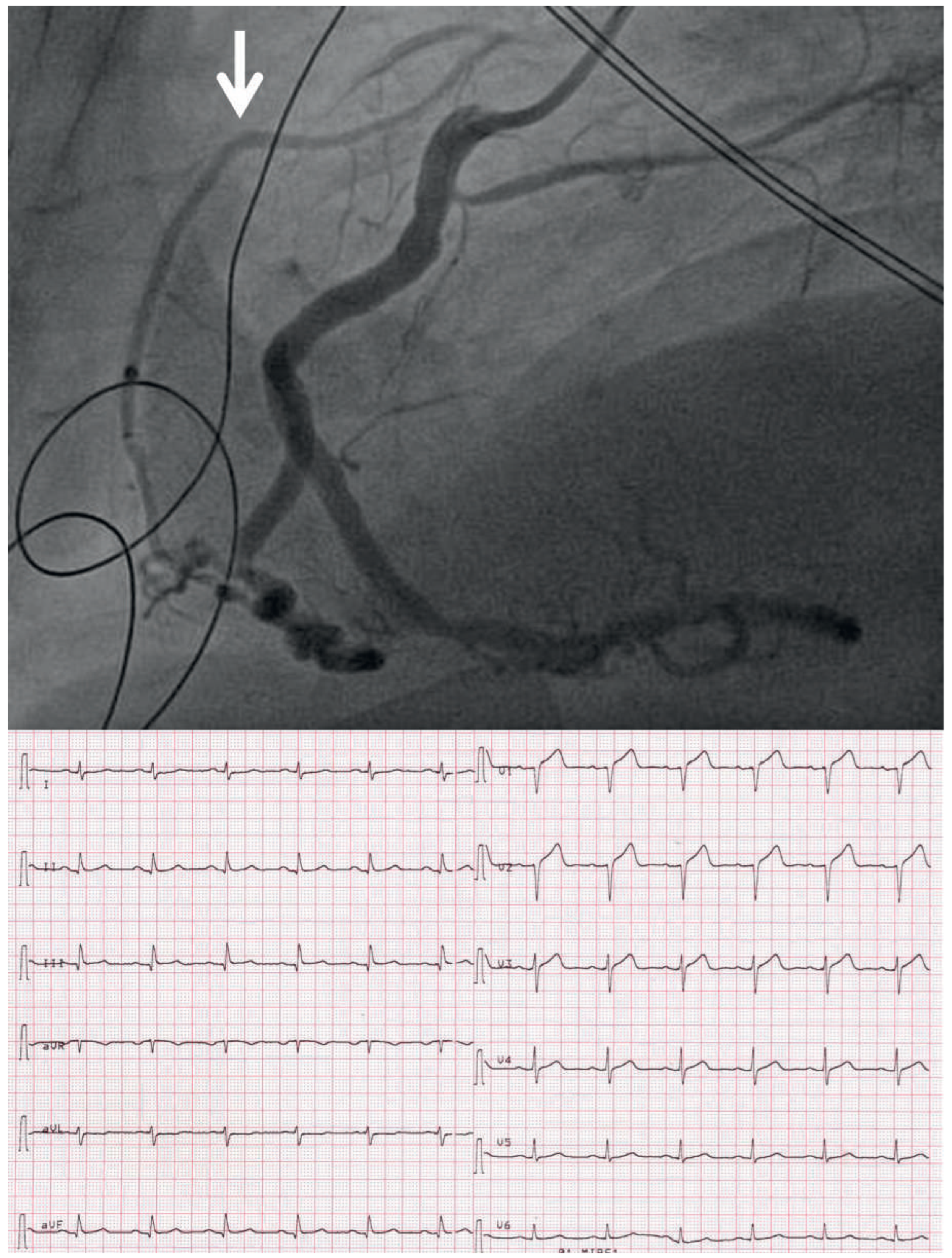
Figure 5.
Top: angiogram after percutaneous coronary intervention (PCI) of the right coronary artery (RCA), LAO 90% (same angiographic projection as
Figure 3, panel D). The RCA is open, and via the RCA and collaterals the LAD now becomes visible (arrow). Bottom: ECG after PCI.