Radiofrequency Ablation of Atrial Tachycardia from ''No-Man's Land"
Abstract
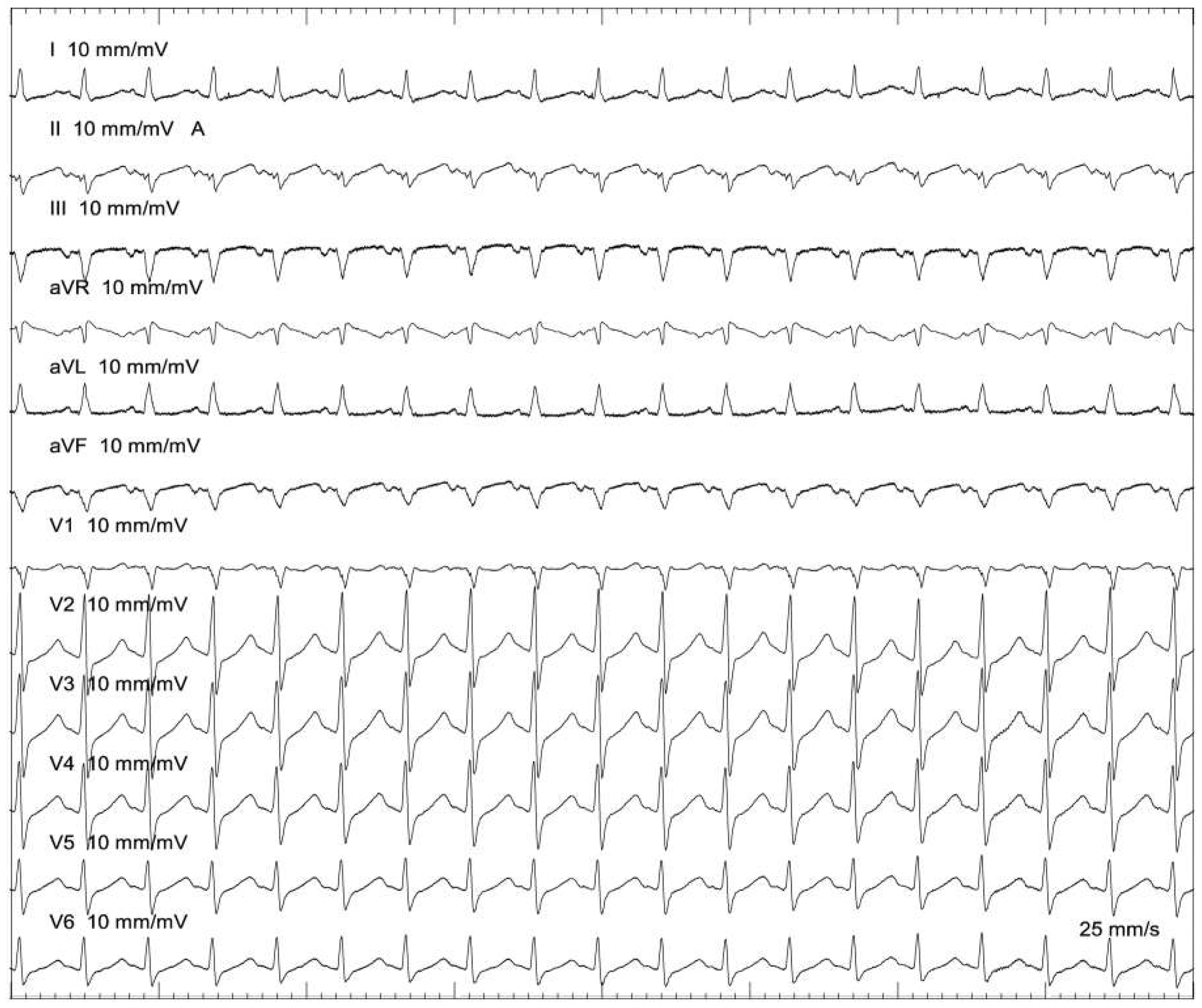
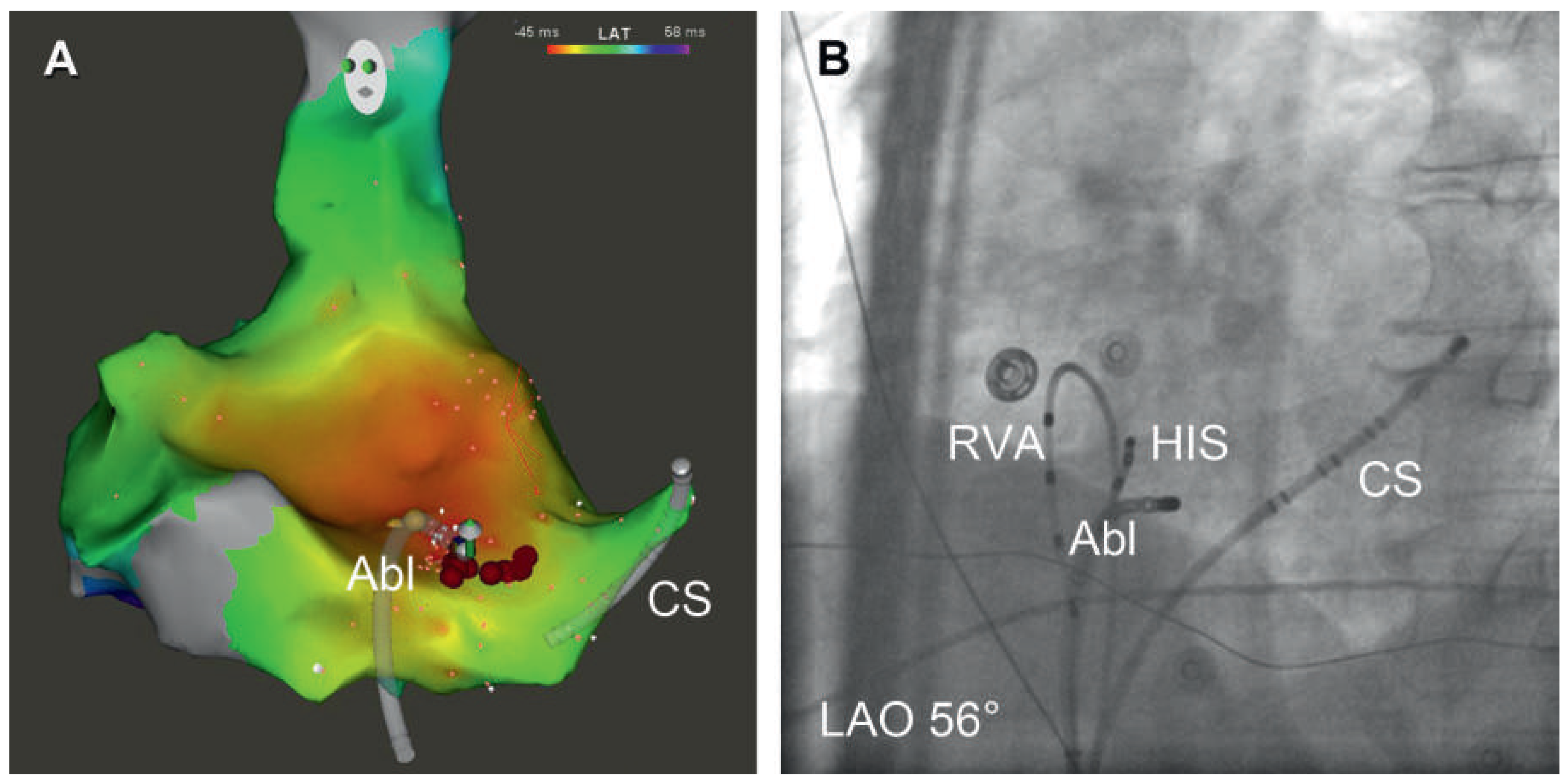
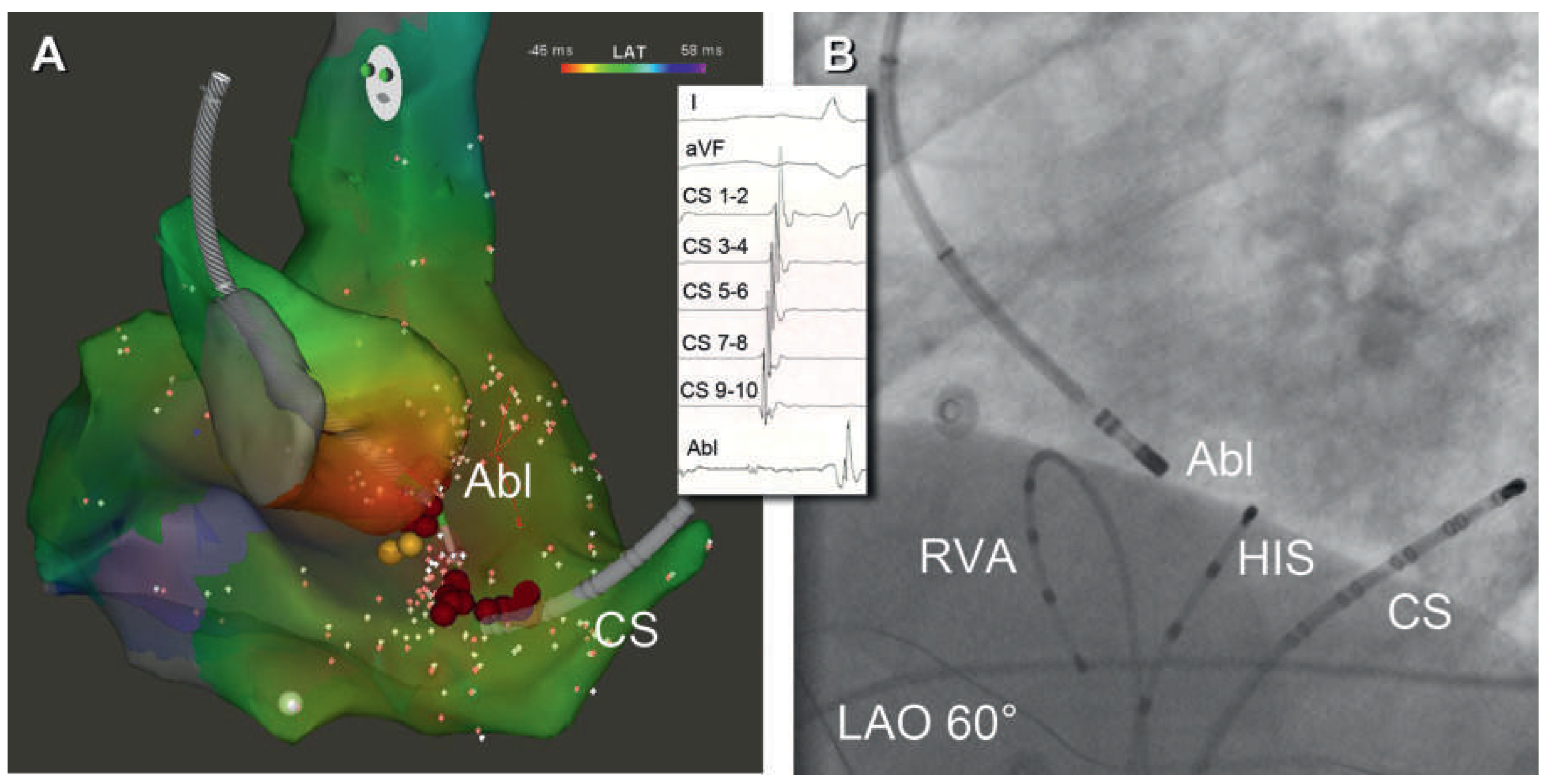
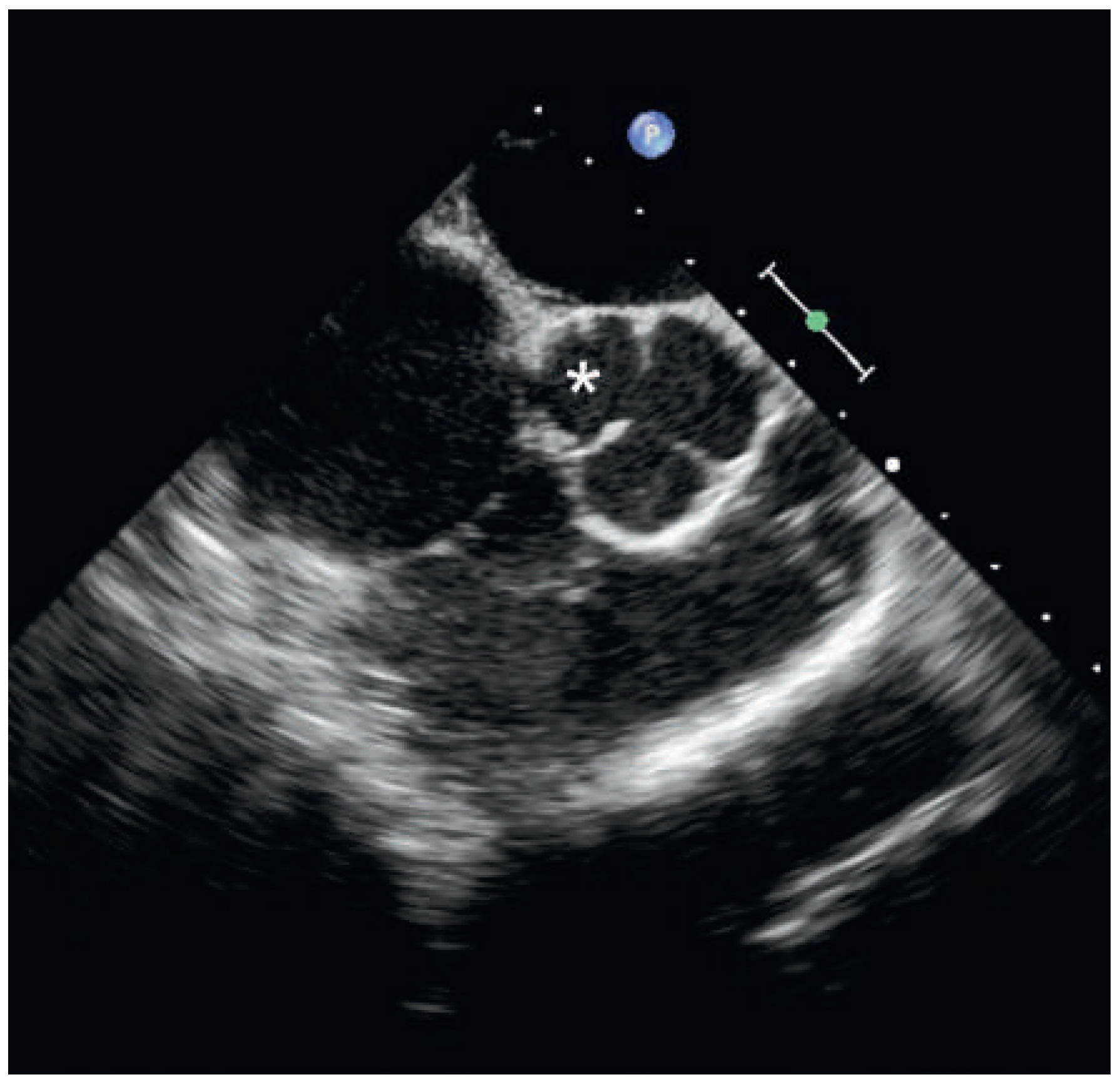
Case report
Discussion
Conclusion
Disclosures
References
© 2015 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Pavlović, N.; Knecht, S.; Mühl, A.; Reichlin, T.; Schaer, B.; Osswald, S.; Sticherling, C.; Kühne, M. Radiofrequency Ablation of Atrial Tachycardia from ''No-Man's Land". Cardiovasc. Med. 2015, 18, 103. https://doi.org/10.4414/cvm.2015.00322
Pavlović N, Knecht S, Mühl A, Reichlin T, Schaer B, Osswald S, Sticherling C, Kühne M. Radiofrequency Ablation of Atrial Tachycardia from ''No-Man's Land". Cardiovascular Medicine. 2015; 18(3):103. https://doi.org/10.4414/cvm.2015.00322
Chicago/Turabian StylePavlović, Nikola, Sven Knecht, Aline Mühl, Tobias Reichlin, Beat Schaer, Stefan Osswald, Christian Sticherling, and Michael Kühne. 2015. "Radiofrequency Ablation of Atrial Tachycardia from ''No-Man's Land"" Cardiovascular Medicine 18, no. 3: 103. https://doi.org/10.4414/cvm.2015.00322
APA StylePavlović, N., Knecht, S., Mühl, A., Reichlin, T., Schaer, B., Osswald, S., Sticherling, C., & Kühne, M. (2015). Radiofrequency Ablation of Atrial Tachycardia from ''No-Man's Land". Cardiovascular Medicine, 18(3), 103. https://doi.org/10.4414/cvm.2015.00322



