Abstract
A case is presented of prolonged complete atrioventricular block after elective balloon aortic valvuloplasty (BAV) of a congenital aortic stenosis in a 10-year-old patient. Implantation of a transient transvenous pacemaker for hemodynamic stabilization was required. Stable sinus rhythm reoccurred 72 hours after BAV
Introduction
Balloon aortic valvuloplasty (BAV) is the first-line treatment option in congenital valvular aortic stenosis in the absence of relevant valvular regurgitation. BAV is palliative in nature but can delay further intervention for several years. Especially in growing children this is a major advantage. It is a well established, and in general quite safe, method with few complications, especially in older children, with aortic regurgitation being the most frequent complication after BAV. There are only few reports of rhythm problems after such an intervention. We report a case of a prolonged and haemodynamically relevant complete atrioventricular (AV) block after standard BAV in a 1O-year-old boy.
Case report
A 10-year-old boy was followed up in our outpatient clinic for congenital valvular aortic stenosis. The stenosis was at the valvular level, with thickened, dysplastic leaflets in an anatomically tricuspid valve (Figure 1). After years of stable findings without symptoms, with moderate stenosis but no aortic regurgitation, he presented with increasing stenosis, with a peak gradient of 90 mm Hg (mean 53 mm Hg) and signs of left ventricular hypertrophy in transthoracic echocardiography. On the basis of these findings, the decision to perform a balloon valvuloplasty was made. The preinterventional electrocardiogram (ECG) did not show any conduction abnormality (sinus rhythm, heart rate 73 bpm, PQ 110 ms, QRS 80 ms, QT 370 ms, normal repolarisation).

Figure 1.
Transthoracic echocardiography; anatomically tricuspid valve with thickened dysplastic leaflets.
Catheterisation was performed under general anaesthesia. The stenotic aortic valve could easily be passed with a 5-French pigtail catheter. Invasive peak gradient was 46 mm Hg. The valve annulus was 16.7 mm (measured in an aortography-stillframe in systole between the valve hinge points). The stenosis was dilated using left ventricular rapid pacing (220 bpm) with a 16 mm Tyshak-balloon. During the first two dilatation attempts, the balloon slipped proximally, the third dilatation being successful (Figure 2), with rapid disappearance of the central waist. Peak gradient was reduced from 46 to 6 mm Hg. Better valve opening was noted but also moderate aortic regurgitation. After the successful dilatation, complete atrioventricular block with a wide QRS escape rhythm of 80 bpm was seen on ECG. Because of persistence of the complete heart block the patient was transferred to the intensive care unit for better surveillance. In the following hours he presented with desaturation, headache, abdominal pain, agitation and lactic acidosis. Therapy with isoprenaline did not improve symptoms. Finally he had to be supported with intravenous inotropes and diuretics because of clinical signs of low cardiac output with severe arterial hypotension and dyspnoea associated with bradycardia. Brain natriuretic peptide (BNP) rose to a maximum of 537 pg/ml at that time (normal value <100 pg/ml). In a transthoracic echocardiogram we could confirm moderate aortic regurgitation with good systolic function and a normal dimension of the left ventricle. Complete AV block persisted after 24 hours (Figure 3). Because of poor clinical tolerance of the new aortic regurgitation with persistent bradycardia (70–80 bpm) a transient intravenous (transjugular) Swan Ganz bipolar pacing catheter was placed 30 hours after BAV. The patient was paced at 100 bpm. Under this therapy the evolution was positive. The clinical symptoms of heart failure rapidly diminished. For afherload reduction therapy with a angiotensin converting-enzyme (ACE) inhibitor was started. Under constant pacing, the underlying rhythm was tested every 12 hours, but only at 72 hours after BAV a normofrequent sinus rhythm reappeared (Figure 4). After stabilisation and recompensation the pacing catheter could be removed 5 days after the intervention and the patient was transferred to the paediatric ward. He left hospital 7 days after BAV under diuretic and ACE inhibitor therapy. A Holter monitor confirmed a stable sinus rhythm at around 90 bpm at rest. Transthoracic echocardiography before discharge showed a mild residual aortic stenosis with residual peak gradient of 28 mm Hg (mean 11 mm Hg), and moderate aortic regurgitation with a calculated regurgitant fraction of 46%. BNP normalised to 44 pg/ml. Follow-up at 1 month showed stable sinus rhythm on Holter monitor and identical findings on echo with well tolerated moderate aortic regurgitation without left ventricular dilatation.
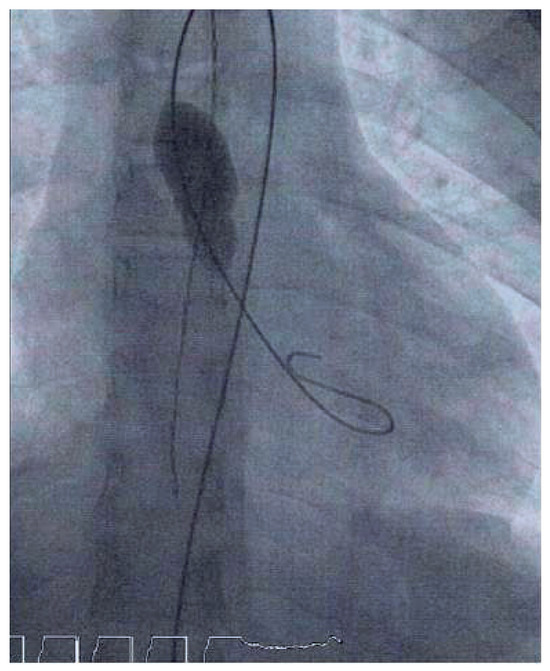
Figure 2.
Balloon position during dilatation.

Figure 3.
ECG at 48 hours after dilatation with complete AV dissociation; sinus rate of 108/min and narrow complex escape rhythm of 64/min.
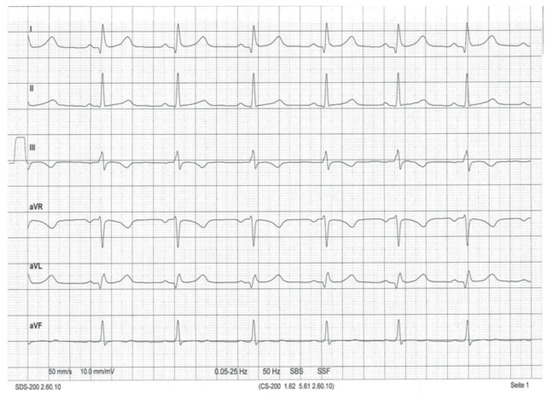
Figure 4.
ECG 72 hours after dilatation; normofrequent sinus rhythm, HR 84/min.
Discussion
Aortic regurgitation is the most common complication after balloon valvuloplasty. BAV is an established method, but especially in newborns the complication rate can be as high as 15% [1]. Short-term and transient arrhythmias are common in paediatric catheter interventions, but we were not able to find reports on longlasting arrhythmia after simple BAV in children. Such a prolonged occurrence of complete AV block was very surprising, and it was because we counted on the reappearance of sinus rhythm at any moment that implantation of a transvenous pacing catheter was deferred initially despite poor haemodynamics.
More data exist about important, persistent arrhythmia and need of permanent pacemaker (PPM) implantation after transcatheter aortic valve replacement (TAVR) in the elderly. A meta-analysis [2] showed male sex, baseline conduction disturbances, especially right bundle branch block, and intraprocedural AV block to be predictors of PPM implantation. One prospective study in adult patients undergoing balloon aortic valvuloplasty before TAVR analysed the frequency of cardiac conduction disturbances [3]. In this study 1.5% needed permanent pacemaker implantation. It was shown that the ratio of balloon size to left ventricular outflow obstruction (LVOT) diameter was an important factor, smaller LVOT being associated with more damage to the conduction system.
In our patient the reason for the prolonged complete AV block remains unclear. The preinterventional ECG did not show any conduction abnormality and the intervention itself was a standard procedure without major problems. It is known that trauma to the LVOT has the potential to damage the conduction system [4]. Balloon size was a proper choice for the diameter of the aortic annulus (16 mm balloon for an aortic annulus of 16.7 mm, ratio balloon/annulus = 0.96). Clinical observations support the concept of damage to the conduction system from mechanical manipulation in the area of the aortic valve. One might also speculate on an anatomic variant of the conduction system with a more subendocardial position on the left ventricular aspect. In conclusion, this case of prolonged complete AV block after BAV is a very unusual observation which does not allow for advice on what should be done differently in future cases.
Conflicts of Interest
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Ewert, P.; Bertram, H.; Breuer, J.; Dähnert, I.; Dittrich, S.; Eicken, A.; et al. Balloon valvuloplasty in the treatment of congenital aortic valve stenosis—A retrospective multicenter survey of more than 1000 patients. Int J Cardiol. 2011, 149, 182–185. [Google Scholar] [CrossRef] [PubMed]
- Siontis, G.C.; Jüni, P.; Pilgrim, T.; Stortecky, S.; Büllesfeld, L.; Meier, B.; et al. Predictors of permanent pacemaker implantation in patients with severe aortic stenosis undergoing TAVR: A meta-analysis. J Am Coll Cardiol. 2014, 15, 129–140. [Google Scholar] [CrossRef] [PubMed]
- Laynez, A.; Ben-Dor, I.; Hauville, C.; Xue, Z.; Satler, L.; Kent, K.; et al. Frequency of Cardiac Conduction Disturbances After Balloon Aortic Valvuloplasty. Am J Cardiol. 2011, 108, 1311–1315. [Google Scholar] [CrossRef] [PubMed]
- Erkapic, D.; De Rosa, S.; Kelava, A.; Lehmann, R.; Fichtlscherer, S.; Hohnloser, S. Risk for Permanent Pacemaker After Transcatheter Aortic Valve Implantation: A Comprehensive Analysis of the Literature. J Cardiovasc Electrophysiol. 2012, 23, 391–397. [Google Scholar] [CrossRef] [PubMed]
© 2015 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).