The Weak Heart: Perioperative Management
Abstract
Introduction
Epidemiology
Heart failure as a perioperative risk factor
Risk assessment
Definition and diagnosis of heart failure
Definition
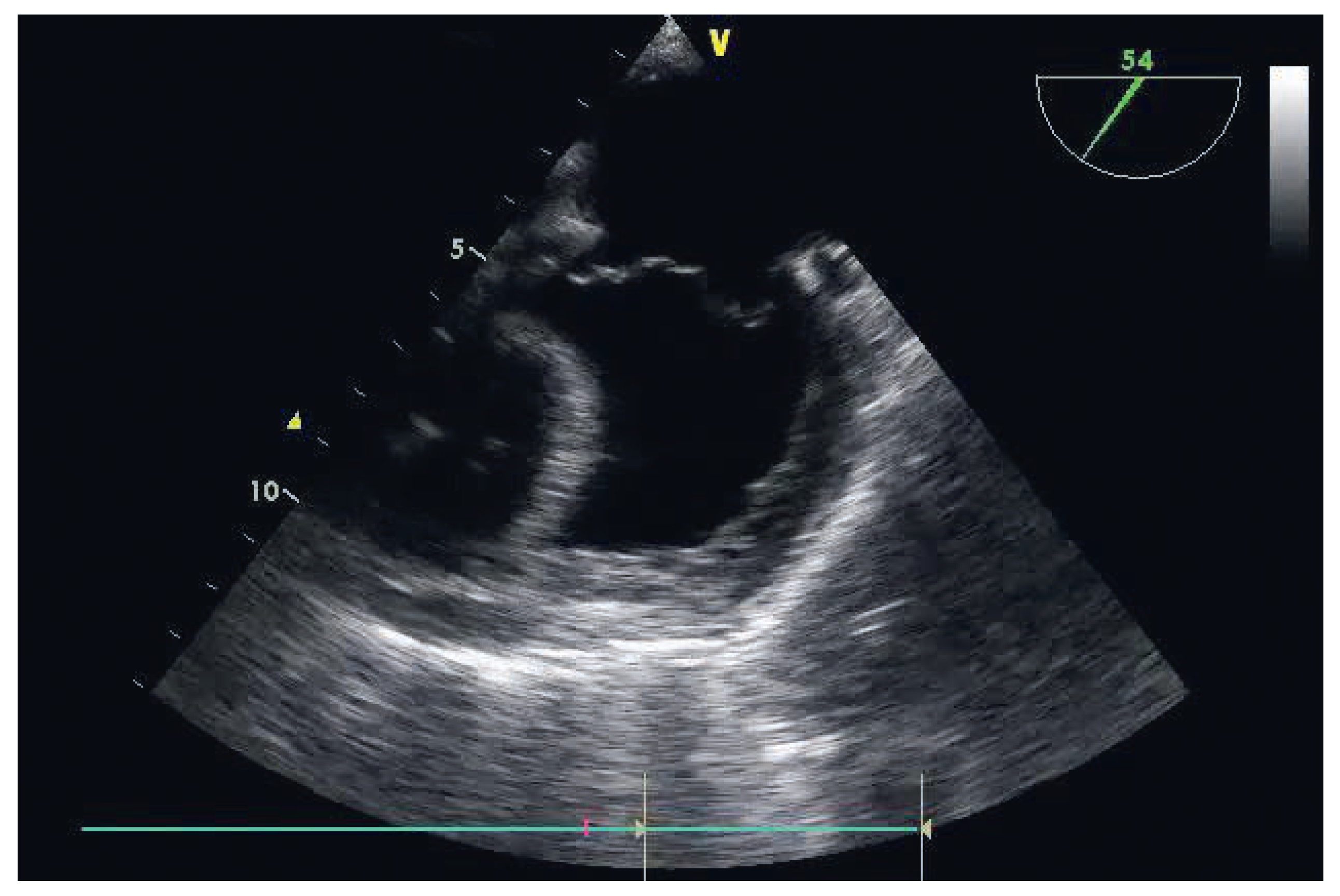
Diagnosis
Perioperative triggers of acute cardiac decompensation
Specific perioperative considerations of right ventricular failure
Premedication
Intraoperative prevention
Monitoring
Choice of anaesthesia
Perioperative LVF management
Specific perioperative considerations of right ventricular failure
- –
- In noncardiac surgery, perioperative right ventricular failure is most often, although not exclusively, secondary to acute PHT; a normal right ventricle can cope for only 1–2 hours with a mean positive airway pressure of ≤40 mm Hg [49].
- –
- In cardiac surgery, right ventricular failure may be secondary to acute PHT, but also frequently to volume overload, myocardial ischaemia, preexisting right ventricular dysfunction or arrhythmias. Among cardiac surgery patients, those undergoing cardiac transplantation or LVAD implantation are at higher risk.
- –
- Grown-up congenital heart disease (GUCH) patients, for cardiac or noncardiac surgery.
Premedication
Intraoperative prevention
Monitoring
Choice of anaesthesia
Perioperative RVF management
Conclusion
Conflicts of Interest

| ACCF/AHA stages of HF | NYHA functional classification | ||
|---|---|---|---|
| A | At high risk for HF but without structural heart disease or symptoms of HF | 0 | |
| B | Structural heart disease but without signs or symptoms of HF | I | No limitation of physical activity, ordinary physical activity does not cause symptoms of HF |
| C | Structural heart disease with prior or current symptoms of HF | I | No limitation of physical activity, ordinary physical activity does not cause symptoms of HF |
| II | Slight limitation of physical activity. Comfortable at rest, but ordinary physical activity results in symptoms of HF | ||
| III | Marked limitation of physical activity. Comfortable at rest, but less than ordinary physical activity causes symptoms of HF | ||
| IV | Unable to carry on any physical activity without symptoms of HF, or symptoms of HF at rest | ||
| D | Refractory HF requiring specialised interventions | IV | Unable to carry on any physical activity without symptoms of HF, or symptoms of HF at rest |
| Mechanism | Left ventricular failure | Right ventricular failure |
|---|---|---|
| Excessive pressure | Aortic stenosis | Primary or secondary pulmonary hypertension |
| load | Hypertrophic obstructive cardiomyopathy | HTPL/LTPL |
| Arterial hypertension | Pulmonary stenosis | |
| Some types of congenital heart disease | ||
| (i.e., Fallot) | ||
| Excessive volume | Aortic or mitral regurgitation | Pulmonary or tricuspid regurgitation |
| load | High-output states (thyrotoxicosis) | ASD |
| Some types of congenital heart disease (i.e., VSD) | Iatrogenic | |
| Iatrogenic | LVAD | |
| Primary myocardial | Ischaemic heart disease | Ischemic heart disease |
| disease | Hypertrophic nonobstructive cardiomyopathy | Hypertrophic obstructive cardiomyopathy |
| Hypertrophic obstructive cardiomyopathy | Dilated cardiomyopathy | |
| Dilated cardiomyopathy | Arrhythmogenic cardiomyopathy | |
| Cardiomyopathy of the elderly | Myocarditis | |
| Myocarditis | ||
| Metabolic heart disease | ||
| Endocrine heart disease | ||
| Impaired ventricular | Tight mitral stenosis | Tight tricuspid stenosis |
| filling | Constrictive pericarditis | Constrictive pericarditis |
| Restrictive cardiomyopathy | Restrictive cardiomyopathy | |
| Tamponade | ||
| Some types of congenital heart disease | ||
| (i.e., Ebstein anomaly) |
| Left ventricular failure | Right ventricular failure |
|---|---|
| Avoidance of drug-induced myocardial depression | Avoidance of drug-induced myocardial depression |
| Preservation of ventricular interaction | |
| Optimisation of preload | Optimisation of preload |
| Maintenance of SR and A–V synchrony Heart rate control | Maintenance of SR and A–V synchrony Heart rate control |
| Reduction of left ventricular afterload | Avoidance of PHT exacerbation: hypoxemia, hypercarbia, hypothermia, acidosis, stress and pain Optimization of ventilator settings |
| Maintenance of adequate systemic perfusion pressure for organ perfusion | Maintenance of systemic perfusion pressure while minimising right ventricular dilatation |
| Avoidance of nephrotoxic and hepatotoxic drugs | Avoidance of nephrotoxic and hepatotoxic drugs |
| Minimisation of blood transfusion, especially of old blood | |
| Tailoring of therapy to the specific aetiology of the LVF | Tailoring of therapy to the specific aetiology of the RVF |
| Reduction of right ventricular afterload, preferentially with inhalative therapy | |
| Inotropic support | Inotropic support |
| Mechanical assist devices | Mechanical assist devices |
| Dose mcg/kg | Dose mcg/kg/min | Effects | Adverse effects | ||||
|---|---|---|---|---|---|---|---|
| Inotropic agent | Bolus | Infusion | CO | HR | SVR | PVR | |
| Dobutamine | N/A | 2.5 to 5 5 to 20 | ↑ ↑ | ↑ ↑ | ↓ ↔ | ↔ ↔ | ↑/↓ BP, T, HA, N, F, hypersensitivity, O2myoc↑ |
| Adrenaline | N/A | to 0.05 | ↑ ↑ | ↑ | ↑ | ↑ | T, A, F, lactate↑ |
| 0.05 to 0.1 | ↑↔ | ↑ ↑ | ↑ ↑ | ↑ ↑ | Glyc↑, O2myoc↑↑ | ||
| >0.1 | ↑↔↓ | ↑ ↑ | ↑ ↑ ↑ | ↑ ↑ | |||
| Milrinone | N/R | 0.125 to 0.175 | ↑ ↑ | ↑ | ↓ | ↓ | A, T, ↓BP, O2myoc↑↔ |
| Levosimendan | N/R | 0.05 to 0.2 | ↑ ↑ | ↑↔ | ↓↓ | ↓ | T, A, HA, ↓BP, hypoK, O2myoc↔ |
| Noncardiac surgery |
|---|
| PHT: hypoxia, hypoventilation, atelectasis, high ventilation pressures, acute pulmonary embolism (orthopaedic surgery) |
| Myocardial ischaemia: coronary artery disease |
| Elevated LAP: mitral valve disease, systolic or diastolic LVF |
| LVAD |
| Lung transplantation |
| GUCH |
| Cardiac surgery |
| Myocardial ischaemia or infarction |
| Inadequate myocardial protection, intracoronary air embolism |
| RV diastolic dysfunction associated with abnormal interventricular septal motion |
| PHT: CPB, protamine reaction, acute on chronic PHT |
| LVAD |
| HTPL |
| GUCH |
© 2015 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bettex, D.A.; Chassot, P.-G.; Rudiger, A. The Weak Heart: Perioperative Management. Cardiovasc. Med. 2015, 18, 273. https://doi.org/10.4414/cvm.2015.00362
Bettex DA, Chassot P-G, Rudiger A. The Weak Heart: Perioperative Management. Cardiovascular Medicine. 2015; 18(10):273. https://doi.org/10.4414/cvm.2015.00362
Chicago/Turabian StyleBettex, Dominique Anne, Pierre-Guy Chassot, and Alain Rudiger. 2015. "The Weak Heart: Perioperative Management" Cardiovascular Medicine 18, no. 10: 273. https://doi.org/10.4414/cvm.2015.00362
APA StyleBettex, D. A., Chassot, P.-G., & Rudiger, A. (2015). The Weak Heart: Perioperative Management. Cardiovascular Medicine, 18(10), 273. https://doi.org/10.4414/cvm.2015.00362




