ARVD with Recurrent Ventricular Tachycardia Episodes
Case presentation
Question
Discussion
- -
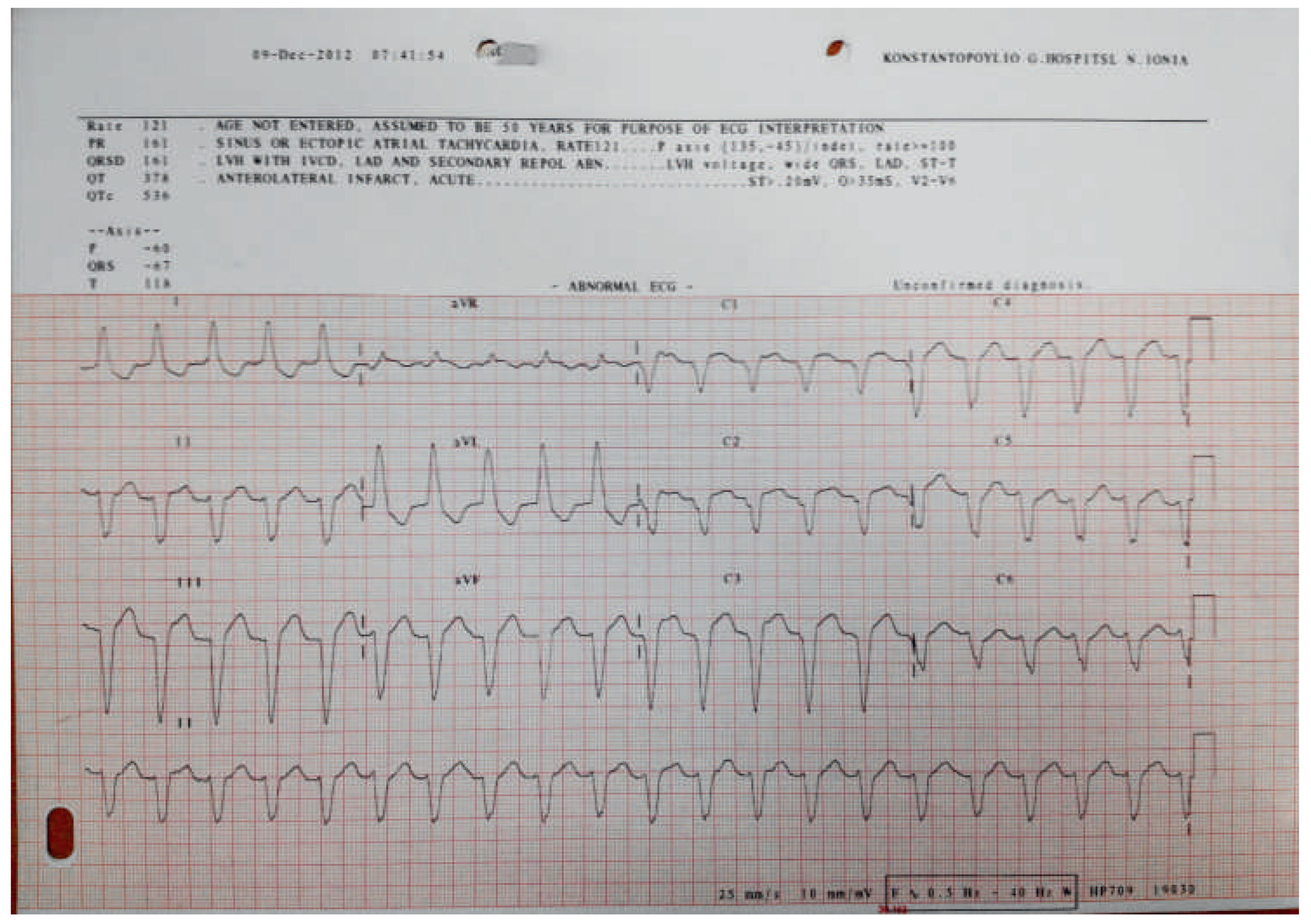
- A terminal activation of duration ≥55 ms in V1–V3 as shown in Figure 2 (measured from the nadir of the S wave to the end of the QRS complex, including R’, in V1, V2 or V3 in the absence of complete right bundle block; minor diagnostic criterion according to TFC).
- -
- Epsilon waves as shown in Figure 2 (arrow; reproducible low-amplitude signal between the end of the QRS complex to the onset of the T wave in V1–V3; major diagnostic criterion according to TFC).
- -
- T wave inversions in V1, V2 and V3 or beyond in individuals older than 14 years of age as shown in Figure 2.
Funding/potential competing interests
© 2014 by the author. Attribution-Non-Commercial-NoDerivatives 4.0.
Share and Cite
Margariti, C.; Vlagouli, V. ARVD with Recurrent Ventricular Tachycardia Episodes. Cardiovasc. Med. 2014, 17, 189. https://doi.org/10.4414/cvm.2014.00245
Margariti C, Vlagouli V. ARVD with Recurrent Ventricular Tachycardia Episodes. Cardiovascular Medicine. 2014; 17(6):189. https://doi.org/10.4414/cvm.2014.00245
Chicago/Turabian StyleMargariti, Chrysanthi, and Vassiliki Vlagouli. 2014. "ARVD with Recurrent Ventricular Tachycardia Episodes" Cardiovascular Medicine 17, no. 6: 189. https://doi.org/10.4414/cvm.2014.00245
APA StyleMargariti, C., & Vlagouli, V. (2014). ARVD with Recurrent Ventricular Tachycardia Episodes. Cardiovascular Medicine, 17(6), 189. https://doi.org/10.4414/cvm.2014.00245



