Which Arrhythmia Would You Prefer?
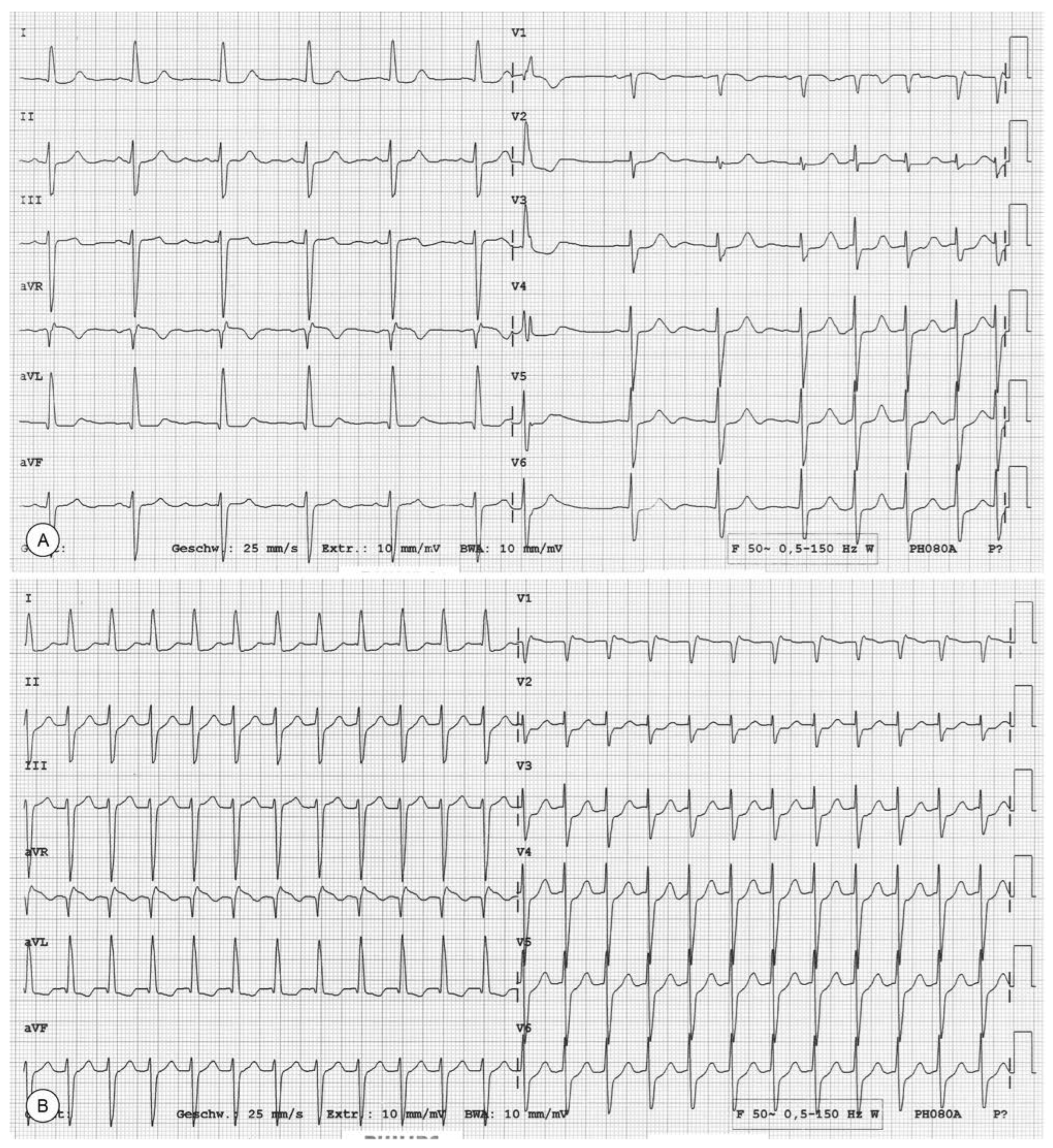
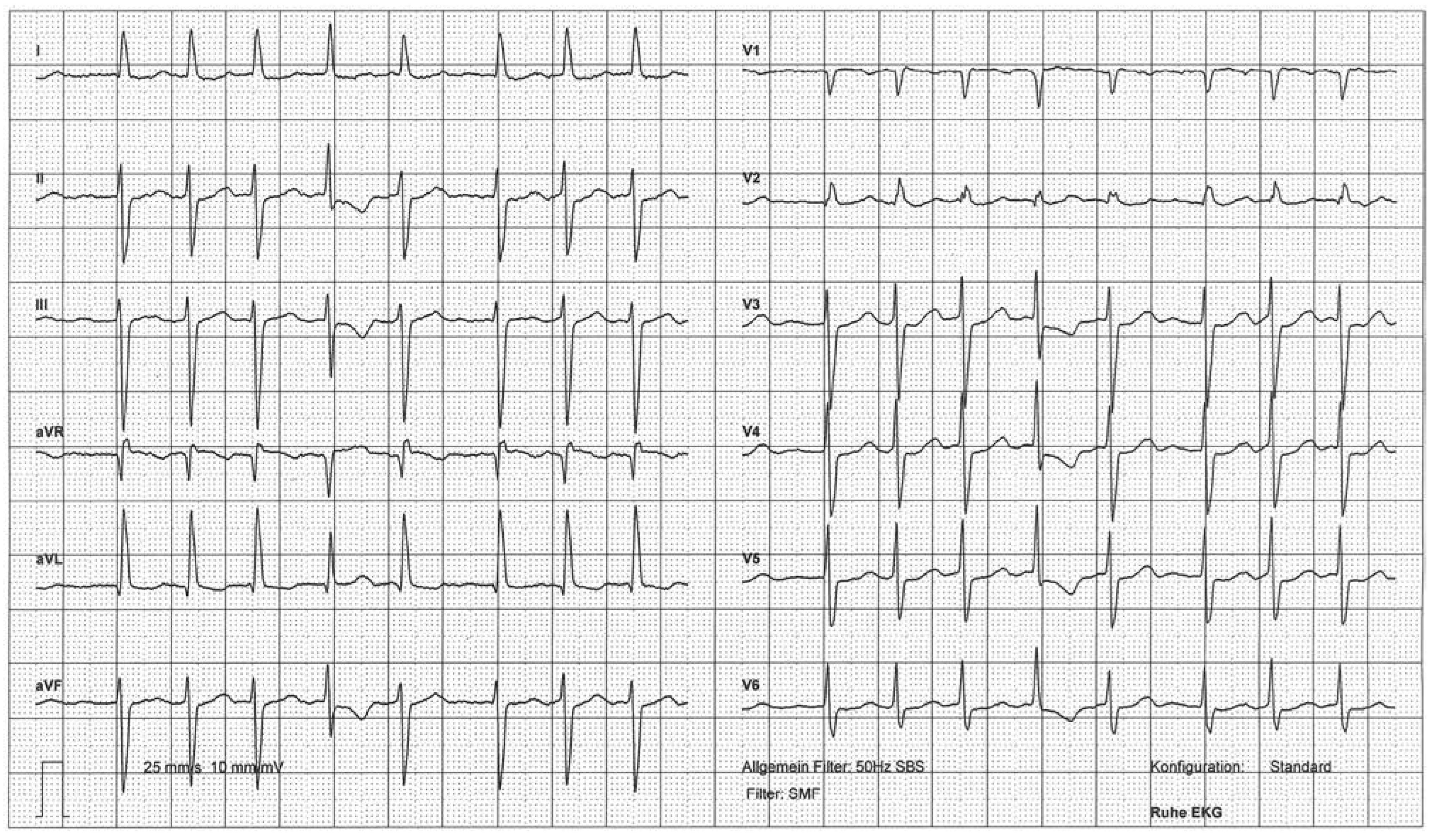
Case report
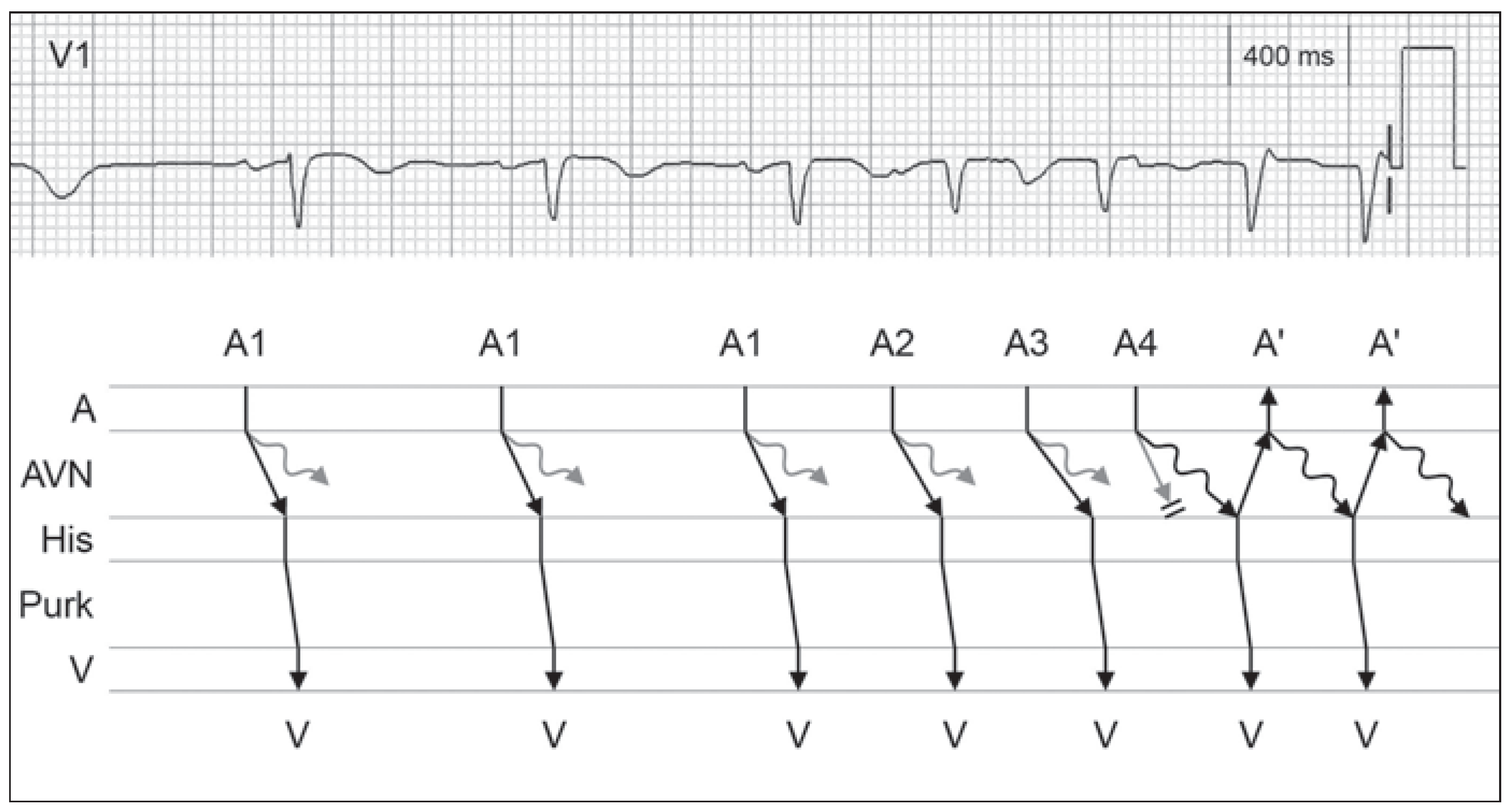
Discussion
Funding/potential competing interests
References
- Centurión, O.A.; Shimizu, A.; Isomoto, S.; Konoe, A. Mechanisms for the genesis of paroxysmal atrial fibrillation in the Wolff Parkinson White syndrome: intrinsic atrial muscle vulnerability vs. electrophysiological properties of the accessory pathway. Europace 2008, 10, 294–302. [Google Scholar] [CrossRef] [PubMed]
- Lip, G.Y.; Tse, H.F.; Lane, D.A. Atrial fibrillation. Lancet 2012, 379, 648–661. [Google Scholar] [CrossRef] [PubMed]
- Camm, A.J.; Lip, G.Y.; De Caterina, R.; Savelieva, I.; Atar, D.; Hohnloser, S.H.; et al. 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur. Heart J. 2012, 33, 2719–2747. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Jäggi, P.; Müller-Burri, S.A. Which Arrhythmia Would You Prefer? Cardiovasc. Med. 2014, 17, 156. https://doi.org/10.4414/cvm.2014.00243
Jäggi P, Müller-Burri SA. Which Arrhythmia Would You Prefer? Cardiovascular Medicine. 2014; 17(5):156. https://doi.org/10.4414/cvm.2014.00243
Chicago/Turabian StyleJäggi, Peter, and Stephan Andreas Müller-Burri. 2014. "Which Arrhythmia Would You Prefer?" Cardiovascular Medicine 17, no. 5: 156. https://doi.org/10.4414/cvm.2014.00243
APA StyleJäggi, P., & Müller-Burri, S. A. (2014). Which Arrhythmia Would You Prefer? Cardiovascular Medicine, 17(5), 156. https://doi.org/10.4414/cvm.2014.00243



