Summary
Distinction between ventricular tachycardia (VT) and supraventricular tachycardia (SVT) with aberrant conduction has major therapeutic and prognostic implications. Exclusive assessment of lead aVR, using a four-step algorithm can rapidly make such distinction with a high degree of diagnostic accuracy. To illustrate the concept, we present the case of a 70-year-old female with a prior history of supraventricular dysrrhythmias, who presented with a wide-complex tachycardia.
Presentation
Distinction between ventricular tachycardia (VT) and supraventricular tachycardia (SVT) with aberrant conduction has major therapeutic and prognostic implications. Rapid assessment of lead aVR, frequently referred to as the “forgotten lead”, can be lifesaving. A 70-year-old woman presented to the Emergency Department with 8 hours of persistent dizziness and palpitations. Her past medical history was significant for compensated ischaemic cardiomyopathy with placement of a cardiac resynchronisation therapy–implantable cardioverter-defibrillator (CRT-ICD) several years ago; her defibrillator component had been deactivated 12 months previously because of multiple inappropriate shocks for supraventricular dysrhythmias, leading to posttraumatic stress disorder. On initial assessment, the patient was conversant and pleasant, in no acute distress, but was noted to be tachycardic, with a systolic blood pressure of 110 mm Hg. Her physical examination was unrevealing. Chest X-ray did not show any acute cardiopulmonary abnormality. Laboratory values included a normal complete blood count, thyroid stimulating hormone and serum electrolytes. Troponin I was negative.
Assessment
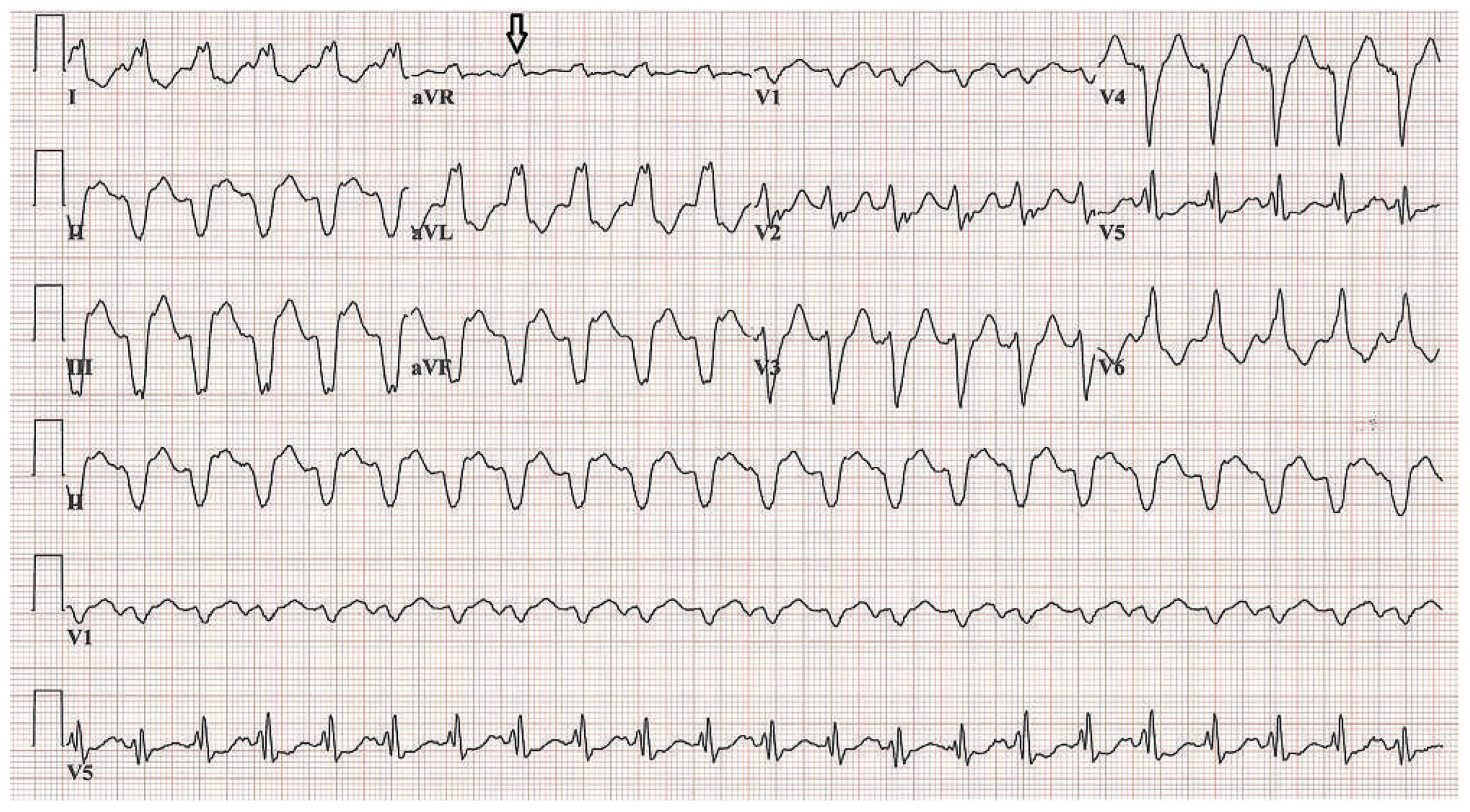
A 12-lead electrocardiogram (ECG) confirmed the presence of tachycardia at rate of 131 beats per minute (Figure 1), with a regular pattern, left axis deviation and a wide QRS complex of 184 ms duration. Precordial ventricular concordance was absent, no fusion or capture complexes could be clearly identified. Given her haemodynamic stability, emergent electrical cardioversion was deferred and the Cardiology Department was consulted to help guide initial pharmacological management.
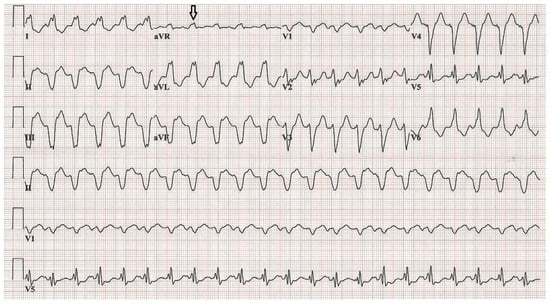
Figure 1.
Electrocardiogram on presentation demonstrated a regular, wide-complex tachycardia at a rate of 131 beats per minute. Notice the presence of an initial R wave in lead aVR.
Diagnosis
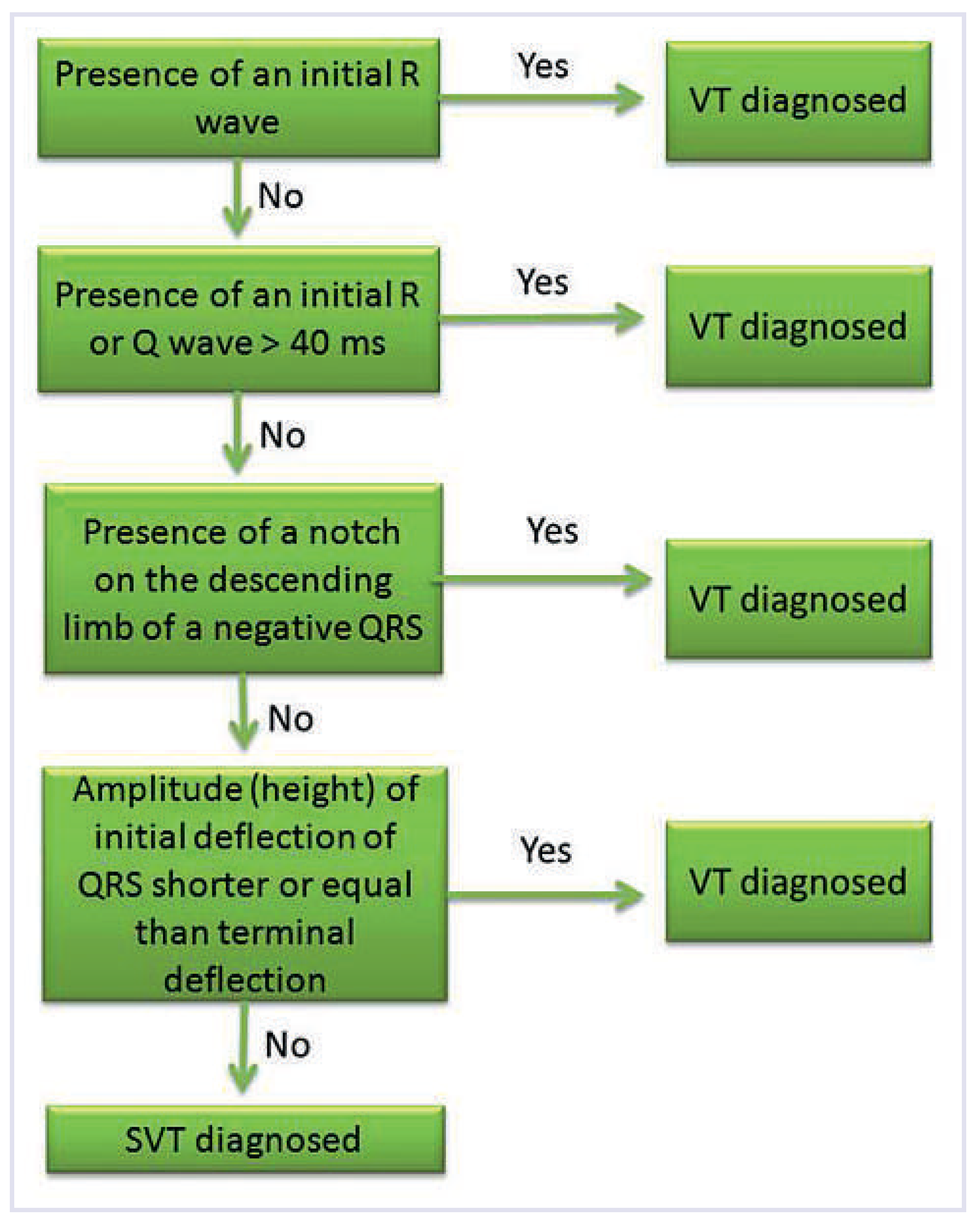
Multiple algorithms and electrocardographical criteria have been proposed to aid in the differential diagnosis of wide complex tachycardias. Brugada et al. [1] suggested a set of sequential criteria to discriminate between VT and SVT with aberrancy, but in real practice physicians often disagree in their diagnosis using such tools [2]. Many of the previously published morphological criteria to help distinguish VT from SVT with aberrancy are rather complex, particularly for the non-specialist, inconsistent and less useful in an acute setting. In an effort to simplify and expedite diagnosis, Vereckei et al. [3] have suggested an alternative algorithm (Figure 2) that requires a stepwise analysis of lead aVR only, with a reported overall test accuracy of 91.5%. A head-tohead comparison against the Brugada algorithm has shown better performance for the aVR algorithm, possibly with the added value of achieving a diagnosis more rapidly. As indicated by the first step of the aVR algorithm, a diagnosis of VT was readily made in this patient, given the presence of an initial dominant R wave in aVR. Other conditions that can give rise to a dominant R wave in aVR include dextrocardia, incorrect lead placement (left and right arm lead reversal) and intoxication with sodium-channel blockers, including tricyclic antidepressants [4].
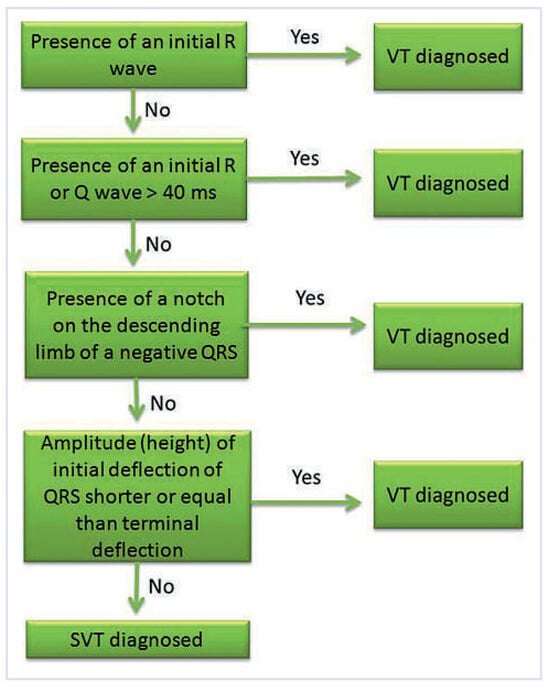
Figure 2.
Four-step algorithm using only lead aVR to discriminate between ventricular tachycardia (VT) or supraventricular tachycardia (SVT) with aberrancy. Adapted from Vereckei et al. [3].
Application of the Brugada criteria in this case would have achieved a diagnosis of VT until the third step, given the presence of atrioventricular (AV) dissociation [1], a very specific finding for VT but only present in 50% of such tracings [3]. A five-step aVR algorithm by Vereckei et al. has been tested, which includes the presence of AV dissociation as the first step, without any increase in diagnostic accuracy as compared with the four-step process.
Management
Medical treatment differs significantly in haemodynamically stable patients with VT when compared with SVT with aberrancy; AV nodal blocking agents, such as beta blockers, calcium-channel blockers and adenosine are often the preferred drugs for SVT with aberrancy; however their misuse in VT can have disastrous consequences [5]. Vaughan-Williams Class 1 or 3 antiarrhythmics are preferred for medical management of VT [6]. Our patient received a bolus of 150 mg lidocaine IV, with plans to perform a synchronised cardioversion under sedation; fortunately, she experienced chemical cardioversion within 5 minutes (Figure 3). Her CRT device was interrogated, and confirmed the presence of ventricular tachycardia. She was transitioned to combination therapy with oral amiodarone and mexiletine with no recurrences at 6 weeks follow up. Reactivation of ICD therapies was offered but the patient declined.
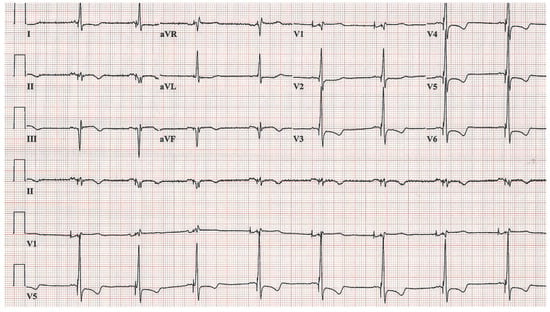
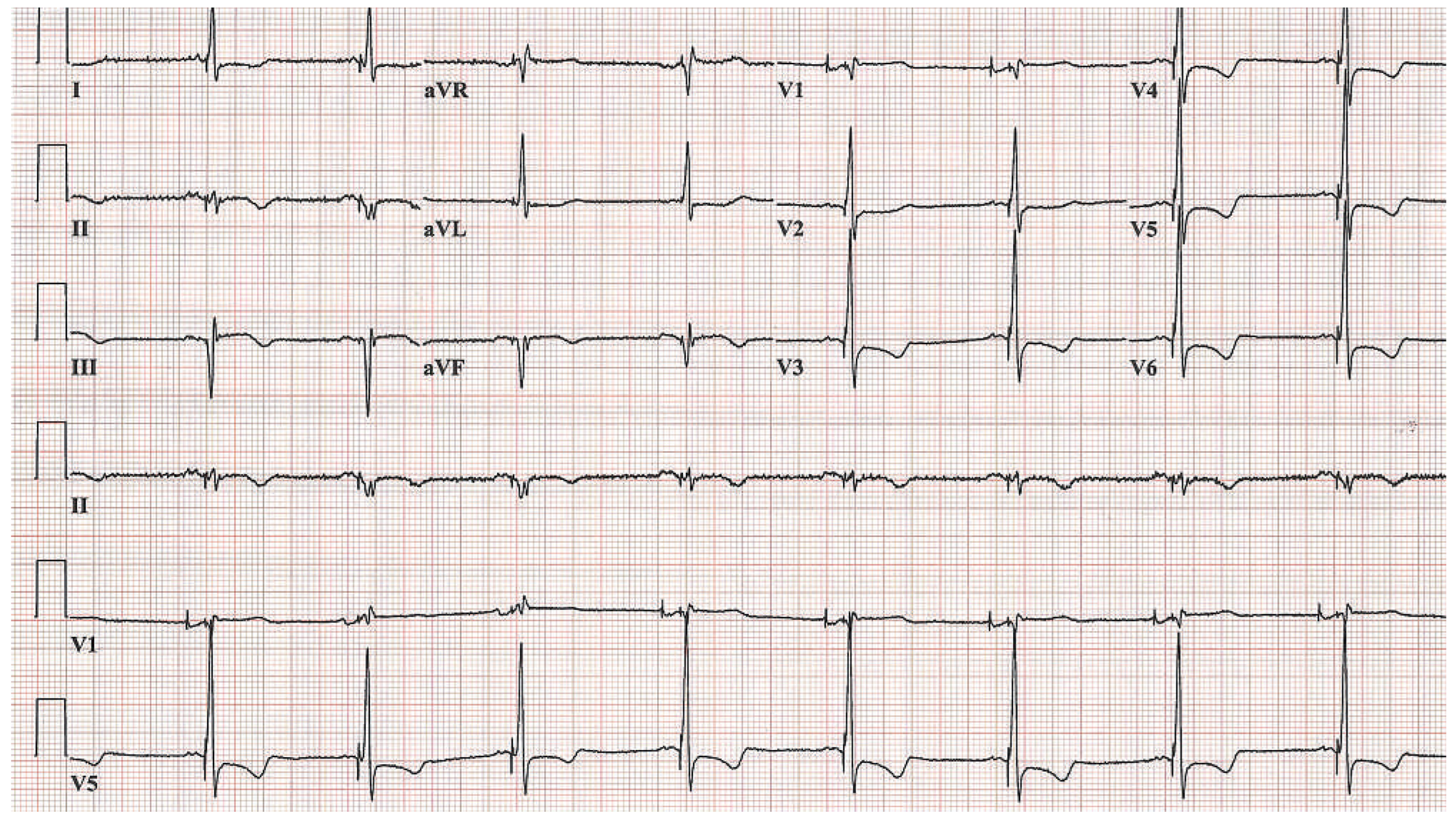
Figure 3.
Repeat electrocardiogram after chemical cardioversion with intravenous lidocaine bolus, which displays underlying normal sinus rhythm and sequential atrioventricular pacing.
Conclusions
Distinction between ventricular tachycardia (VT) and supraventricular tachycardia (SVT) with aberrant conduction has major therapeutic and prognostic implications, and appropriate assessment of patient’s history and ECG are essential. Not all patients presenting with VT exhibit haemodynamic instability, and it may be well tolerated in patients with no significant structural heart disease or those already on antiarrhythmic drugs. Exclusive assessment of lead aVR with a simple four-step algorithm can allow rapid discrimination between VT and SVT with aberrancy, with a high degree of diagnostic accuracy.
Funding / potential competing interests
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Brugada, P.; Brugada, J.; Mont, L.; Smeets, J.; Andries, E.W. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991, 83, 1649–1659. [Google Scholar] [CrossRef] [PubMed]
- Herbert, M.E.; Votey, S.R.; Morgan, M.T.; Cameron, P.; Dziukas, L. Failure to agree on the electrocardiographic diagnosis of ventricular tachycardia. Ann Emerg Med. 1996, 27, 35–38. [Google Scholar] [CrossRef] [PubMed]
- Vereckei, A.; Duray, G.; Szenasi, G.; Altemose, G.T.; Miller, J.M. New algorithm using only lead aVR for differential diagnosis of wide QRS complex tachycardia. Heart Rhythm. 2008, 5, 89–98. [Google Scholar] [CrossRef] [PubMed]
- George, A.; Arumugham, P.S.; Figueredo, V.M. aVR-the forgotten lead. Exp Clin Cardiol. 2010, 15, e36–e44. [Google Scholar] [PubMed]
- Stewart, R.B.; Barddy, G.H.; Greene, H.L. Wide complex tachycardia: Misdiagnosis and outcome after emergent therapy. Ann Intern Med. 1986, 104, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Zipes, D.P.; Camm, A.J.; Borggrefe, M.; Buxton, A.E.; Chaitman, B.; Fromer, M.; et al. ACC/AHA/ESC guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. J Am Coll Cardiol. 2006, 48, e247–e346. [Google Scholar] [CrossRef] [PubMed]
© 2014 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.