1. Case Presentation
A 27-year-old male with no previous medical history presented with dyspnoea during exercise and intermittent irregular heartbeats. The patient had never experienced paroxysmal tachycardia, dizziness or syncope. The physical examination was unremarkable except for an irregular pulse with an abrupt intermittent drop in rate from 100 to 60 bpm.
The patient’s ECG is shown in Figure 1.

Figure 1.
The presenting ECG. P-waves are highlighted by arrowheads.
2. Questions
- What is your diagnosis?
- What treatment should be proposed?
3. Commentary
The tracing shows sinus rhythm at 100 bpm with atrioventricular (AV) conduction over an accessory pathway alternating with complete AV block and junctional escape rhythm. Slowing of the sinus rate favoured conduction over the accessory pathway (Figure 2) whereas acceleration of the sinus rate induced complete block over the accessory pathway (Figure 3). A DDD pacemaker was implanted and the subsequent clinical course was uneventful. No attempt was made to ablate the accessory pathway, as anterograde conduction was intermittent and the patient had never complained of tachycardia.
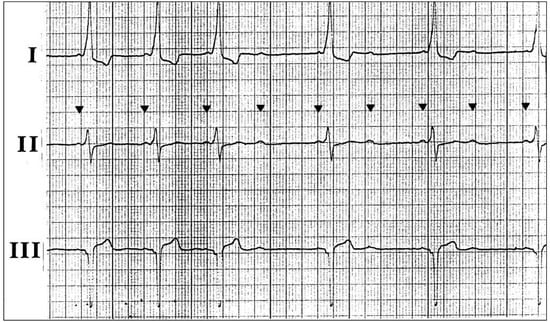
Figure 2.
Sinus rhythm at 75 bpm with 1:1 AV conduction via the accessory pathway followed by acceleration of the sinus rate with 2:1 AV conduction over the accessory pathway.

Figure 3.
Sinus rate of 105 bpm with complete AV block and a junctional escape rhythm at 50 bpm.
The association between congenital complete AV block and ventricular pre-excitation is rare [1,2,3,4]. Preexcitation is in fact beneficial when complete congenital AV block is present because it allows 1:1 AV conduction at rest and during exercise as long as anterograde conduction is preserved over the accessory pathway. No orthodromic atrioventricular reentrant tachycardia (AVRT) can occur because AV conduction is permanently blocked, but pre-excited tachycardias (atrial tachycardia, atrial flutter or atrial fibrillation) may be observed. Theoretically, antidromic AVRT can also occur if retrograde AV conduction is preserved, or if a second accessory pathway is present. Malaise, a sudden drop in heart rate or even syncope may occur when accessory pathway conduction becomes intermittent or disappears. Hence syncope in a patient with ventricular pre-excitation is not necessarily related to rapid conduction over the accessory pathway. Careful evaluation of AV node conduction is mandatory (e.g by demonstrating varying degrees of ventricular pre-excitation with incremental atrial pacing) when ablation of the accessory pathway is considered.
Funding
Dr. Burri was supported by a grant from the “Fondation de La Tour pour la Recherche Cardiovasculaire”.
References
- Erickson, C.C.; Yetman, A.T.; Jones, C.S.; Dungan, W.T. Late Onset of Accessory Pathway Conduction in a Patient with Complete AV Block. Pacing Clin. Electrophysiol. 2000, 23, 280–282. [Google Scholar] [CrossRef] [PubMed]
- A McLeod, K.; Rankin, A.C.; Houston, A.B. 1:1 atrioventricular conduction in congenital complete heart block. Heart 1998, 80, 525–526. [Google Scholar] [CrossRef] [PubMed]
- Rubio, J.A.; Saez, P.; Jimenez, J.J.; Robles, P. Congenital Complete Atrioventricular Block and Preexcitation Syndrome: A Well-Matched Partner. J. Interv. Card. Electrophysiol. 2005, 13, 159–161. [Google Scholar] [CrossRef] [PubMed]
- Sacher, F.; Douard, H.; Wright, M.; Vircoulon, B.; Broustet, J. Compensatory Accessory Pathway for Complete Atrioventricular Block: 28-Year Follow-Up. Pacing Clin. Electrophysiol. 2009, 32, 952–956. [Google Scholar] [CrossRef] [PubMed]
© 2013 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.