Rehabilitation Enrollment After Cardiac Procedures
Abstract
Introduction
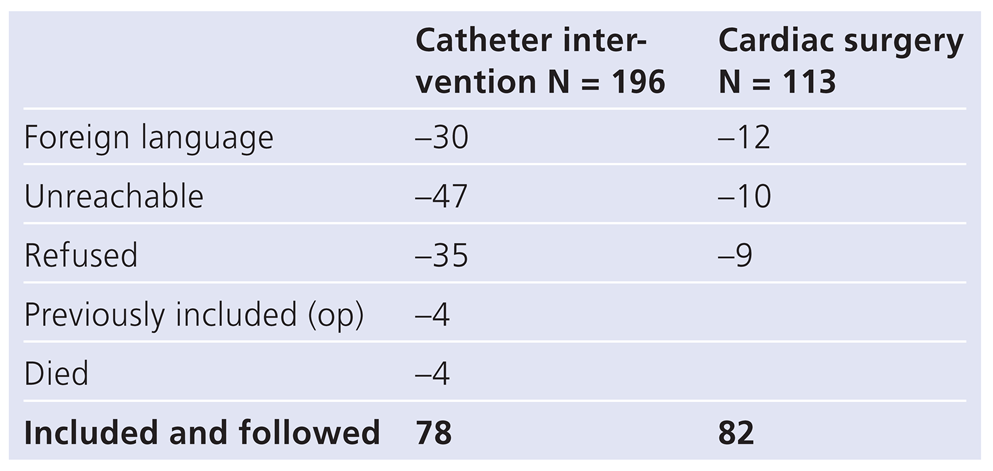
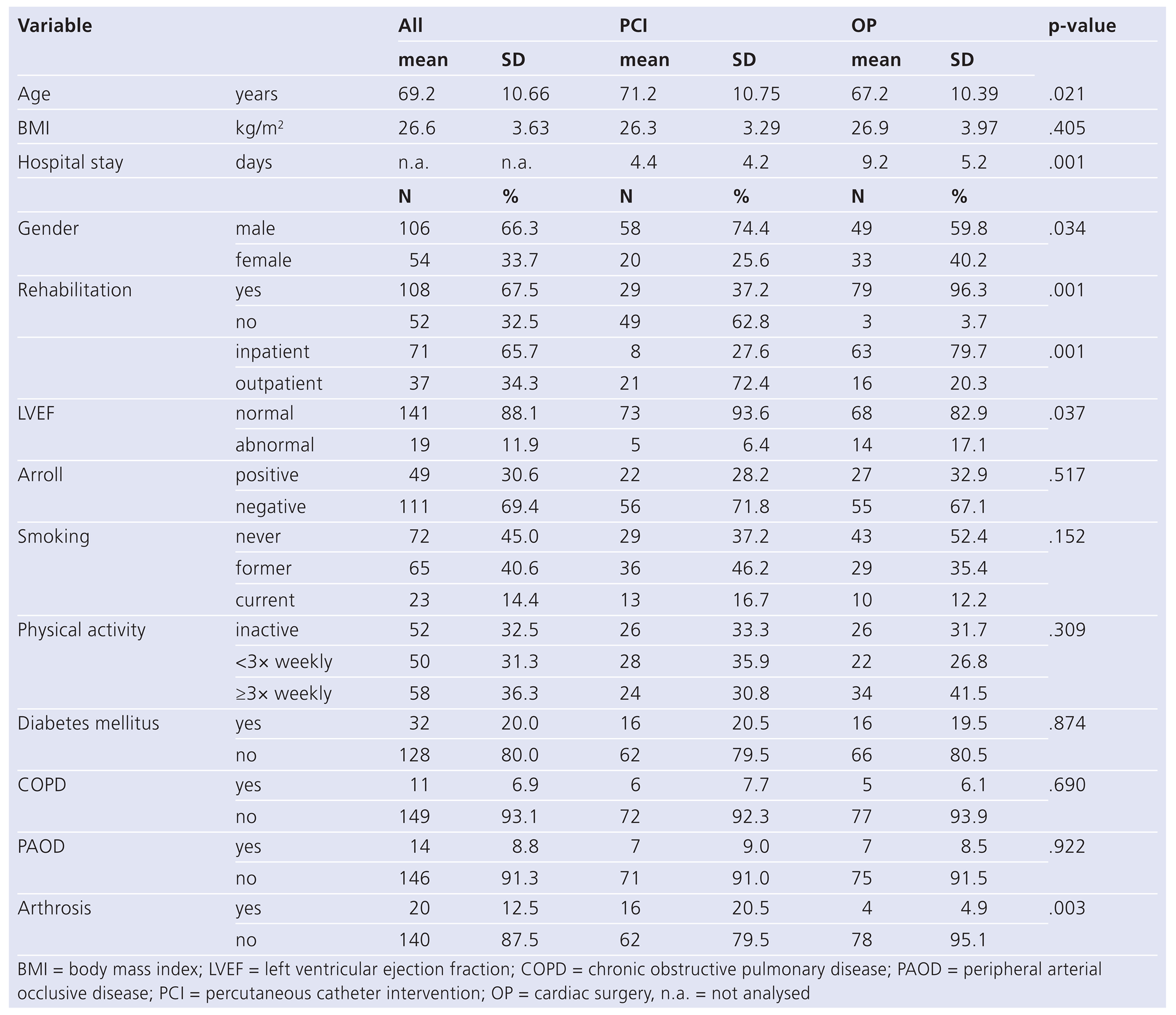
Methods
- –
- questions as to sociodemografic and vocational status;
- –
- questions concerning health status, including cardiovascular risk factors and comorbid state and assessment of depressivity by two screening questions of Arroll [12];
- –
- questions concerning rehabilitation enrollment, type of programme, reasons for participation or nonparticipation. Nonparticipants were at that time offered free individual counseling on physical activity for three months;
- –
- information on the type of intervention, LV function, complications and other medical variables were taken from the hospital records.
Statistics
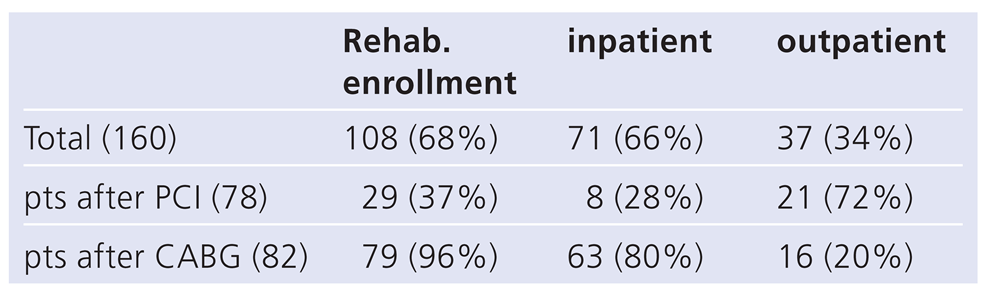
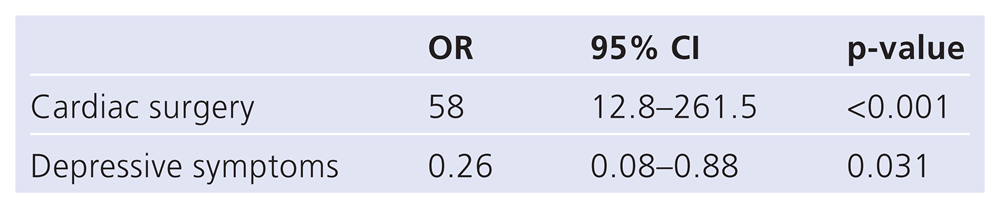
Results
Discussion
Participation rate
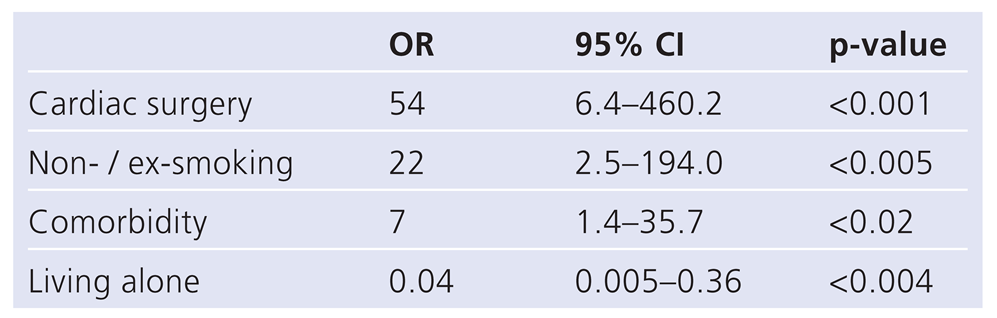
Predictors of rehabilitation enrollment
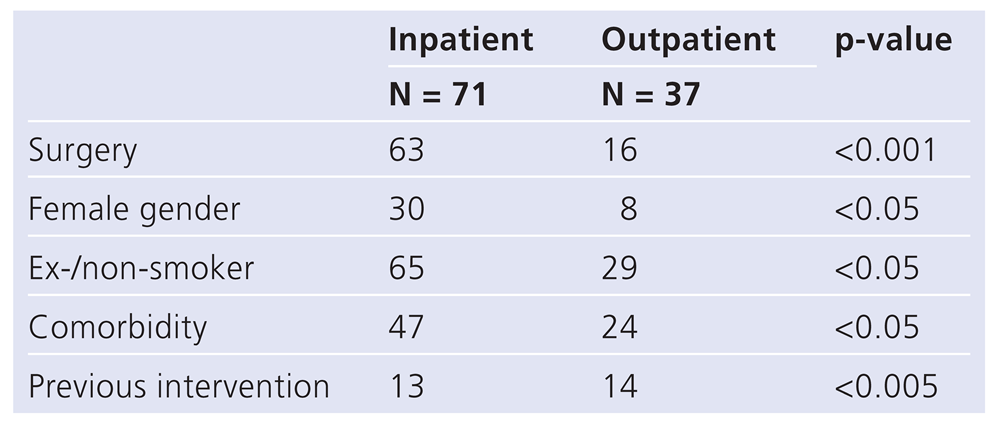
Inpatient vs outpatient programmes
Limitations
Funding/potential competing interests
References
- Joliffe, J.A.; Rees, K.; Taylor, R.S.; Thompson, D.; Oldridge, N.; Ebrahim, S. Exercise based rehabilitation for coronary heart disease. Cochrane Database Syst Rev 2001, 1, CD0011800. [Google Scholar] [CrossRef]
- Oldridge, N.B.; Guyatt, G.H.; Fischer, M.E.; Rimm, A.A. Cardiac rehabilitation after myocardial infarction combined experience of randomized clinical trials. JAMA. 1988, 260, 945–950. [Google Scholar] [CrossRef]
- Bjarnason Wehrens, B.; Schulz, O.; Gielen, S.; Halle, M.; Dürsch, M.; et al. Leitlinie körperliche Aktivität zur Sekundärprävention und Therapie kardiovaskulärer Erkrankungen. Clin Res Cardiol. 2009;Supplements 2009, 4, 1–44. [Google Scholar] [CrossRef]
- Heran, B.S.; Chen, J.M.; Ebrahim, S.; Moxham, T.; Oldridge, N.; Rees, K.; et al. Exercise based cardiac rehabilitation for coronary heart disease. Cochrane Database Syst Rev. 2011, 7, CD001800. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Corrà, U.; Benzer, W.; Bjarnason Wehrens, B.; Dendale, P.; Gaita, D.; et al. Secondary prevention through cardiac rehabilitation: from knowledge to implementation. A position paper from the Cardiac Rehabilitation Section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Prev Cardiol. 2010, 1, 1–17. [Google Scholar] [CrossRef]
- DeBacker GAmbrosioni, E.; Borch Johnson, K.; et al. European guidelines on cardiovascular disease prevention in clinical practice. Eur J Prev Rehabil. 2003, 10 (Suppl. 1), S1–S78. [Google Scholar]
- Bjarnason Wehrens, B.; Held, K.; Hoberg, E.; Karoff, M.; Rauch, B. Deutsche Leitlinie zur Rehabilitation von Patienten mit Herz Kreislauferkrankungen (DLL KardReha). Clin Res Cardiol. 2007, 2, 1–54. [Google Scholar] [CrossRef]
- Levine, G.N.; Bates, E.R.; Blankenship, J.C. 2011 ACCF/AHA/SCAI Guideline for PCI: executive summary. JACC. 2011, 58, 2550–2583. [Google Scholar] [CrossRef]
- Fraker, T.D.; Fihn, S.D. 2007 chronic angina focused update of the AHA/ ACC 2002 guidelines for the management of patients with chronic stable angina. J Am Coll Cardiol. 2007, 50, 2264–2274. [Google Scholar] [CrossRef]
- Papadakis, S.; Reid, R.R.; Coyle, D.; Beaton, L.; Angus, D.; Oldridge, N. Costeffectiveness of cardiac rehabilitation program delivery models in patients at varying cardic risk, reason for referral and sex. Eur J Cardiovasc Prev Rehab. 2008, 15, 347–353. [Google Scholar] [CrossRef]
- Leon, A.S.; Franklin, B.A.; Costa, F.; Balady, G.J.; Berra, K.A.; Stewart, K.J.; et al. Cardiac rehabilitation and secondary prevention of coronary heart disease. Circulation. 2005, 111, 369–376. [Google Scholar] [CrossRef]
- Arroll, B.; Khin, N.; Kerse, N. Screening for depression in primary care with two verbally asked questions: cross sectional study. BMJ. 2003, 327, 1144–1146. [Google Scholar] [CrossRef]
- Bjarnason Wehrens, B. Kardiologische Rehabilitation in Europa. Clin Res Cardiol. 2009, 4, 82–88. [Google Scholar] [CrossRef]
- Van Engen Verheul, M.; de Vries, H.; Kemps, H.; Kraaijenhagen, R.; de Keizer, N.; Peek, N. Cardiac Rehabilitation uptake and its determinants in the Netherlands. Eur J Prev Cardiol. 2012; epub. [Google Scholar] [CrossRef]
- Parashar, S.; Spertus, J.A.; Tang, F.; Bishop, K.L.; Vaccarino, V.; Jackson, C.F.; et al. Predictors of early and late enrollment in cardiac rehabilitaton among those referred after acute myocardial infarction. Circulation. 2012, 126, 1587–1595. [Google Scholar] [CrossRef]
- Kwan, G.; Balady, G.J. Cardiac Rehabilitation: Advancing the field through emerging science. Circulation. 2012, 125, e369–e373. [Google Scholar] [CrossRef]
- Evenson, K.R.; Rosamond, W.D.; Luepker, R.V. Predictors of outpatient cardiac rehabilitation utilization: The Minnesota Heart Survey Registry. J Cardiopulm Rehabil. 1998, 18, 192–198. [Google Scholar] [CrossRef] [PubMed]
- Maeder, M.; Windecker, S.; Roffi, M.; Kaiser, C.A.; Stauffer, J.C.; Pedrazzini, G.; Rickli, H. Interventional Cardiology in Switzerland during the year 2007. Kardiovaskuläre Medizin. 2010, 13, 18–24. [Google Scholar]
- Koçer, O.; Wachter, M.; Zellweger, M.J.; Piazzalonga, S.; Hoffmann, A. Prevalence of depressive symptoms and wellbeing during and up to nine years after outpatient cardiac rehabilitation. Swiss Med Wkly. 2011, 141, w13242. [Google Scholar] [CrossRef] [PubMed]
- Pfiffner, D.; Hoffmann, A. Psychosocial predictors of death for low risk patients after a first myocardial infarction: a 7 year follow up study. J Cardiopulm Rehabil. 2004, 24, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Ades, P.A.; Waldmann, M.L.; McCann, W.J.; Weaver, S.O. Predictors of cardiac rehabilitation participation in older coronary patients. Arch Intern Med. 1992, 152, 1033–1035. [Google Scholar] [CrossRef]
- Bittner, V.; Sanderson, B.; Breland, J.; Green, D. Referral patterns to a university based cardiac rehabilitation program. Am J Cardiol. 1999, 83, 252–255. [Google Scholar] [CrossRef] [PubMed]
- Schwaab, B.; Riemer, T.; Schneider, S.; Gohlke, H.; Katus, H.; Senges, J.; et al. Cardiac rehabilitation after acute myocardial infarction – effect on mortality, morbidity, medication and lifestyle changes. Eur Heart J. 2011, 32, 389. [Google Scholar]

© 2013 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Hoffmann, A.; Spinnler, B., 2; Buchs, M.; Eckstein, F.; Kaiser, C.A. Rehabilitation Enrollment After Cardiac Procedures. Cardiovasc. Med. 2013, 16, 203. https://doi.org/10.4414/cvm.2013.00169
Hoffmann A, Spinnler B 2, Buchs M, Eckstein F, Kaiser CA. Rehabilitation Enrollment After Cardiac Procedures. Cardiovascular Medicine. 2013; 16(7-8):203. https://doi.org/10.4414/cvm.2013.00169
Chicago/Turabian StyleHoffmann, Andreas, Bettina Spinnler, 2, Martina Buchs, Friedrich Eckstein, and Christoph A. Kaiser. 2013. "Rehabilitation Enrollment After Cardiac Procedures" Cardiovascular Medicine 16, no. 7-8: 203. https://doi.org/10.4414/cvm.2013.00169
APA StyleHoffmann, A., Spinnler, B., 2, Buchs, M., Eckstein, F., & Kaiser, C. A. (2013). Rehabilitation Enrollment After Cardiac Procedures. Cardiovascular Medicine, 16(7-8), 203. https://doi.org/10.4414/cvm.2013.00169




