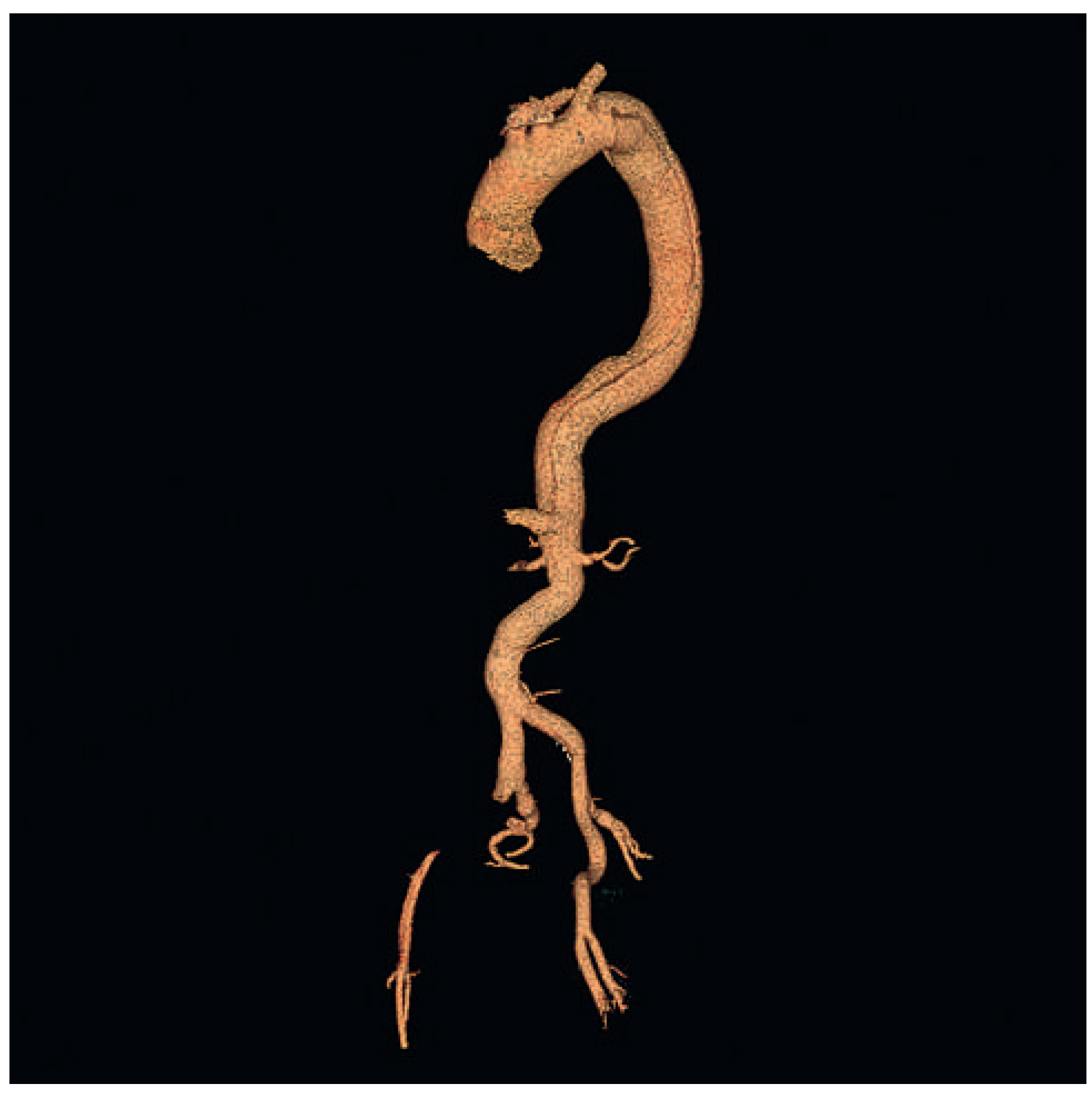
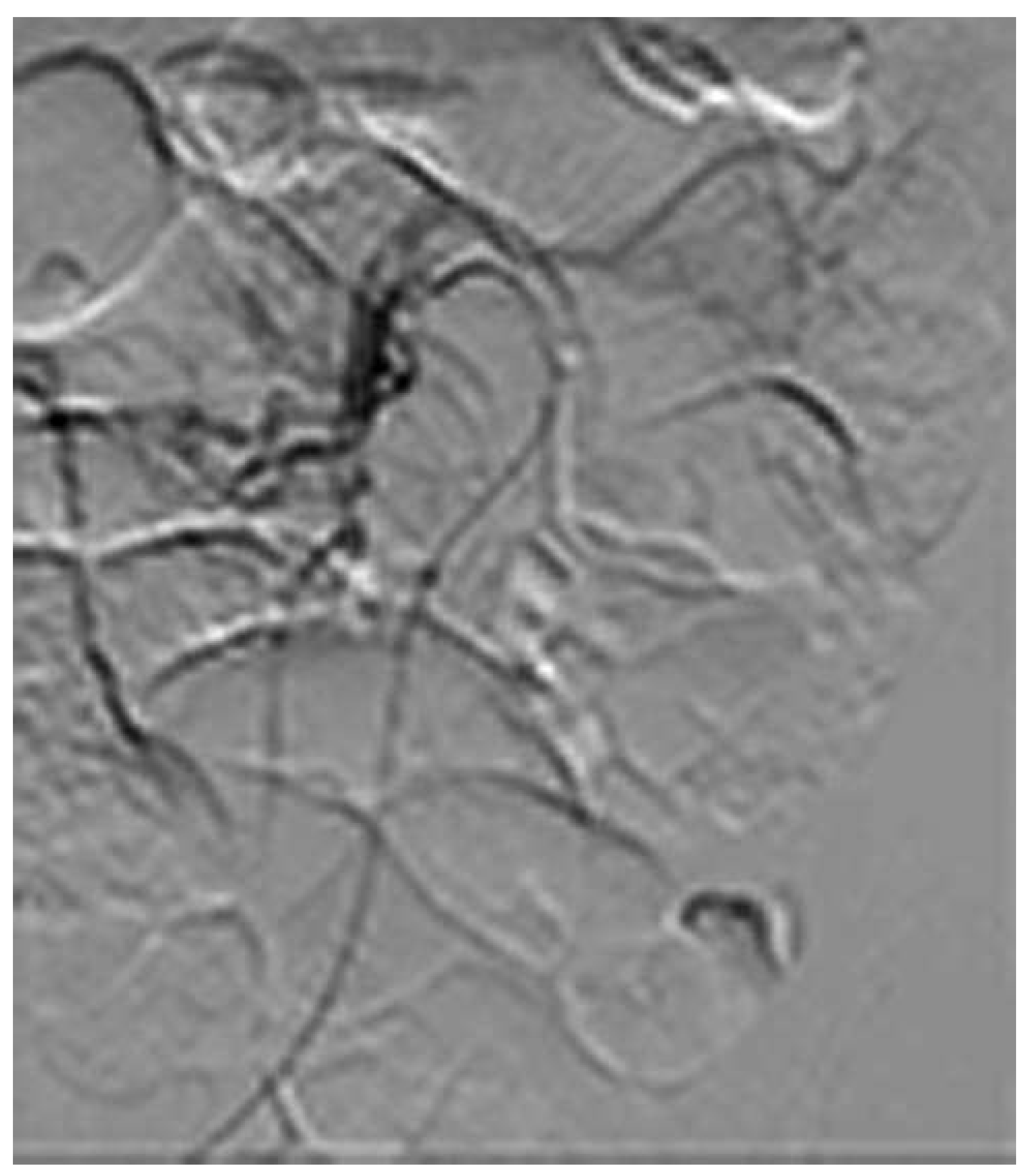
Endovascular Treatment of a Complex Type B Aortic Dissection
Summary
Introduction
Case report
Discussion
Funding
Conflicts of Interest
References
- Akin, I.; Kische, S.; Ince, H.; Nienaber, C. Penetrating aortic ulcer, intramural hematoma, acute aortic syndrome: when to do what. J Cardiovasc Surg (Torino). 2012, 53 (Suppl. 1), 83–90. [Google Scholar] [PubMed]
- Trimarchi, S.; Tolenaar, J.L.; Tsai, T.T.; Froehlich, J.; Pegorer, M.; Upchurch, G.R.; et al. Influence of clinical presentation on the outcome of acute B aortic dissection: evidences from IRAD. J Cardiovasc Surg (Torino). 2012, 53, 161–168. [Google Scholar] [PubMed]
- Tsai, T.T.; Fattori, R.; Trimarchi, S.; Isselbacher, E.; Myrmel, T.; Evangelista, A.; et al. Long-term survival in patients presenting with type B acute aortic dissection: insights from the International Registry of Acute Aortic Dissection. Circulation. 2006, 114, 2226–2231. [Google Scholar] [CrossRef] [PubMed]
- Henke, P.K.; Williams, D.M.; Upchurch, G.R., Jr.; Proctor, M.; Cooper, J.V.; Fang, J.; et al. Acute limb ischemia associated with type B aortic dissection: clinical relevance and therapy. Surgery. 2006, 140, 532–539. [Google Scholar] [CrossRef] [PubMed]
- Di Eusanio, M.; Trimarchi, S.; Patel, H.J.; Hutchison, S.; Suzuki, T.; Peterson, M.D.; et al. Clinical presentation, management, and short-term outcome of patients with type A acute dissection complicated by mesenteric malperfusion: observations from the International Registry of Acute Aortic Dissection. J Thorac Cardiovasc Surg. 2013, 145, 385–390. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.M.; Lee, D.Y.; Hamilton, B.H.; Marx, M.V.; Narasimham, D.L.; Kazanjian, S.N.; et al. The dissected aorta: part III. Anatomy and radiologic diagnosis of branch-vessel compromise. Radiology. 1997, 203, 37–44. [Google Scholar] [CrossRef] [PubMed]
- Nienaber, C.A.; Kische, S.; Zeller, T.; Rehders, T.C.; Schneider, H.; Lorenzen, B.; et al. Provisional extension to induce complete attachment after stentgraft placement in type B aortic dissection: the PETTICOAT concept. J Endovasc Ther. 2006, 13, 738–746. [Google Scholar] [CrossRef] [PubMed]




© 2013 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Li, W.-D.; Meng, Q.-Y.; Zhu, L.-W.; Wang, W.-B.; Zhang, Y.-Q.; Li, C.-L.; Li, X.-Q. Endovascular Treatment of a Complex Type B Aortic Dissection. Cardiovasc. Med. 2013, 16, 267. https://doi.org/10.4414/cvm.2013.00187
Li W-D, Meng Q-Y, Zhu L-W, Wang W-B, Zhang Y-Q, Li C-L, Li X-Q. Endovascular Treatment of a Complex Type B Aortic Dissection. Cardiovascular Medicine. 2013; 16(10):267. https://doi.org/10.4414/cvm.2013.00187
Chicago/Turabian StyleLi, Wen-Dong, Qing-You Meng, Li-Wei Zhu, Wen-Bin Wang, Ye-Qing Zhang, Cheng-Long Li, and Xiao-Qiang Li. 2013. "Endovascular Treatment of a Complex Type B Aortic Dissection" Cardiovascular Medicine 16, no. 10: 267. https://doi.org/10.4414/cvm.2013.00187
APA StyleLi, W.-D., Meng, Q.-Y., Zhu, L.-W., Wang, W.-B., Zhang, Y.-Q., Li, C.-L., & Li, X.-Q. (2013). Endovascular Treatment of a Complex Type B Aortic Dissection. Cardiovascular Medicine, 16(10), 267. https://doi.org/10.4414/cvm.2013.00187



