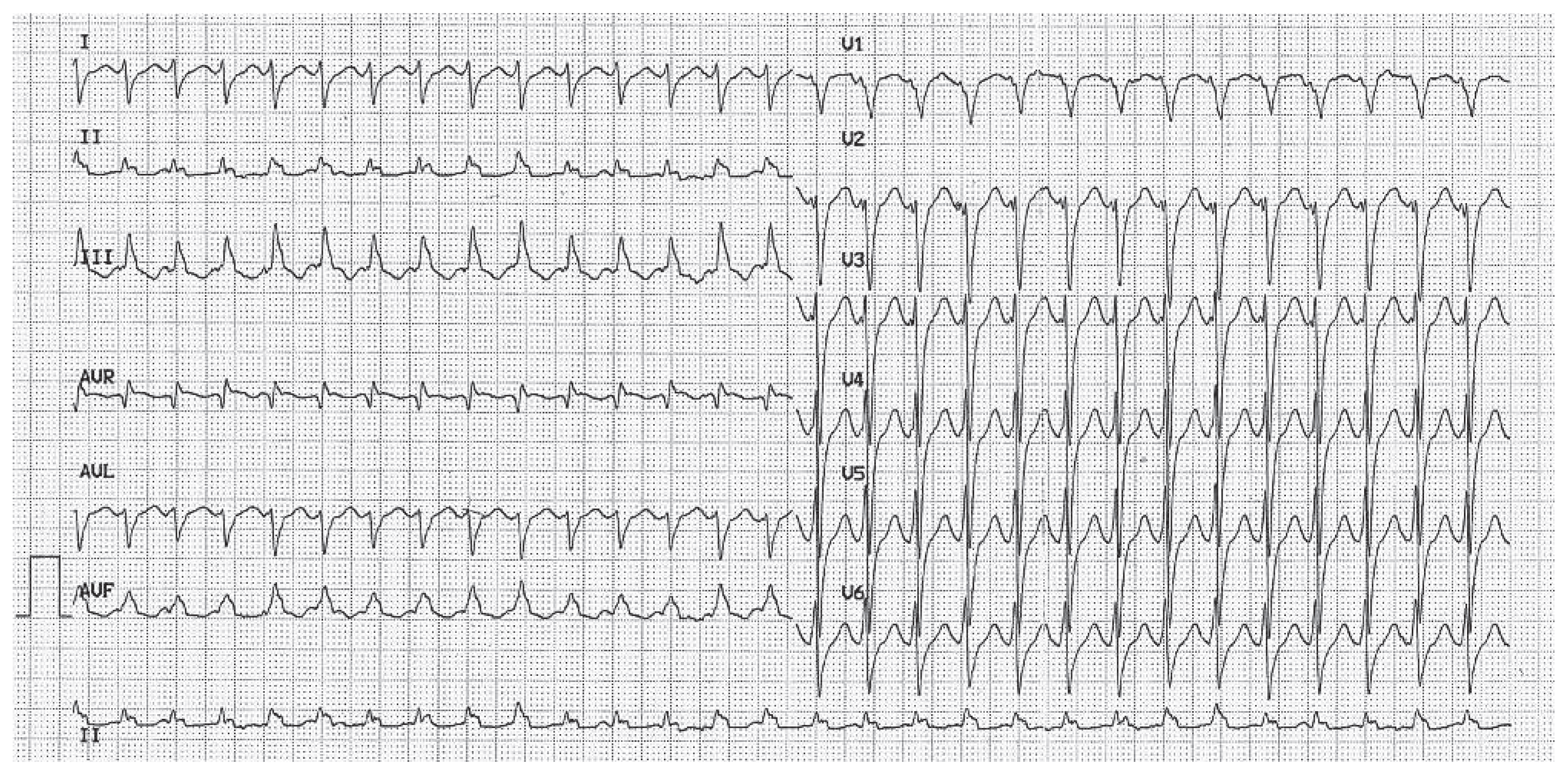
A Tachycardia with QRS Duration Narrower Than That During Sinus Rhythm
Case Presentation
Questions
Comments
Funding/Potential Competing Interests
References
- Akihiko Nogami, M.D. Purkinje-related arrythmias Part I: Monomorphic ventricular tachycardias. PACE 2011, 34, 624–650. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, M.; Kobayashi, Y.; Iwasaki, Y.K.; Morita, N.; Miyauchi, Y.; Kato, T. Novel mechanism of postinfarction ventricular tachycardia originating in surviving left posterior Purkinje fibers. Heart Rhythm. 2006, 3, 908–918. [Google Scholar] [CrossRef]

© 2012 by the author. Attribution-Non-Commercial-NoDerivatives 4.0.
Share and Cite
Longchamp, D.Z.; Pruvot, E. A Tachycardia with QRS Duration Narrower Than That During Sinus Rhythm. Cardiovasc. Med. 2012, 15, 296. https://doi.org/10.4414/cvm.2012.00107
Longchamp DZ, Pruvot E. A Tachycardia with QRS Duration Narrower Than That During Sinus Rhythm. Cardiovascular Medicine. 2012; 15(10):296. https://doi.org/10.4414/cvm.2012.00107
Chicago/Turabian StyleLongchamp, Danielle Zaugg, and Etienne Pruvot. 2012. "A Tachycardia with QRS Duration Narrower Than That During Sinus Rhythm" Cardiovascular Medicine 15, no. 10: 296. https://doi.org/10.4414/cvm.2012.00107
APA StyleLongchamp, D. Z., & Pruvot, E. (2012). A Tachycardia with QRS Duration Narrower Than That During Sinus Rhythm. Cardiovascular Medicine, 15(10), 296. https://doi.org/10.4414/cvm.2012.00107



