Introduction
Dyslipidaemia represents one of the major risk factors for cardiovascular disease [
1]. In the last two decades, a large number of outcome-based clinical trials have convincingly demonstrated that lowering cholesterol levels – particularly with statins – leads to a significant reduction of the risk of developing cardiovascular disease in various populations [
2,
3]. Moreover, lipid lowering therapy was shown to significantly reduce the risk of cardiovascular events in patients with already established cardiovascular disease, including those with coronary heart disease (CHD) who are considered to be at high risk for cardiovascular events [
2,
3].
Based on current evidence, American, European and other societies have published guidelines on the prevention of cardiovascular disease which include recommendations for lipid management in the setting of primary and secondary prevention [
4,
5,
6,
7]. Consistently, all these guidelines recommend a target low density lipoprotein cholesterol (LDL-C) level <2.6 mmol/l to be achieved in high-risk patients such as those with established CHD. Notably, recent surveys indicated that adherence to these guidelines has improved in the last years in various European countries [
8,
9]. In Switzerland, a national survey on the prescription of cardiovascular drugs among outpatients with CHD had been performed in the years 2000/2001 [
10]. Although this survey demonstrated that evidence-based prescription of lipid lowering drugs had improved compared to former surveys, this study also revealed that lipid lowering drugs were still underused and that target LDL-C levels were not reached in a considerable proportion of Swiss outpatients with CHD in general practice. Since then, Swiss national guidelines on the prevention of atherosclerotic disease were published by the Swiss Working Group for Lipids and Atherosclerosis (AGLA) and the Swiss Society of Cardiology (SGK) in 2005 [
11]. However, it is unknown whether the implementation of these guidelines was associated with an improvement of lipid management in high-risk outpatients in Switzerland.
Thus, the aim of the present study was to assess the current quality of lipid management in high-risk patients, that is, patients with known CHD and a history of myocardial infarction, in general practice in Graubuenden, Switzerland.
Results
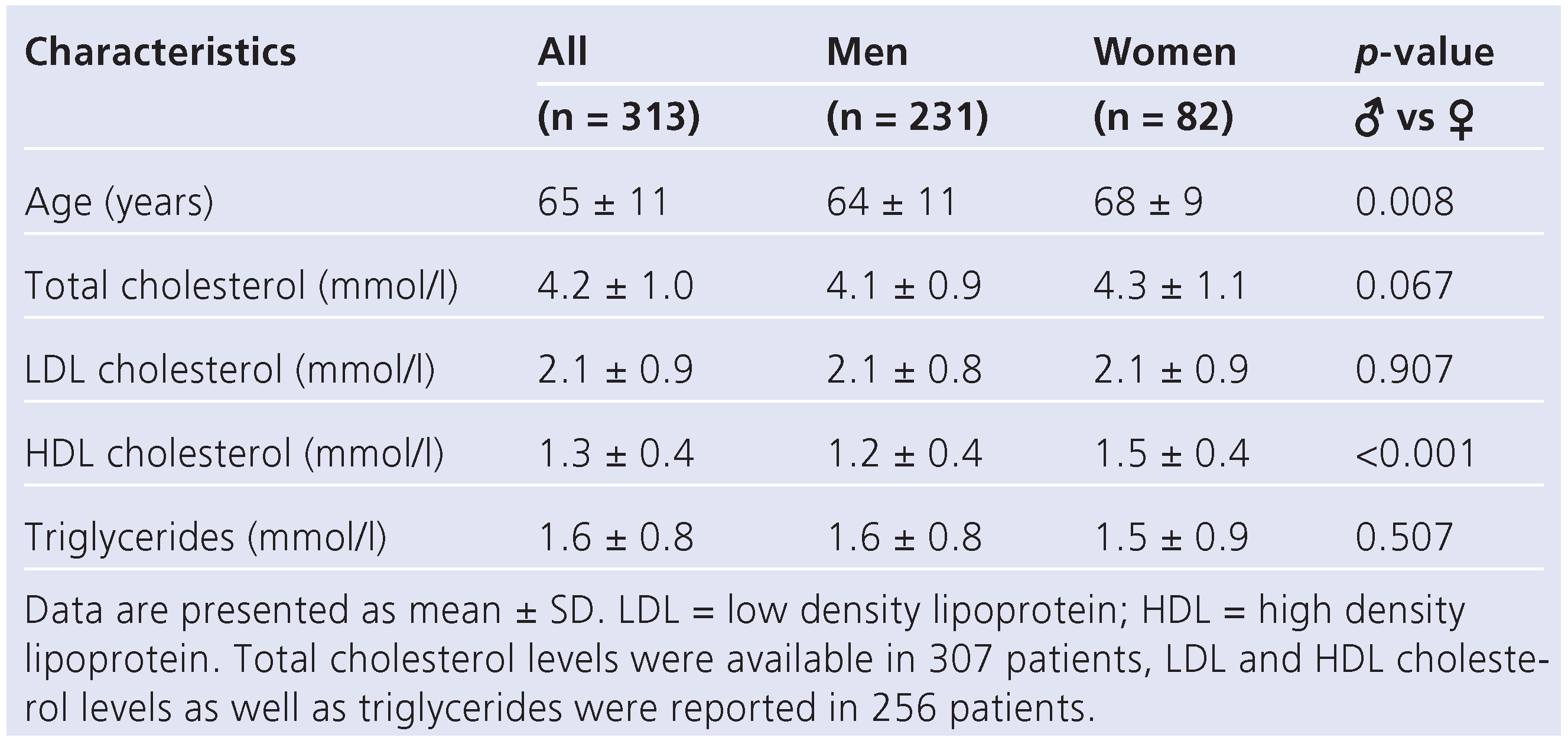
At least one questionnaire was returned by 114 of all 128 contacted primary care physicians (89%). By December 2009, a total of 323 questionnaires had been returned, corresponding to a return rate of 83%. Of these patients, 10 (3%) had died since the index event. Thus, questionnaires regarding 313 patients (80% of the entire study cohort) were included in the final analysis. Of these, 231 (74%) were men and 82 (26%) were women. Male patients were younger, had lower average HDL-C levels and tended to have lower total cholesterol levels, whereas levels of LDL-C and triglycerides were similar among both sexes (
Table 1). The average time interval between the index myocardial infarction and the completion of the questionnaire was 24 ± 10 months (range: 5–43 months).
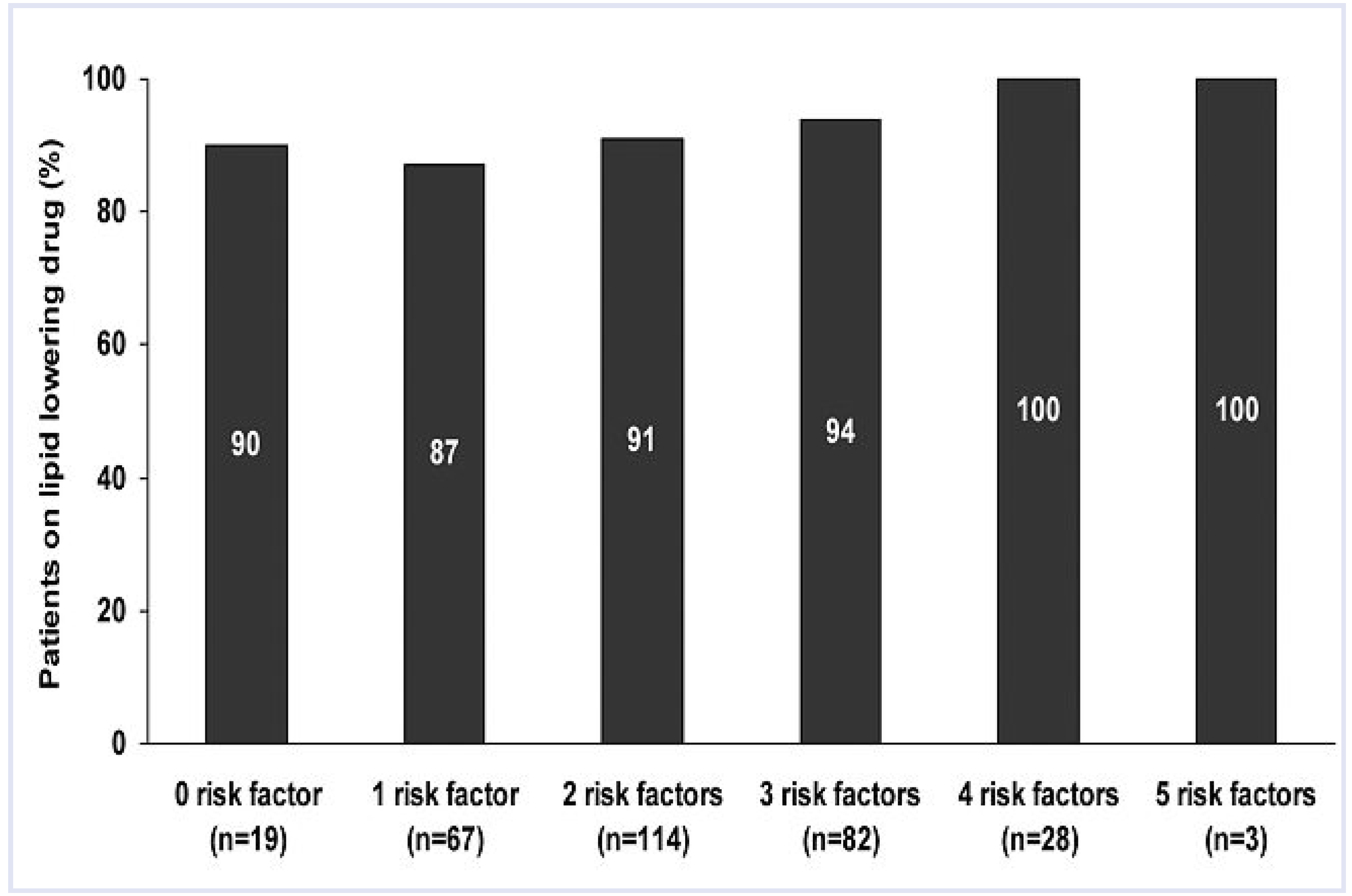
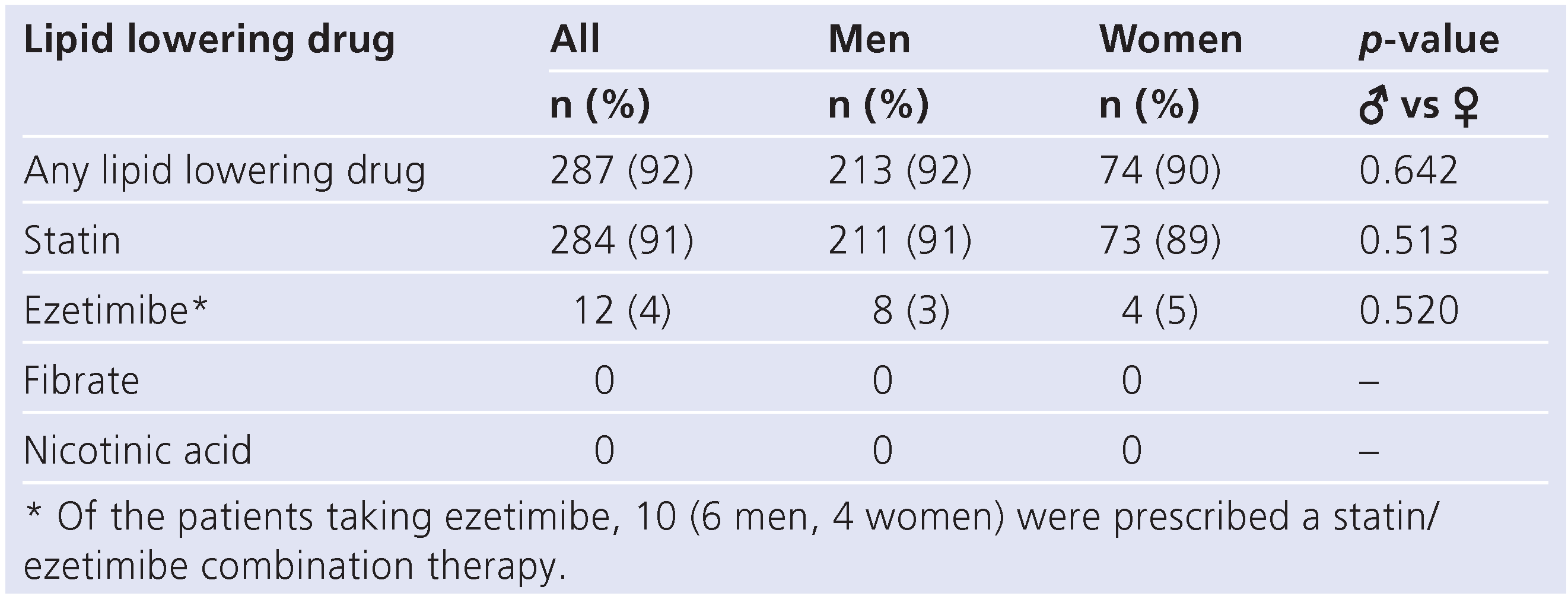
A total of 287 patients (92%) had a lipid lowering drug prescribed to them (
Table 2). Of these, 99% used a statin, resulting in an overall statin use of 91% (
Table 2,
Figure 1). Ezetimibe was only used by a minority of patients and fibrates or nicotinic acid were not prescribed in our population. The prescription rate of lipid lowering drugs was independent of the number of risk factors present in an individual (
Figure 2). The reason for not prescribing a lipid lowering drug was reported in 25 of 26 patients without lipid lowering therapy. In 9 individuals, lipid lowering therapy was deemed unnecessary because lipid levels were considered to be in the therapeutic range without therapy. This decision was based on a fasting LDL-C level <2.6 mmol/l in 4 patients and on a fasting total cholesterol level <5.0 mmol/l in 4 patients. However, 1 of these patients was not prescribed lipid lowering therapy although his LDL-C and total cholesterol levels were above the target values (3.7 mmol/l and 5.3 mmol/l, respectively). Malcompliance, prior side effects to lipid lowering drugs and comorbidities were the reasons for not prescribing lipid lowering therapy in 7, 5 and 4 patients, respectively. The prescription rate of lipid lowering drugs did not depend on the time interval between the index event and the completion of the questionnaire (data not shown).
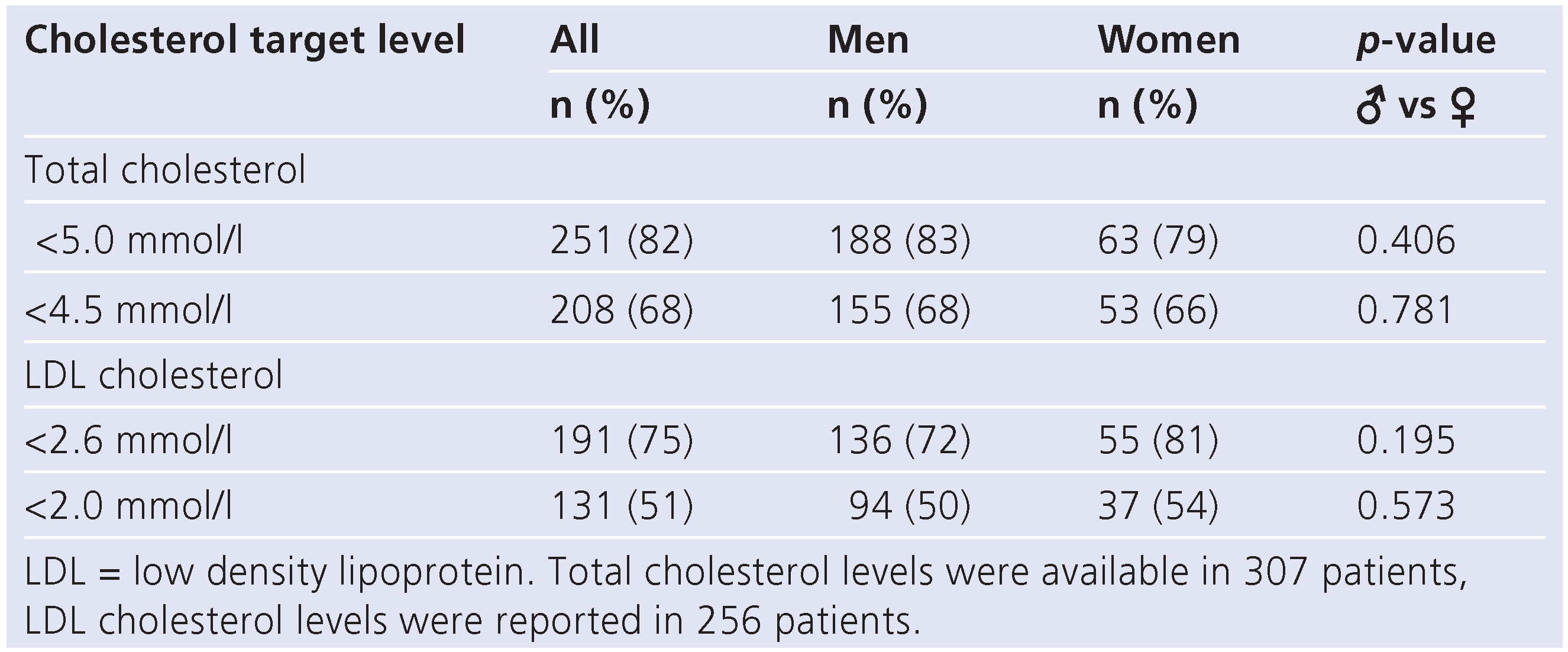
In the present survey, lipid levels were available for 307 patients. In these, total cholesterol and cholesterol subfractions were reported in 256 patients (83%), whereas only total cholesterol (but not cholesterol subfractions) was reported in 51 individuals (17%). Of the individuals with reported total cholesterol values, 82% had a total cholesterol level <5.0 mmol/l, while 68% achieved a total cholesterol level <4.5 mmol/l (
Table 3). Of the patients with reported LDL-C values, 75% achieved the target LDL-C level <2.6 mmol/l and 51% had an LDL-C level <2.0 mmol/l (
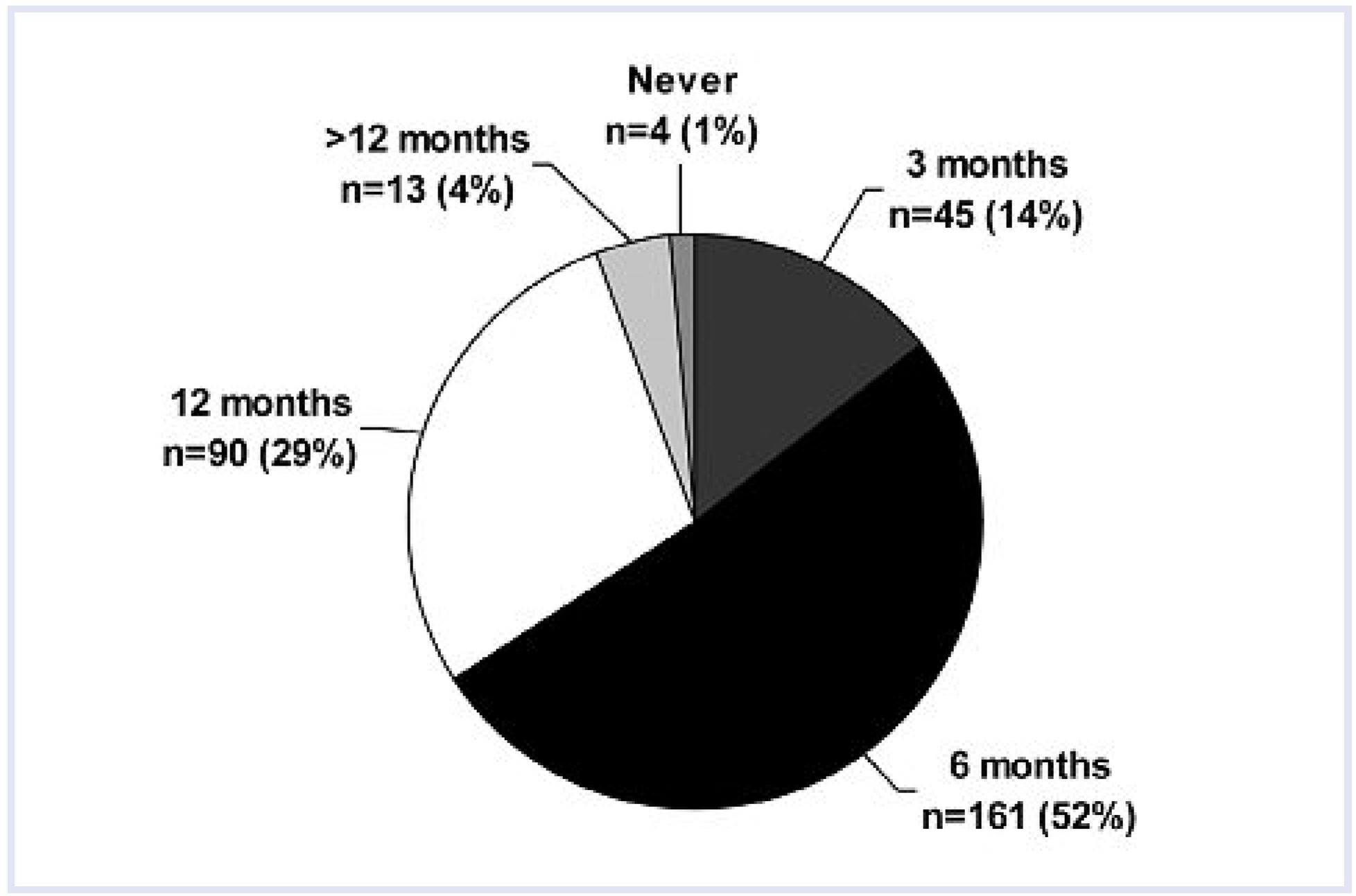
Table 3). According to the participating primary care physicians, lipid levels were assessed at least once per year in 95% of all patients (
Figure 3).
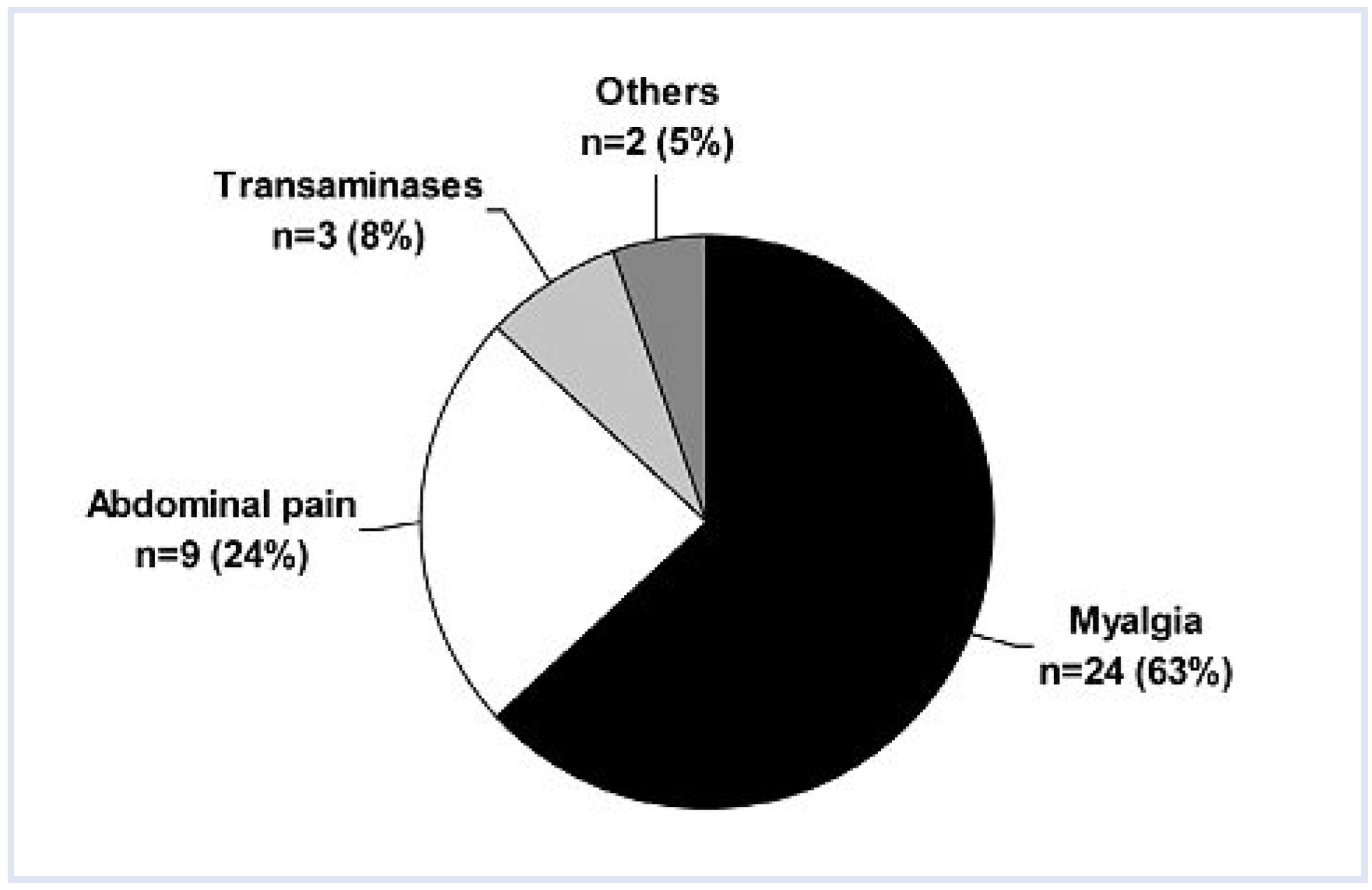
Side effects of lipid lowering therapy were reported in 38 patients (12% of the study population). In one patient abdominal pain occurred in response to ezetimibe, whereas all other side effects were observed under statin therapy. Myalgia (i.e., muscle pain without a rise in the creatine kinase concentration to greater than ten times the upper limit of normal) was the most common side effect reported (
Figure 4). To our knowledge, however, no case of myopathy (i.e., any muscle symptom – pain, tenderness, or weakness – accompanied by a creatine kinase concentration greater than ten times the upper limit of normal) was observed in our population. Side effects led to a change in lipid lowering therapy in 25 patients (8% of the study population) and to a discontinuation of lipid lowering therapy in 8 patients (3% of the study population). In 5 patients (2% of the study population), lipid lowering therapy was continued despite the side effect.
A total of 197 patients (63%) participated in a cardiac rehabilitation programme after the index event. In these patients, the prescription rate of lipid lowering drugs was significantly higher than in those who did not participate in such a program (94% vs 87%; p = 0.023). However, average LDL cholesterol levels did not differ among patients who participated in a cardiac rehabilitation programme and those who did not (2.1 ± 0.8 mmol/l vs 2.2 ± 0.9 mmol/l, p = 0.555).
A total of 271 out of all included patients (87%) were given some kind of specific counselling with regard to measures for lifestyle improvement by their primary care physicians in the course of their disease. Notably, such counselling was considered to be at least partly successful and worth the effort and time by the participating physicians in the majority of patients (
Figure 5).
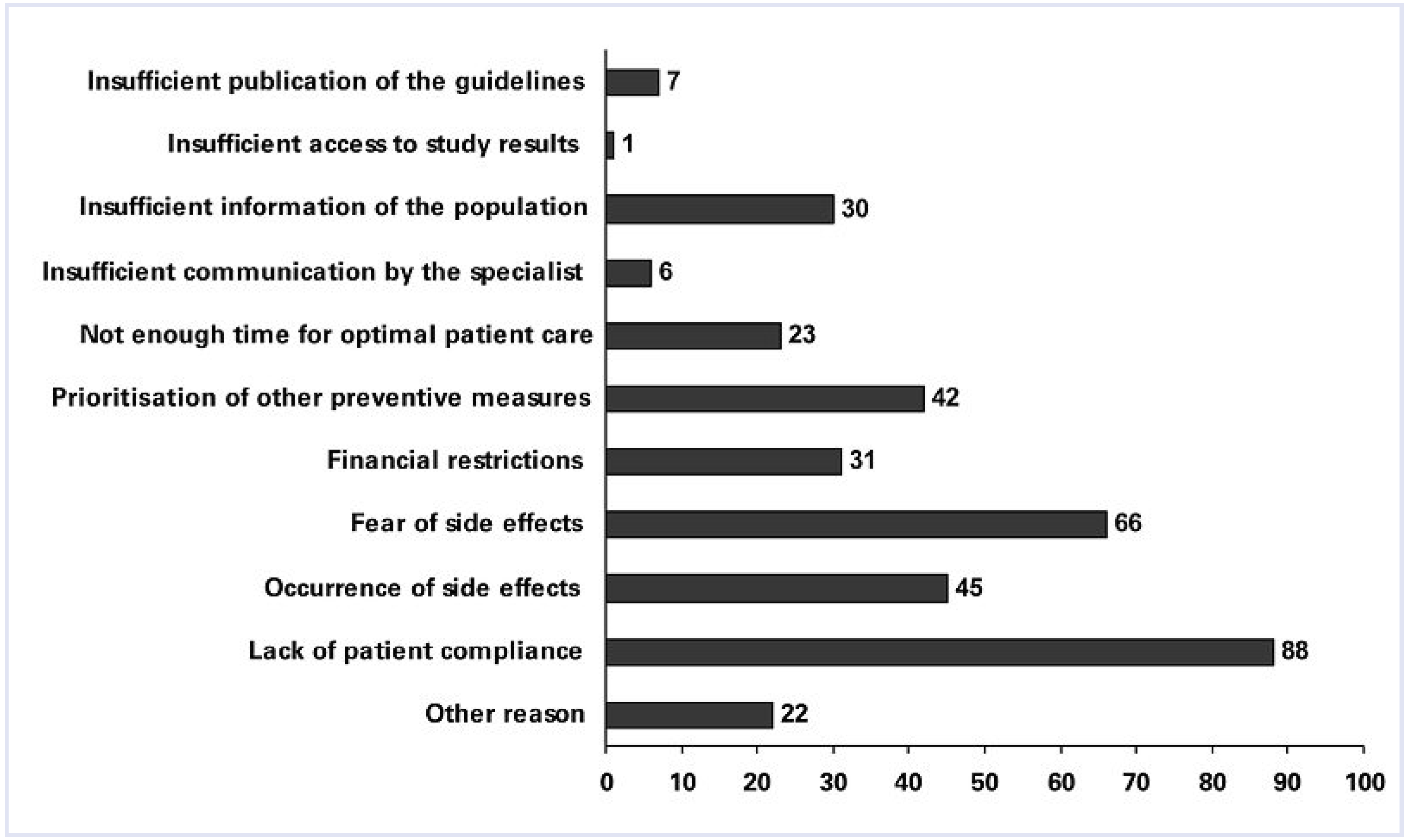
According to the participating primary care physicians, lack of patient compliance was regarded as the most important reason for not achieving the lipid targets in outpatients with CHD in general practice (
Figure 6).
Discussion
The present survey assessing lipid lowering therapy among outpatients with CHD and a history of myocardial infarction demonstrated that current lipid management is performed according to national and international guidelines in the majority of affected individuals in Graubuenden, Switzerland.
A nation-wide survey in 2000/2001 had shown that lipid management was insufficient and that target lipid levels were not met in a considerable proportion of patients with established CHD in Switzerland [
10]. At that time, for example, only 63% of all patients with CHD were prescribed lipid lowering drugs and 60% had serum lipid levels above the intervention cut-off according to the former 1999 Swiss recommendations, which were less strict than current recommendations and included the presence of two of the following three criteria: total cholesterol >5.0 mmol/l, LDL-C >3.0 mmol/l, and total cholesterol/HDL-C ratio >5 [
11,
12]. Although lipid management was slightly better within a subset of patients with a history of myocardial infarction or coronary revascularisation in 2000/2001 (prescription of lipid lowering drugs in 82%, total cholesterol >5 mmol/l in 56%), our data suggest that lipid management of patients with CHD has improved during the last decade in Switzerland. Notably, our results also indicate that the prescription rate of lipid lowering drugs and the achievement of target lipid values are similar in both sexes.
The EUROASPIRE I, II, and III surveys assessed risk factor management in CHD patients in various European countries in 1995/1996, 1999/2000, and 2006/2007 [
8,
9]. In this programme, a gradual improvement of the prescription rate of lipid lowering drugs and of lipid control could be observed over time. In the EUROASPIRE III survey, 89% of all patients received a lipid lowering drug, which was a statin in most cases (87% of all patients). Thus, the prescription rates of lipid lowering drugs and statins (92% and 91%, respectively) found in the current survey are comparable with those in other European countries.
The prevalence of a total cholesterol level <5.0 mmol or <4.5 mmol/l and of an LDL-C level <2.6 mmol/l was 72%, 54% and 53% in the EUROASPIRE III survey [
8,
9]. In our survey the respective proportions were 82%, 68% and 75%. Therefore, our results compare well with those of the EUROASPIRE III survey. However, despite these favourable results, it needs to be emphasised that still one quarter of all our patients with a history of myocardial infarction had an LDL-C level above the recommended target level of <2.6 mmol/l.
Recent evidence has suggested that lowering LDL-C levels below currently recommended targets results in improved outcomes [
13]. Thus, advocates of a “lower is better strategy” propose an LDL-C goal of <2.0 mmol/l as a therapeutic option in patients who are considered to be at very high risk [
13,
14]. In our survey, about half of all patients had LDL-C values <2.0 mmol/l. This demonstrates that achievement of LDL-C levels below the current intervention cut-off is feasible in a considerable proportion of outpatients with CHD.
A minority of our patients were not prescribed a lipid lowering drug. In some patients, therapy was withheld because their lipid levels were considered to be in the target range without therapy. However, this decision was not justified in 5 individuals based on an LDL-C level >2.6 mmol/l. Also, only total cholesterol levels and not cholesterol subfractions were measured in 17% of all patients included in the present survey. Taken together, these observations suggest that a minority of primary care physicians are not familiar with current national guidelines.
Only 4 patients were not treated with a lipid lowering drug because of prior therapeutic side effects. However, side effects of lipid lowering therapy (all except one occurred during statin therapy) were reported in 12% of the study population, with myalgia being the most frequent. It is well known that all statins can cause myopathy and rhabdomyolysis. However, there is no clear evidence from randomised trials that statins cause myalgia, although this is widely believed [
15]. Pooled data from randomised clinical trials with various statins indicate that the frequency of myalgia is similar in patients receiving statins or placebo [
15]. Thus, whether the reported cases of myalgia were, indeed, caused by statin therapy is debatable. Furthermore, our data demonstrate that for most people statins are safe and well-tolerated.
Lack of patient compliance was named as the reason for not prescribing lipid lowering therapy in only 7 patients. However, according to the participating primary care physicians, lack of patient compliance was considered to be the main reason for not reaching target lipid levels in daily practice. Insufficient patient knowledge about the risk factor “dyslipidaemia” represents a key factor for poor patient compliance [
16]. Therefore, the fact that participating primary care physicians put a lot of effort into patient counselling in most included individuals might explain why lack of patient compliance was not a major issue in our population. In this regard, the current data underline that good communication between primary care physicians and their patients is a key factor to enhance patient compliance. In order to further enhance patient compliance, improving information for patients with dyslipidaemia is one of the goals of the currently ongoing “Swiss Cholesterol Network” campaign of the Swiss Working Group for Lipids and Atherosclerosis (AGLA) and the Swiss Society of Cardiology (SGK) [
17]. However, although the effectiveness of lipid lowering therapy crucially depends on the patient’s compliance, it must be emphasised that improving compliance by specific initiatives does not necessarily translate into an increase in the number of patients achieving target lipid levels [
18].
The current survey has some limitations. Firstly, as in all voluntary questionnaire-based surveys reporting bias might have affected our results. However, the high participation rate of contacted primary care physicians as well as the excellent questionnaire return rate suggests that reporting bias is not a major issue in the present survey. Secondly, cholesterol levels were not reported in a minority of the patients, however this is unlikely to affect the overall findings of our survey. Thirdly, our survey was limited to individuals with a history of myocardial infarction, which represents a subset of very high risk CHD patients, who may particularly benefit from optimal lipid management. Thus, our results must be interpreted with caution and may not apply to all CHD patients. Indeed, a recent Swiss survey on cardiovascular risk management in daily practice indicated that lipid management is insufficient in patients at risk for cardiovascular events with only 71% of those considered to be at high risk (PROCAM score >20% or known CHD or known diabetes mellitus) being treated and only 37% reaching an LDL-C level <2.6 mmol/l [
19]. However, in this survey, only 47% of all included high risk patients had known CHD and no information was given regarding the proportion of patients with prior myocardial infarction. Thus, given the results of our survey, it may be speculated that a history of myocardial infarction is associated with more consequent lipid management in outpatients with CHD.
In conclusion, the results of our representative survey demonstrated that the majority of patients with CHD and prior myocardial infarction were treated according to current national and international guidelines in Graubuenden, Switzerland. However, despite these encouraging results, target lipid levels are still not reached in about one fourth of all patients suggesting a potential for further improvement of lipid management in patients with CHD and a history of myocardial infarction.
The authors are indebted to all participating colleagues in private practice for their efforts and contribution.