Acute Myocardial Infarction in a 19 Year-Old Woman: Sometimes Hoofbeats are Zebras
Abstract
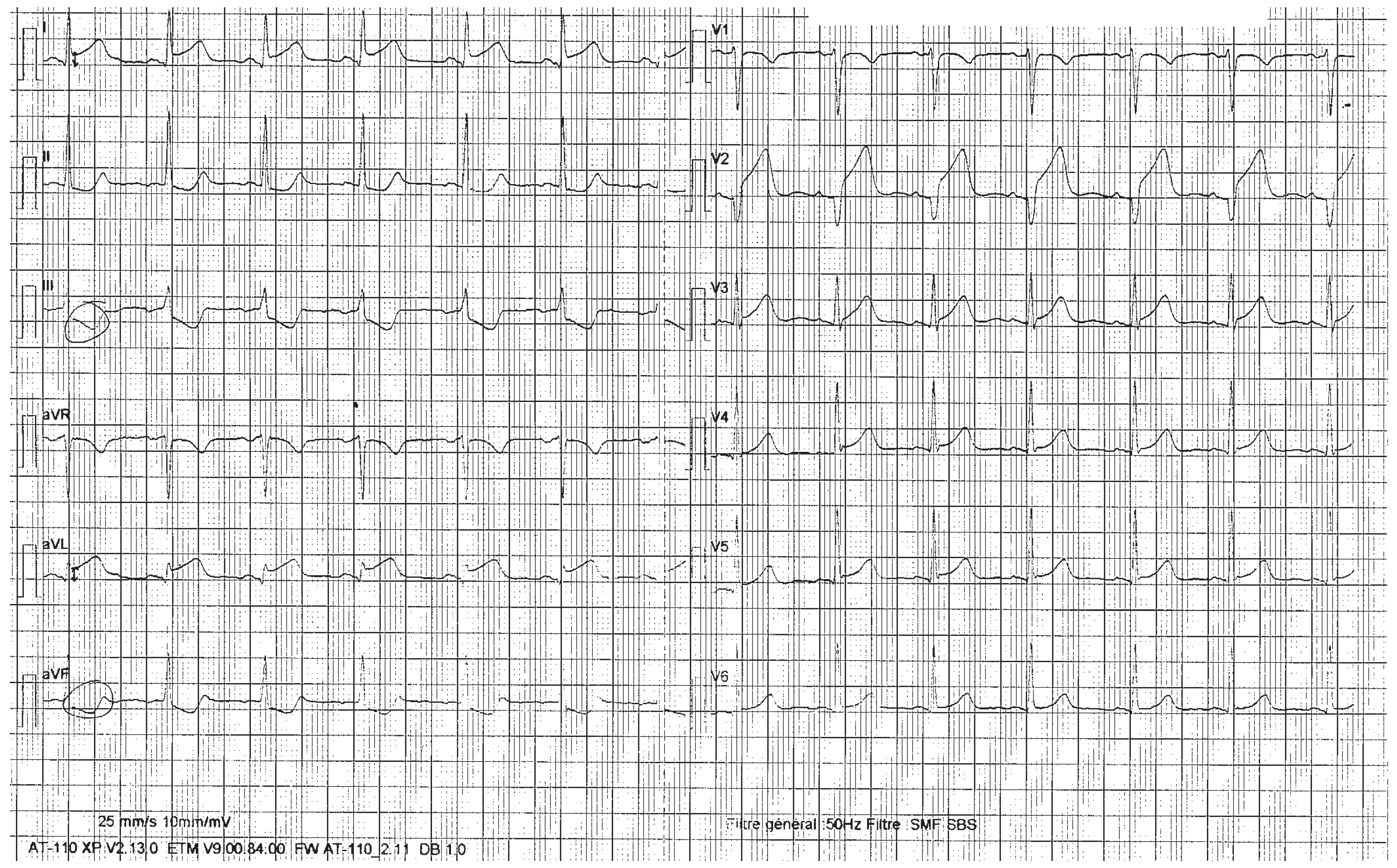
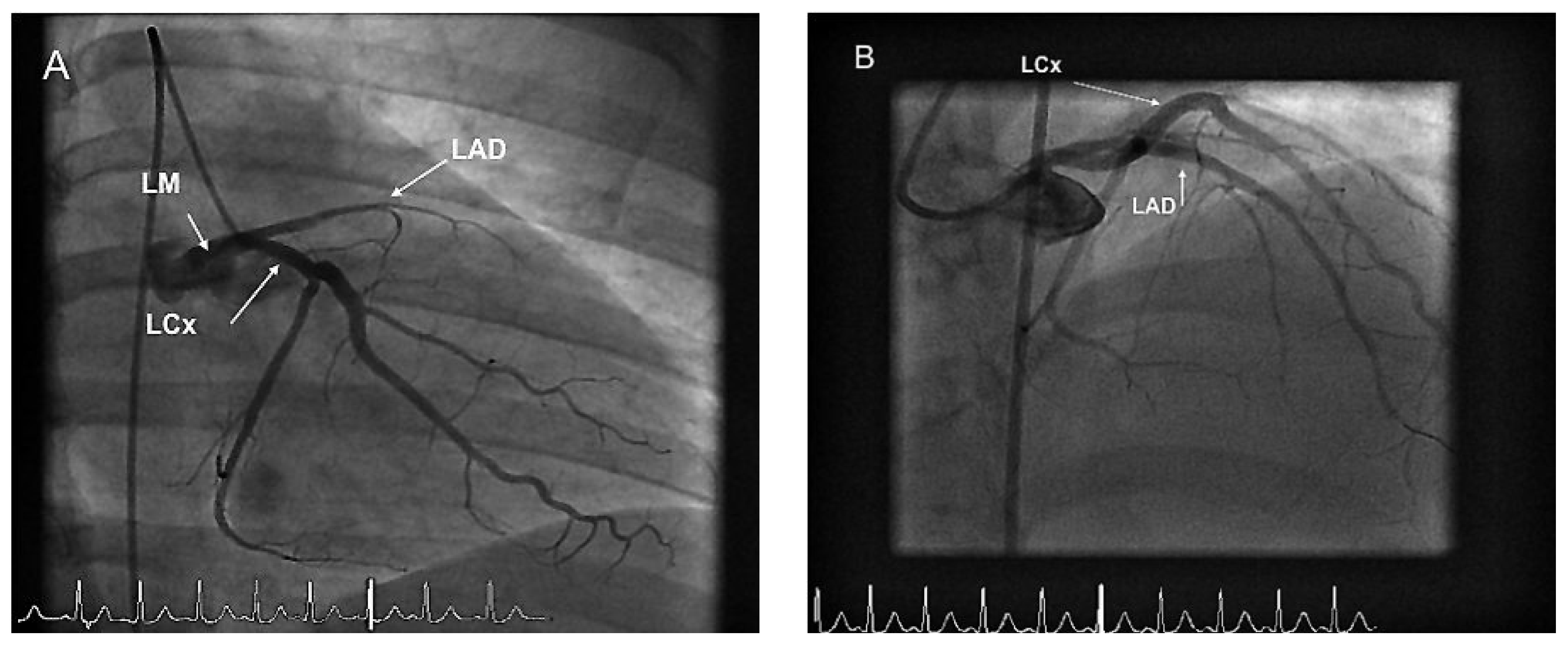
Case report
Discussion
Conflicts of Interest
References
- Doughty, M.; Mehta, R.; Bruckman, D.; et al. Acute myocardial infarction in the young—The University of Michigan experience. Am Heart J. 2002, 143, 56. [Google Scholar] [CrossRef] [PubMed]
- Schoenenberger, A.W.; Radovanovic, D.; Stauffer, J.C.; Windecker, S.; Urban, P.; Niedermaier, G.; et al. Acute coronary syndromes in young patiente: Presentation, treatment and outcome. Int J Cardiol. 2009. [CrossRef]
- Mukherjee, D.; Hsu, A.; Moliterno, D.J.; Lincoff, A.M.; Goormastic, M.; Topol, E.J. Risk factors for premature coronary artery disease and determinants of adverse outcomes after revascularisation in patients less than 40 years old. Am J Cardiol. 2003, 92, 1465–1467. [Google Scholar] [CrossRef] [PubMed]
- Jalowiec, D.A.; Hill, J.A. Myocardial infarction in the young and in women. Cardiovascular Clinics. 1989, 20, 197–206. [Google Scholar] [PubMed]
- Rosenberg, L.; Palmer, J.R.; Rao, R.S.; Shapiro, S. Low-dose oral contraceptive use and the risk of myocardial infarction. Arch Intern Med. 2001, 161, 1065. [Google Scholar] [CrossRef] [PubMed]
- Warren, S.E.; Thompson, S.I.; Vieweg, W.V. Historic and angiographic features of young adults surviving myocardial infarction. Chest. 1979, 75, 667–670. [Google Scholar] [CrossRef] [PubMed]
- Smith, B.A.; Grider, D.J. Sudden death in a young adult: sequelae of childhood Kawasaki disease. Am J Emer Med. 1993, 11, 381–383. [Google Scholar] [CrossRef] [PubMed]
- Wilson, V.E.; Eck, S.L.; Bates, E.R. Evaluation and treatment of acute myocardial infarction complicating systemic lupus erythematosis. Chest. 1992, 101, 420–424. [Google Scholar] [CrossRef] [PubMed]
- Vaarala, O. Antiphospholipid antibodies and athrtrosclerosis. Lupus. 1996, 5, 442–447. [Google Scholar] [CrossRef] [PubMed]
- Nygard, O.; Nordrehaug, J.E.; Refsum, H.; Ueland, P.M.; Farstad, M.; Vollset, S.E. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997, 337, 230–236. [Google Scholar] [CrossRef] [PubMed]
- Hollander, J.E.; Todd, K.H.; Green, G.; et al. Chest pain associated with cocaine: an assessment of prevalence in suburban and urban emergency departments. Ann Emerg Med. 1995, 26, 671–676. [Google Scholar] [CrossRef] [PubMed]
- Lange, R.A.; Hills, C.D. Cardiovascular complications of cocaine use. N Engl J Med. 2001, 345, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Fournier, J.A.; Sanchez, A.; Quero, J.; et al. Myocardial infarction in men aged 40 years or less: a prospective clinical-angiographic study. Clin Cardiol. 1996, 19, 631. [Google Scholar] [CrossRef] [PubMed]
- Morillas, P.; Bartomeu, V.; Pahon, P.; et al. Characteristics and outcome of acute myocardial infarction in young patients. The PRIAMHO II study, Cardiology. 2006, 107, 217–225. [Google Scholar] [CrossRef] [PubMed]
- Zimmerman, F.H.; Cameron, A.; Fisher, L.D. Myocardial infarction in young adults: angiographic characterization, risk factors and prognosis (Coronary Artery Surgery Study Registry). J Am Coll Cardiol. 1995, 26, 654. [Google Scholar] [CrossRef] [PubMed]
- Porter, A.; Wurzel, M.; Ben-Gal, T.; et al. Long-term prognosis of 210 patients who underwent coronary angiography before 40 years of age. Am J Cardiol. 1998, 81, 1168. [Google Scholar] [CrossRef] [PubMed]
- Cole, J.H.; Miller, J.I.; Sperling, L.S.; Weintraub, W.S. Longe-term follow up of coronary artery disease presenting in young adults. J Am Coll Cardiol. 2003, 41, 521. [Google Scholar] [CrossRef] [PubMed]
© 2011 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Arroyo, D.; Rutz, T.; Stauffer, J.-C. Acute Myocardial Infarction in a 19 Year-Old Woman: Sometimes Hoofbeats are Zebras. Cardiovasc. Med. 2011, 14, 95. https://doi.org/10.4414/cvm.2011.01576
Arroyo D, Rutz T, Stauffer J-C. Acute Myocardial Infarction in a 19 Year-Old Woman: Sometimes Hoofbeats are Zebras. Cardiovascular Medicine. 2011; 14(3):95. https://doi.org/10.4414/cvm.2011.01576
Chicago/Turabian StyleArroyo, Diego, Tobias Rutz, and Jean-Christophe Stauffer. 2011. "Acute Myocardial Infarction in a 19 Year-Old Woman: Sometimes Hoofbeats are Zebras" Cardiovascular Medicine 14, no. 3: 95. https://doi.org/10.4414/cvm.2011.01576
APA StyleArroyo, D., Rutz, T., & Stauffer, J.-C. (2011). Acute Myocardial Infarction in a 19 Year-Old Woman: Sometimes Hoofbeats are Zebras. Cardiovascular Medicine, 14(3), 95. https://doi.org/10.4414/cvm.2011.01576



