Typical Signs of Secundum Atrial Septal Defect in a Young Man
Abstract
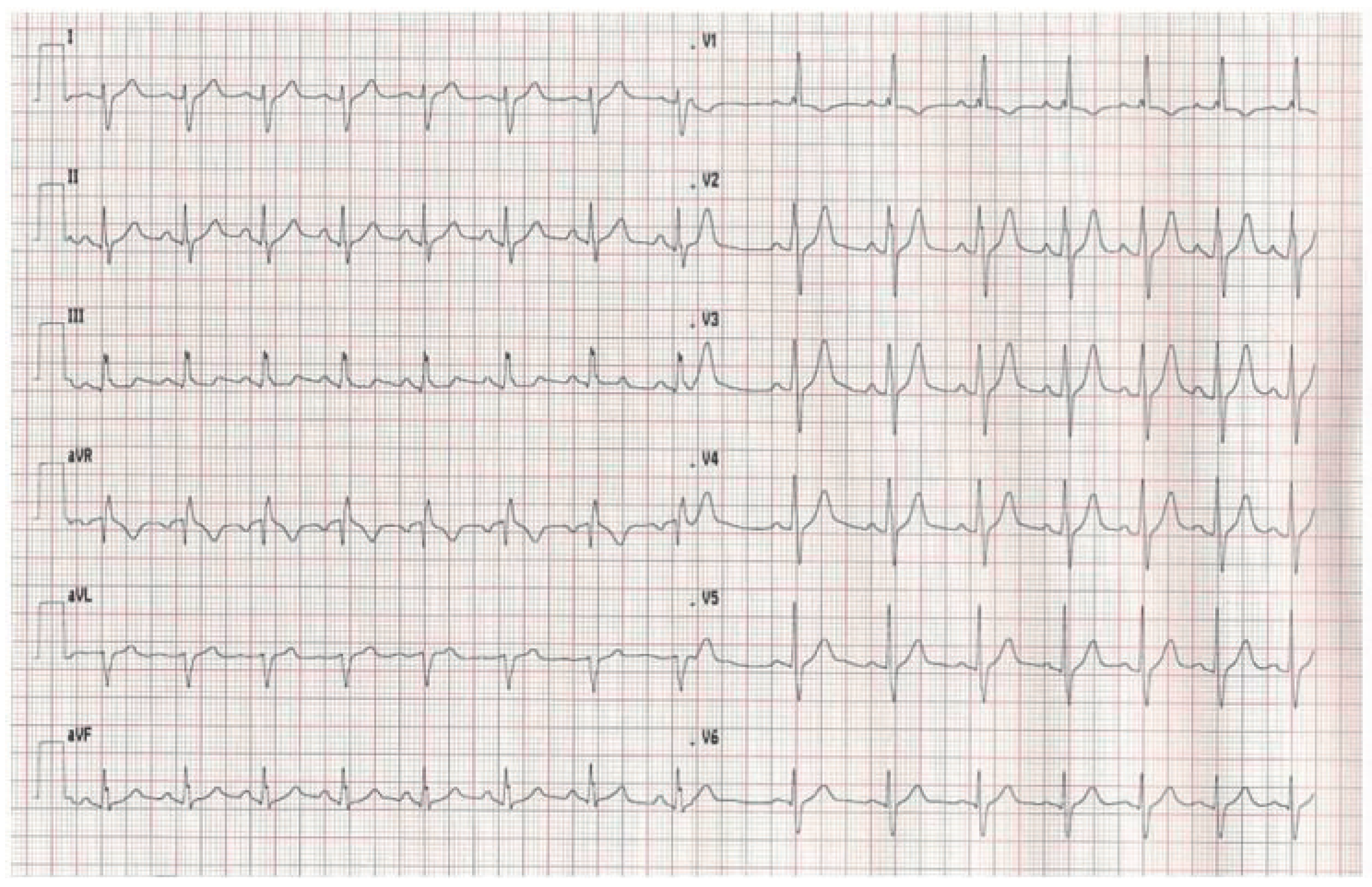
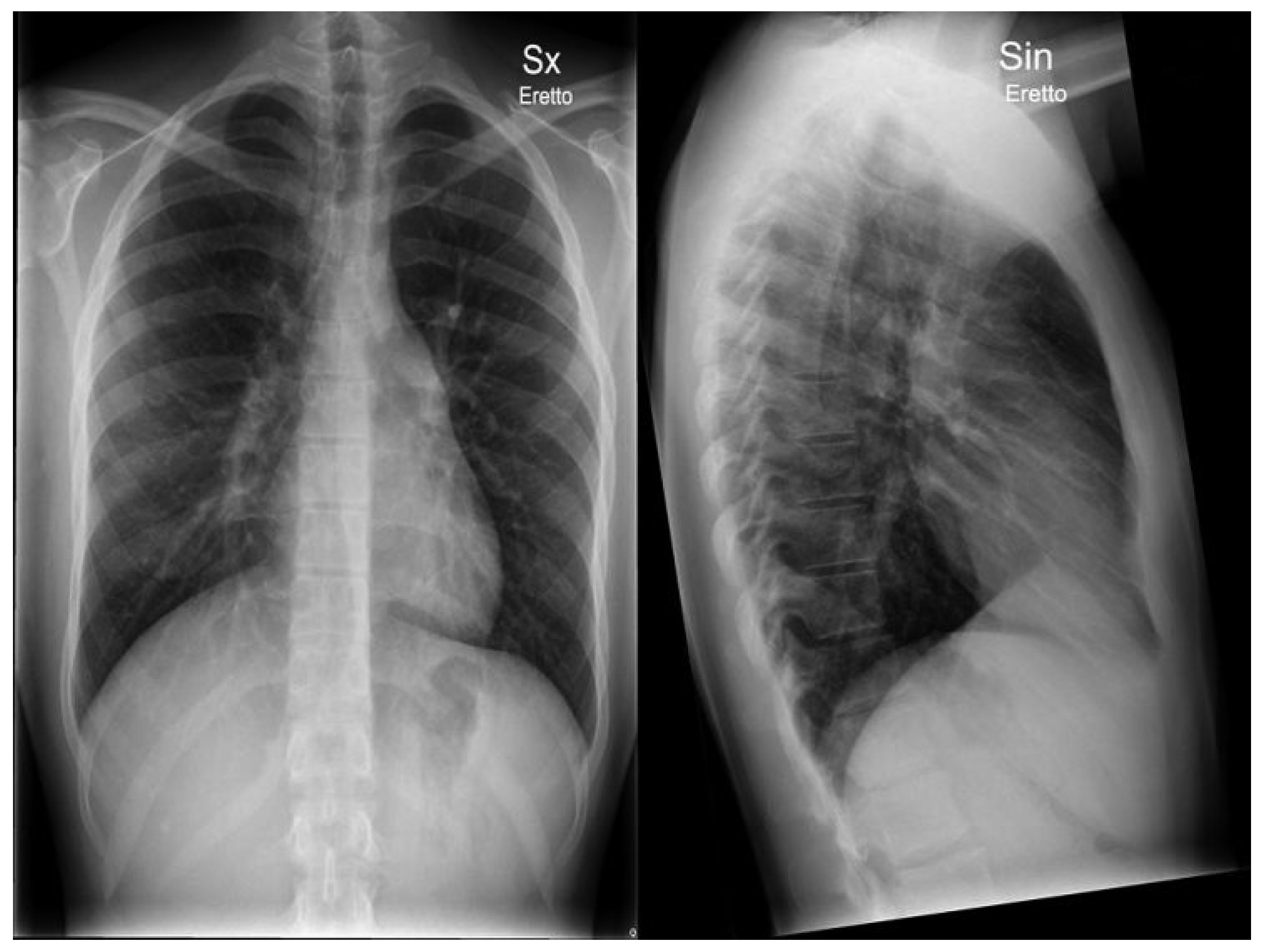
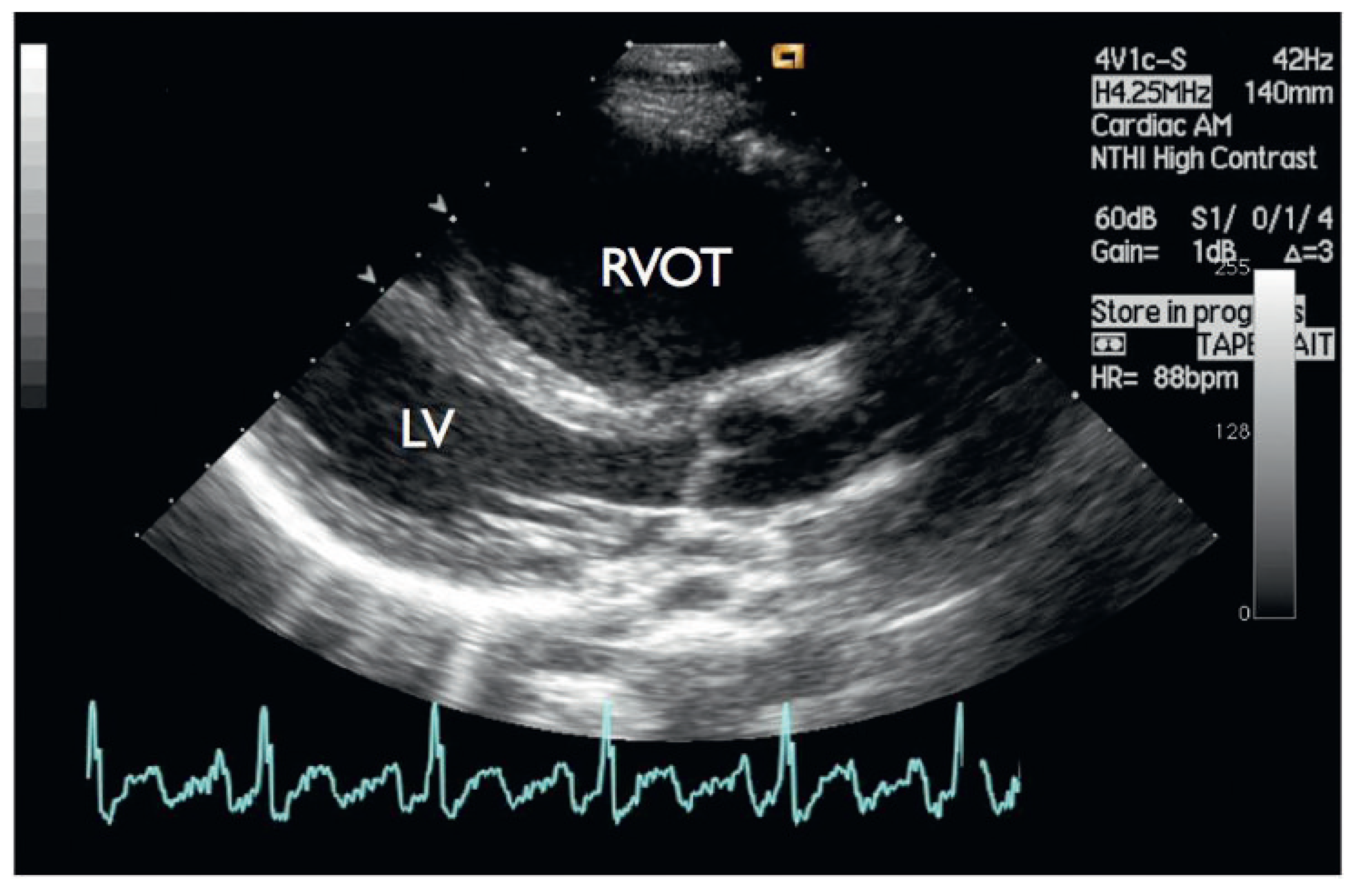
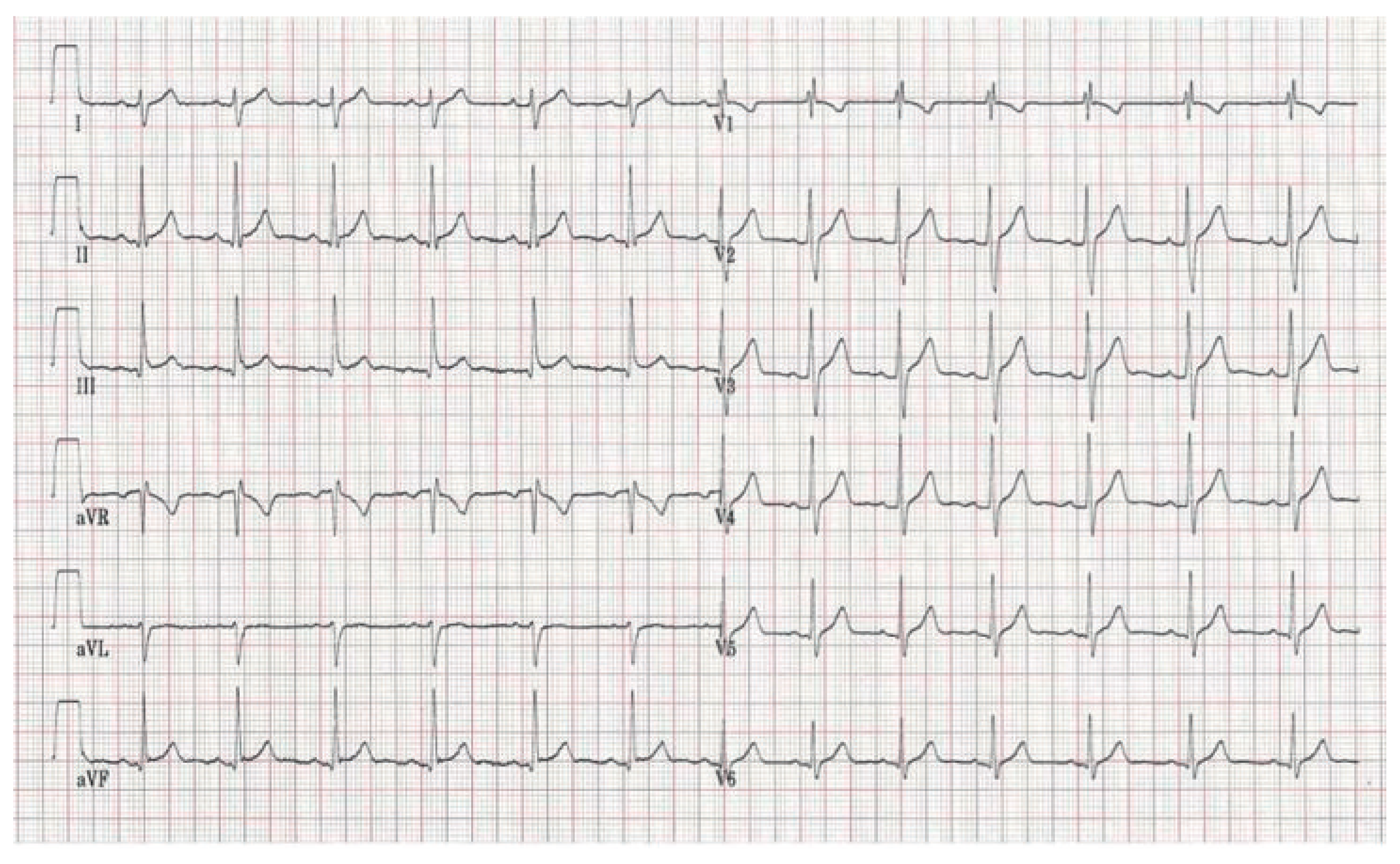
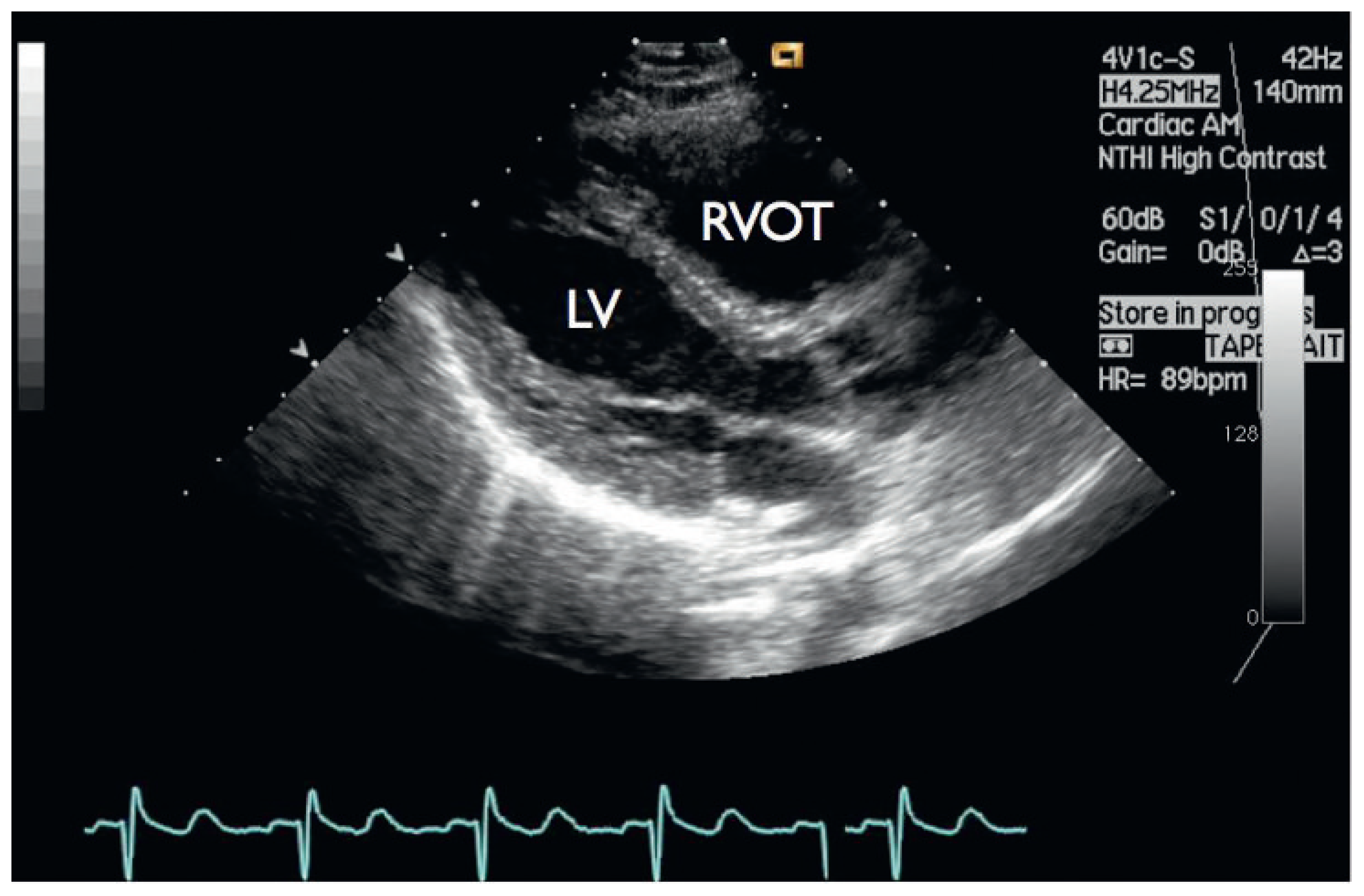
Case report
Discussion
Conflicts of Interest
References
- Webb, G.; Gatzoulis, M.A. Atrial septal defects in the adult recent progress and overview. Circulation. 2006, 114, 1645–1653. [Google Scholar] [CrossRef] [PubMed]
- Surawicz, B.; Knilans, T. Chou’s Electrocardiography in clinical practice, 6th ed.; Elsevier: Saunders, Philadelphia, 2008; pp. 672–674. [Google Scholar]
- Azhari, N.; Shihata, M.S.; Al-Fatani, A. Spontaneous closure of atrial septal defects within the oval fossa. Cardiol Young. 2004, 14, 148. [Google Scholar] [CrossRef] [PubMed]
- Nadrai, A. ECG in the diagnostics of atrial septal defect. Acta Paediatr Acad Sci Hung. 1964, 65, 201–215. [Google Scholar]
- Heller, J.; Hagège, A.A.; Besse, B.; Desnos, M.; Marie, F.N.; Guerot, C. “Crochetage” (Notch) on R Wave in inferior limb leads: a new independent electrocardiographic sign of atrial septal defect. J Am Coll Cardiol. 1996, 27, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Guray, U.; Guray, Y.; Mecit, B.; et al. Maximum p wave duration and p wave dispersion in adult patients with secundum atrial septal defect: the impact of surgical repair. Ann Noninvasive Electrocardiol. 2004, 9, 136. [Google Scholar] [CrossRef] [PubMed]
- Davia, J.E.; Cheitlin, M.D.; Bedynek, J.L. Sinus venosus atrial septal defect: analysis of fifty cases. Am Heart J. 1973, 85, 177. [Google Scholar] [CrossRef] [PubMed]
- Egeblad, H.; Berning, J.; Efsen, F.; Wennevold, A. Non-invasive diagnosis in clinically suspected atrial septal defect of secundum or sinus venosus type: value of combining chest x-ray, phonocardiography, and M-mode echocardiography. Br Heart J. 1980, 44, 317–321. [Google Scholar] [PubMed]
- Murphy, J.G.; Gersh, B.J.; McGoon, M.D.; Mair, D.D.; Porter, C.J.; Ilstrup, D.M.; et al. Long-term outcome after surgical repair of isolated atrial septal defect: follow-up at 27 to 32 years. N Engl J Med. 1990, 323, 1645–1650. [Google Scholar] [PubMed]
© 2011 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Valentino, M.D.; Gallino, A.; Klimusina, J.; Demertzis, S.; Menafoglio, A. Typical Signs of Secundum Atrial Septal Defect in a Young Man. Cardiovasc. Med. 2011, 14, 98. https://doi.org/10.4414/cvm.2011.01577
Valentino MD, Gallino A, Klimusina J, Demertzis S, Menafoglio A. Typical Signs of Secundum Atrial Septal Defect in a Young Man. Cardiovascular Medicine. 2011; 14(3):98. https://doi.org/10.4414/cvm.2011.01577
Chicago/Turabian StyleValentino, Marcello Di, Augusto Gallino, Julija Klimusina, Stephanos Demertzis, and Andrea Menafoglio. 2011. "Typical Signs of Secundum Atrial Septal Defect in a Young Man" Cardiovascular Medicine 14, no. 3: 98. https://doi.org/10.4414/cvm.2011.01577
APA StyleValentino, M. D., Gallino, A., Klimusina, J., Demertzis, S., & Menafoglio, A. (2011). Typical Signs of Secundum Atrial Septal Defect in a Young Man. Cardiovascular Medicine, 14(3), 98. https://doi.org/10.4414/cvm.2011.01577



