Case description
A 37-year-old man, with active smoking and dyslipidemia as cardiovascular risk factors, experienced acute onset chest pain and dyspnea while playing badminton. His game opponent called the paramedics. The physician dispatched with the ambulance performed a 12-lead electrocardiogram showing tombstone ST segment elevation in the anterior leads (
Figure 1A), and therefore activated the ST segment elevation myocardial infarction (STEMI) alarm in order to prepare the cardiac catheterisation laboratory at the primary percutaneous coronary intervention (PCI) centre. After administration of 250 mg intravenous (IV) aspirin, 600 mg loading dose of clopidogrel and 5000 IU of IV unfractionated heparin, the patient was brought directly to the cardiac catheterisation laboratory.
Shortly after the beginning of the procedure, the patient developed haemodynamic instability with hypotension and pulmonary oedema. Single injection of the left coronary artery, performed using a right femoral approach, showed a completely occluded left main stem (LMS) in its mid portion (
Figure 1B). The diagnostic catheter was then exchanged for a 6 French extra backup 4.0 guiding catheter and two 0.014 wires were advanced into the left anterior descending coronary artery (LAD) and first obtuse marginal (OM). This restored a TIMI II flow (
Figure 1C) and allowed appreciation of an isolated mid-LMS plaque rupture not involving the LMS bifurcation. Reperfusion was followed by a sustained ventricular tachycardia which spontaneously cardioverted. Abciximab bolus and perfusion were administered, and thrombo-aspiration was performed with a Diver Catheter (Invatec, Roncadelle, Italy) (
Figure 1D) followed by the implantation of a 3.5 × 23 mm drug-eluting stent (Xience Prime, Abbott vascular) and restoration of TIMI III flow (
Figure 1E). Stent implantation was limited to the body of the LMS, thus no kissing balloon inflation was performed at the distal bifurcation. The timing intervals between alarm to firstmedical-contact, first-medical-contact to door and door to stent were 9, 29 and 21 min, respectively. Therefore, there was only 50 min between firstmedical-contact to stent implantation and no more than 70 min between symptom onset and revascularisation.
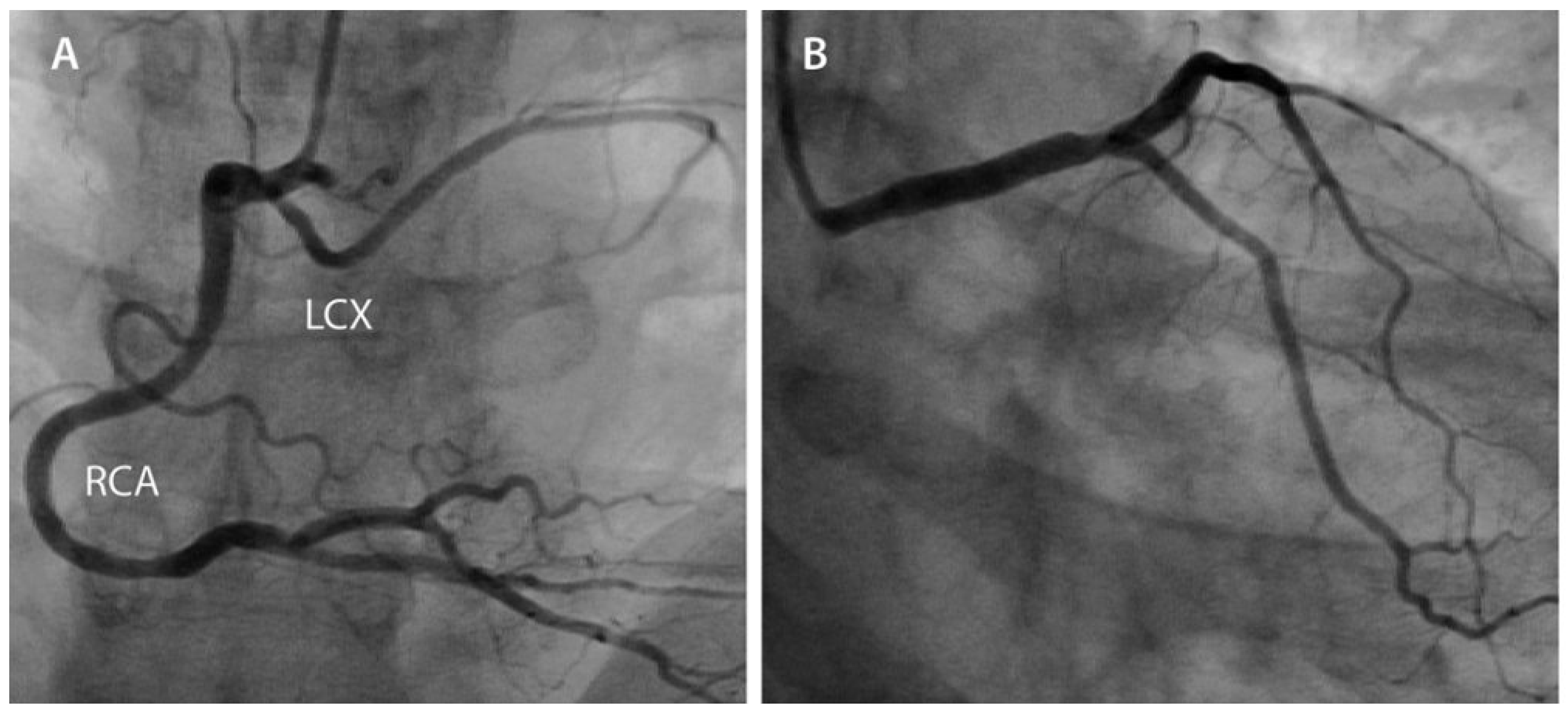
The right coronary artery (RCA) injection, performed thereafter, showed a normal dominant RCA with a partially aberrant left circumflex coronary artery (LCX), with the first OM arising from the left coronary tree (
Figure 2A). At the end of the primary PCI, an intra-aortic balloon pump (IABP) was inserted through the right femoral sheath and kept there for 48 h. The maximal creatine kinase and troponin values were 4800 U/l and 110 µg/L, respectively. Left ventricular ejection fraction (LVEF) was moderately decreased (35%) at transthoracic echocardiography (TTE).
The patient was transferred from the intensive care unit to the ward on day 4. He was then discharged home on day 9 on dual anti-platelet therapy (aspirin 100 mg and clopidogrel 150 mg for 15 days, followed by 75 mg daily for at least one year), metoprolol, linisopril, eplerenone and atorvastatin, and followed by an ambulatory cardiac rehabilitation programme for 6 weeks. Since the early platelet VASP phosphorylation assessment was above the target of 50% (68%), a 600 mg clopidogrel reload was administered with a second VASP assessment at 40%.
At 3 months, the LVEF was 40% on TTE assessment and the control coronary angiography at 9 months did not show any significant re-stenosis (
Figure 2B) in the LMS stent. Under 40 mg atorvastatin and lifestyle modification, LDL cholesterol decreased from 5.6 to 1.3 mmol/L, and at the one-year follow-up the patient was free of symptoms.
Discussion
We report the case of a young patient presenting with anterior STEMI and LMS occlusion with a favourable result following primary PCI. The prevalence of a culprit LMS lesion in patients undergoing primary PCI for STEMI is around 0.8–2.5%, and about 75% of the patients presenting with this condition are in cardiogenic shock [
1,
2,
3,
4,
5]. The rate of patients with a pre-procedure TIMI 0 flow varies between 40 and 79% according to published series on acute LMS disease [
1,
2,
3,
4]. In the pre-procedure TIMI 0 flow group, the 30-day mortality rate has been reported at around 60%, which is twice the rate described for patients with TIMI flow ≥ 1 at presentation [
1]. Multivariate analysis has shown that the absence or poor collateral angiographic circulation, sub-optimal post-procedural flow (TIMI flow < 3) and cardiogenic shock at presentation are independent predictors of mortality in patients with LMS stenosis and acute presentation [
1].
Although the partially aberrant LCX might have contributed to protect the patient, the short delay between symptom onset and revascularisation likely had a major impact on the favourable outcome of this patient who became haemodynamically unstable shortly after the beginning of the procedure. Specifically, the activation of the alarm system for STEMI from the field with direct transfer of the patient from the ambulance to the catheterisation laboratory markedly reduces the ischemic time. In our centre, the introduction of this alarm system led to a median reduction of 38 min of the door-to-balloon time and the proportion of patients treated within 90 min of hospital admission more than doubled [
6].
As the time interval between chest pain onset and first medical contact was less than 2 h in our case, according to the 2008 ESC STEMI guidelines [
7], thrombolysis could have been considered if the patient was not transferrable to a catheterisation laboratory in less than 90 min. Obviously, due to the extremely short transport distance (1.7 km), primary PCI was favoured.
Our usual practice is to cannulate both coronary arteries before starting recanalisation. This allows for adequate catheter French size and shape choice as well as the administration of anti-thrombotic drugs such as glycoprotein IIb/IIIa receptor inhibitor prior to wire passing. Since the culprit lesion involved the LMS, the RCA injection was performed only once the LMS was patent in order to reduce the time to reperfusion. Given the massive ST elevation involving the anterior lead, using a guiding catheter directly could have been an alternative option.
In our case, we favoured reperfusion over IABP insertion to avoid prolongation of the ischemic time by preparing a second vascular access and the IABP device. The latter was finally inserted at the end of the procedure in order to decrease cardiac workload. However, in this context, IABP insertion prior to recanalisation could have been an alternative strategy and in the case of refractory shock despite reperfusion and IABP insertion, a left ventricle assist device would have provided greater haemodynamic support.
In patients with acute coronary syndrome secondary to LMS lesion, if there is TIMI 3 flow grade and no cardiogenic shock, the time to revascularisation is less critical, and the decision between PCI versus coronary artery bypass graft surgery can be made based on the location and extension of the coronary artery disease, and the co-morbidities [
8].
Nowadays in the context of STEMI, prasugrel would be the preferred anti-platelet therapy in such a patient without contra-indications (age < 75 year old, weight > 60 kilos and no history of stroke). However, at the time of the procedure, and since prasugrel was not yet available in Switzerland, clopidogrel was prescribed and early platelet VASP phosphorylation assessment was performed.
Finally, when LMS is long as in our patient, anomalies of LCX origin should be suspected. It is a benign coronary anomaly described in 0.67% of coronary angiography [
9]. In the current case, the anomaly is likely to have protected the patient from refractory shock or ventricular fibrillation.
In conclusion, LMS thrombosis is a life-threatening disease, most often associated with cardiogenic shock. Primary PCI allows perfusion restoration and the potential to reverse arrhythmic and haemodynamic instability. The rapid percutaneous revascularisation in the presence of a dominant RCA and a partially aberrant LCX led to a favourable outcome in this 37-year-old patient.