Case report
We report the case of a 48-year-old female patient who presented with early-morning chest pain and dyspnoea and suffered a collapse at home. In a very agitated and convulsive state she was brought to the emergency room of a regional hospital where a cranial CT was performed which proved normal. After intravenous (i.v.) administration of midazolam, 3rd-degree AV-block followed by ventricular fibrillation was documented. Immediate cardiopulmonary resuscitation was performed and the patient was haemodynamically stabilised. Bedside transthoracic echocardiography showed anteroseptal wall motion abnormalities with poor left ventricular function (EF 35%). Acute coronary syndrome was diagnosed and therapy with clopidrogel, aspirin, betablocker, statin and heparin was started. Due to a recurrence of agitation and dyspnoea the patient had to be intubated and soon afterwards a short period of cardiopulmonary resuscitation was necessary again.
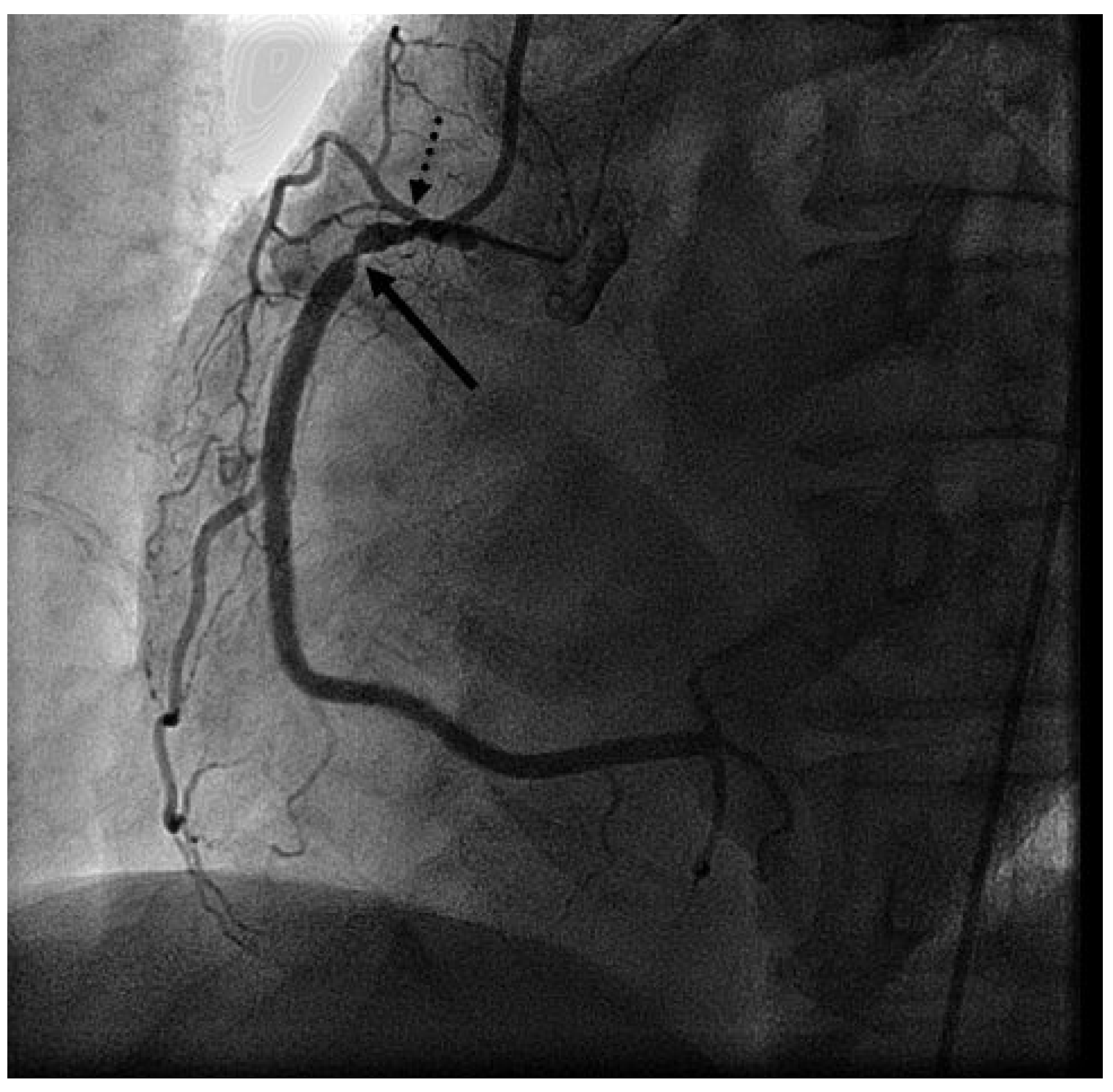
Presenting ECG changes (inferior ST-elevations) and rising cardiac enzymes, the patient was transferred to the acute care hospital and cath lab. Emergency coronary angiography showed severe stenotic lesions in the proximal right coronary artery (RCA) (
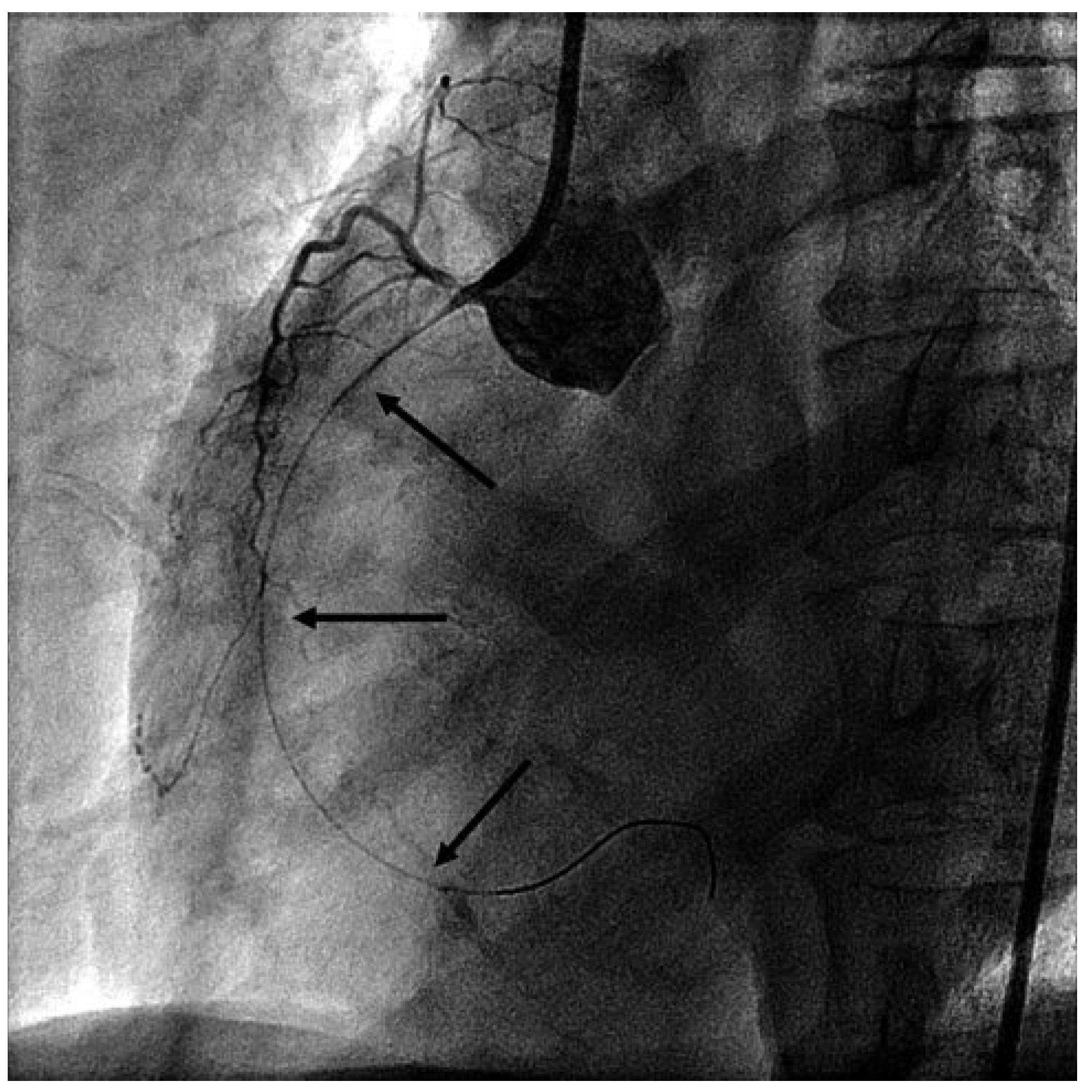
Figure 1), in the proximal left anterior descending artery and in the diagonal and marginal branches. Due to cardiogenic shock and inferior ECG changes, a percutaneous coronary intervention in the RCA was organised. After engaging the RCA with the guide catheter, total occlusion of the RCA was observed. The coronary wire was immediately placed in the distal RCA but this failed to restore the flow (
Figure 2).
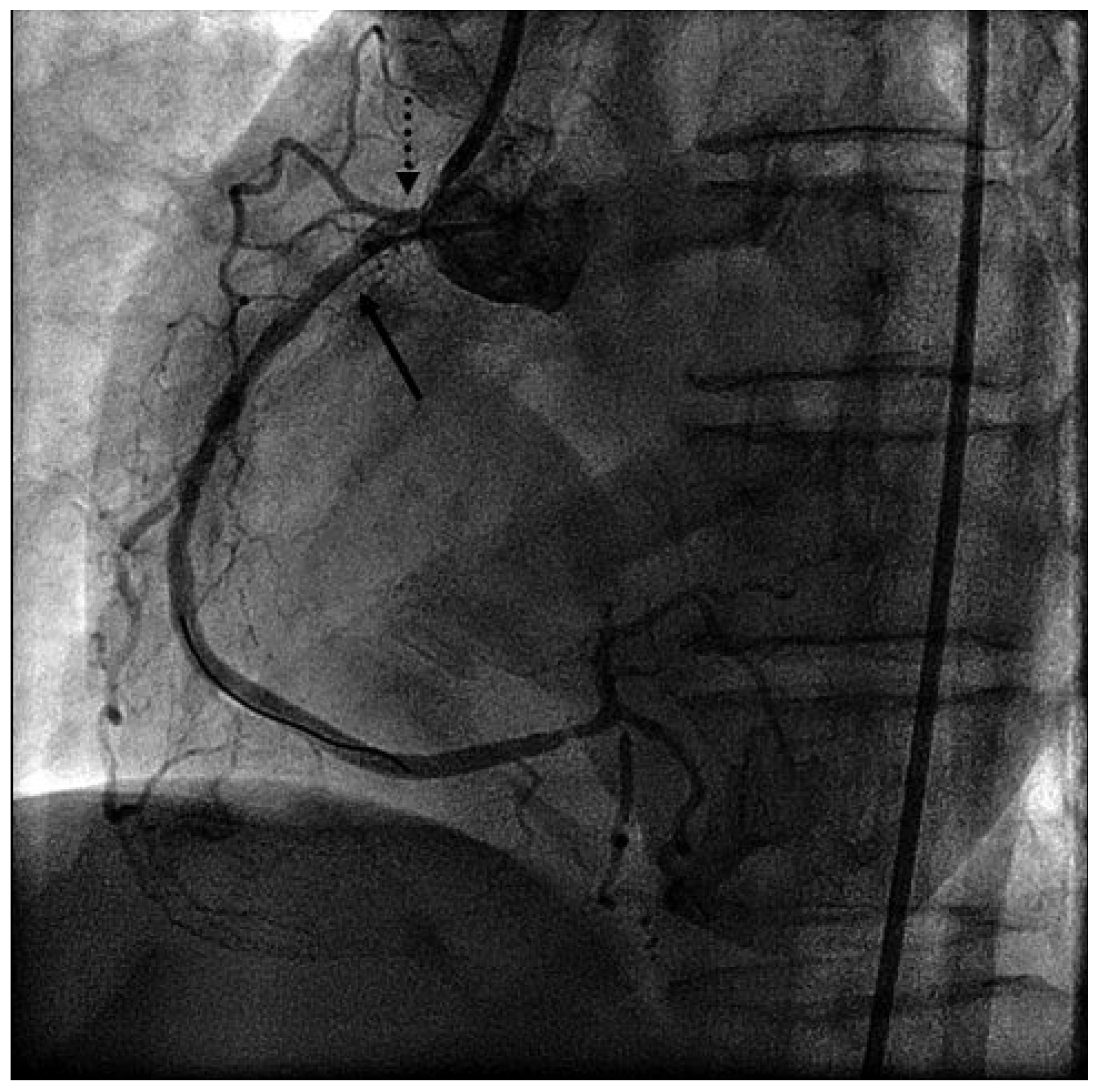
Due to further haemodynamic deterioration an intraaortic balloon pump was placed. At this point review of the angiogram led us to suspect spasmodic occlusion of the RCA due to guide catheter and wire irritation. Intracoronary nitroglycerin (NTG), adenosin and verapamil were administered. The wire was pulled as far as the mid-RCA, after which measures flow was restored in the RCA (
Figure 3) and the patient’s haemodynamic status stabilised. Reangiography of the left coronary artery showed resolution of the previously observed spasmodic lesions, and finally variant angina (prinzmetal angina) was diagnosed.
Continuous i.v. NTG was started and it was possible to extubate the patient next day. After reduction of the NTG dose the patient reported three episodes of retrosternal pain accompanied by either anterior STelevation and inferior ST-depression in the ECG, and the pain resolved after increasing the i.v. NTG dose again. The further history revealed that for at least a year the patient had experienced nightly episodes of retrosternal pain of increasing frequency and intensity.
Treatment with pantoprazole for mild gastrointestinal reflux disease brought no symptomatic relief, and she was therefore considered to have had a psychic disorder recently. Her personal history also revealed desensitised Widal syndrome and smoking. To wean her off NTG and prevent further coronary spasmodic episodes, medication with the long-acting calcium channel blockers nifedipine and diltiazem was started and the dosage increased to maximum. Under this therapy the patient remained asymptomatic and during the treadmill exercise test neither chest pain nor ECG changes were documented. Transthoracic echocardiography at discharge showed normal left ventricular function without wall motion abnormalities. At three months’ follow-up the patient was still asymptomatic.
Discussion
In 1959, Malcolm Prinzmetal reported on “variant angina” as an independent cardiac disorder, consistent with vasospastic coronary stenoses [
1]. The disease is about three times more frequent in Japanese subjects than in Caucasians. There is typical angina at rest, which is recurrent and cyclic in the first hours of the day [
2] associated with ST-segment elevation in the ECG. Variant angina may be associated with myocardial infarction and life-threatening cardiac arrhythmias including ventricular tachycardia and ventricular fibrillation. Variant angina can be correctly diagnosed in the light of spasms and ECG changes during coronary angiography (life-case demonstration or provocation test), which, along with the dramatic response to nitrates and calcium channel blockers, are strong indicators. Provocative tests include intracoronary administration of acetycholine (preferred in Asia) or ergonovine, which should be done carefully. Also, provocation by hyperventilation performed over six minutes in the early morning may help to detect coronary spasms, though it is less provocative than ergonovine. Less invasive methods are telemetry and ambulatory Holter-ECG, which may detect ST changes and arrhythmias during cardiac ischaemic episodes.
Pathomechanically, endothelial dysfunction and generalised hypersensitivity of the coronary arteries are thought to cause spasms. Calcium overload of smooth muscle cells appears to be the final common pathway, and mediators may be adrenergic and parasympathetic agonists.
Several medications including anaesthetics, analgesics and chemotherapies may induce coronary vasospasms, and alcohol withdrawal, nicotine consumption, oxidative stress or local mechanical irritation may trigger them. An allergic reaction (release of inflammatory mediators) may also trigger spasms, as described by Kounis in 1991 [
3].
Dihydropyridine calcium channel blockers (CCBs) are highly effective in suppressing vasospasms and are widely accepted as standard therapy [
4]. There are significantly fewer myocardial infarctions and cardiac deaths in patients treated with CCBs, but recurrence of symptoms caused by coronary spasms cannot always be completely suppressed. The incidence is 37% in the first year and increases during subsequent years [
5]. Additional treatment options are long-acting nitrates if symptoms are recurrent or CCB side effects occur. Nicorandil may be tried, though more data on its efficacy are awaited.
In this patient, we combined CCBs of the dihydropyridine and diltiazem type, and the symptoms have been suppressed completely so far. Diltiazem in particular produces coronary dilation but is a less potent peripheral vasodilator. The therapeutic effects, vasodilation, afterload reduction and decreased oxygen consumption, may be additive and more effective in treating the disease. Our patient also stopped smoking, which is a risk factor of variant angina (around 60% of the patients are smokers). Whenever the efficacy of medication is unclear, an ambulatory Holter-ECG may help to detect symptomatic episodes. Preventive coronary stenting or a bypass operation should not be done if there is no fixed obstructive lesion, since it may do serious harm. Quite often coronary spasms are multilocal, as shown in this patient (multivessel spasms); localisation may also be different at various times. Implantation of an ICD as secondary prevention of sudden cardiac death is an option in cases with sustained ventricular tachycardia, and might be recommended early if medical therapy is not highly effective.
Although a cardiac origin of chest pain in younger patients is rare, the syndrome of variant angina, which shows an obvious circadian pattern, should be kept in mind.