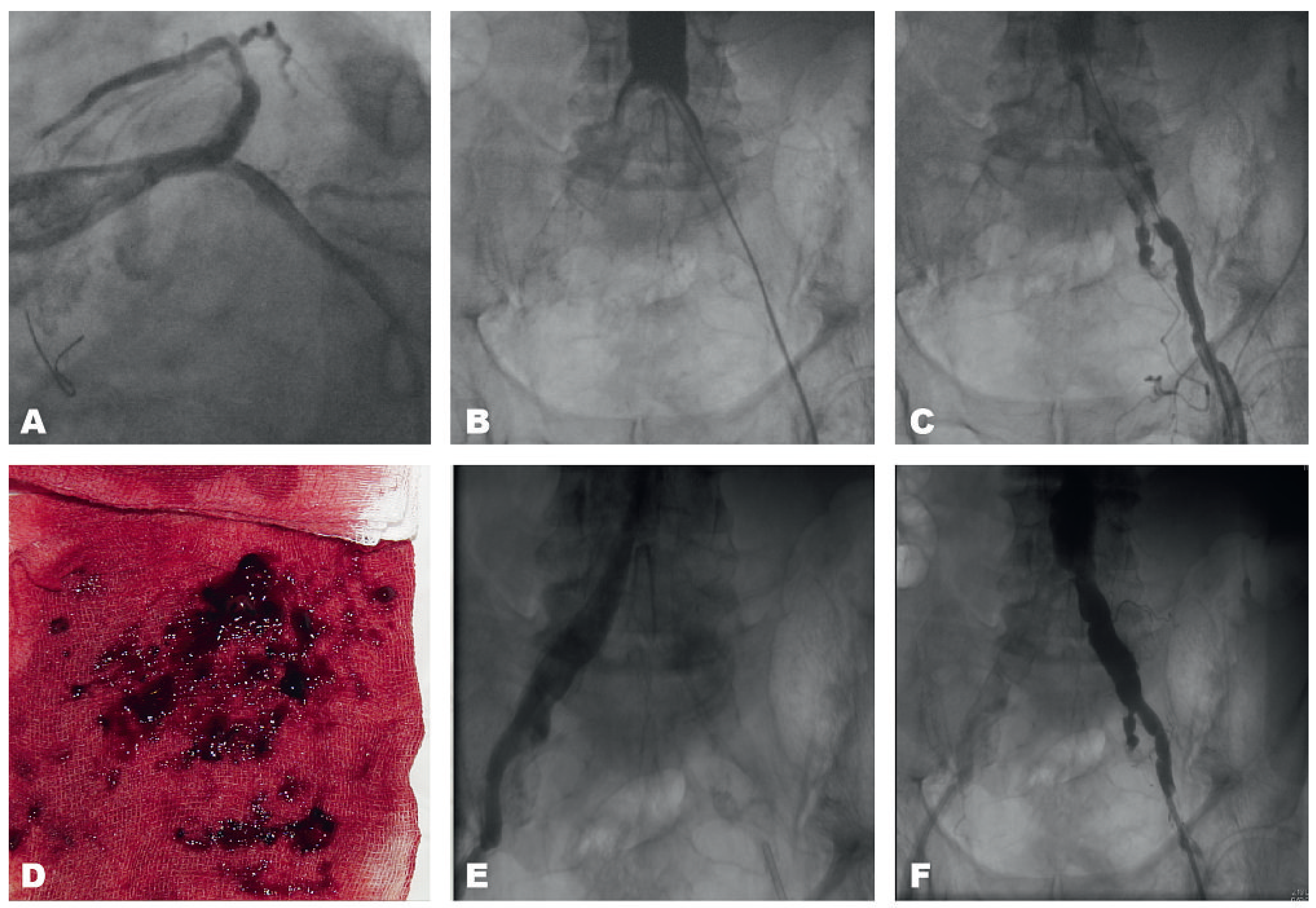
Acute Leriche Syndrome in an 83-Year-Old Man with Non NSTEMI After Cardiac Resuscitation Because of Ventricular Fibrillation
Case description
Comments
Conflicts of Interest
References
- Wiesenack, C.; Kerschbaum, G.; Keyser, A.; Kobuch, R.; Taeger, K. Acute Leriche’s syndrome in a patient undergoing coronary artery bypass grafting with extracorporeal circulation. Anaesthesist. 2001, 50(1), 32–36. [Google Scholar] [CrossRef] [PubMed]
- Dorland’s Illustrated Medical Dictionary 27th edition.
© 2010 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Sürder, D.; van den Berg, J.C.; Moccetti, T.; Pedrazzini, G.B. Acute Leriche Syndrome in an 83-Year-Old Man with Non NSTEMI After Cardiac Resuscitation Because of Ventricular Fibrillation. Cardiovasc. Med. 2010, 13, 292. https://doi.org/10.4414/cvm.2010.01521
Sürder D, van den Berg JC, Moccetti T, Pedrazzini GB. Acute Leriche Syndrome in an 83-Year-Old Man with Non NSTEMI After Cardiac Resuscitation Because of Ventricular Fibrillation. Cardiovascular Medicine. 2010; 13(9):292. https://doi.org/10.4414/cvm.2010.01521
Chicago/Turabian StyleSürder, Daniel, Jos C. van den Berg, Tiziano Moccetti, and Giovanni B. Pedrazzini. 2010. "Acute Leriche Syndrome in an 83-Year-Old Man with Non NSTEMI After Cardiac Resuscitation Because of Ventricular Fibrillation" Cardiovascular Medicine 13, no. 9: 292. https://doi.org/10.4414/cvm.2010.01521
APA StyleSürder, D., van den Berg, J. C., Moccetti, T., & Pedrazzini, G. B. (2010). Acute Leriche Syndrome in an 83-Year-Old Man with Non NSTEMI After Cardiac Resuscitation Because of Ventricular Fibrillation. Cardiovascular Medicine, 13(9), 292. https://doi.org/10.4414/cvm.2010.01521



