Case Report
The patient with severe degenerative stenosis of a tricuspid aortic valve complained of exertional chest pain and occasional dizziness but no loss of consciousness. Severe aortic stenosis had been diagnosed due to a murmur observed during the occasion of a hospitalisation for a skiing accident eight months earlier. Past medical history was remarkable for persistant atrial fibrillation and hypertension. The electrocardiogram showed atrial fibrillation at a rate of 96 bpm with no evidence of bundle branch block. Transthoracic echocardiography revealed a mean/peak gradient of 47/67 mm Hg projecting an aortic valve area of 0.5 cm2, according to the continuity equation. Left ventricular function was normal and there was no pulmonary hypertension. Exercise treadmill testing showed a mildly decreased exercise tolerance, reproduced the reported symptoms, and showed ST-deviations without an exercise-induced drop of systolic blood pressure. The patient refused to undergo open heart surgery and was reluctant to continue oral anticoagulation for atrial fibrillation. He agreed to cardiac catheterisation with percutaneous cardiac intervention.
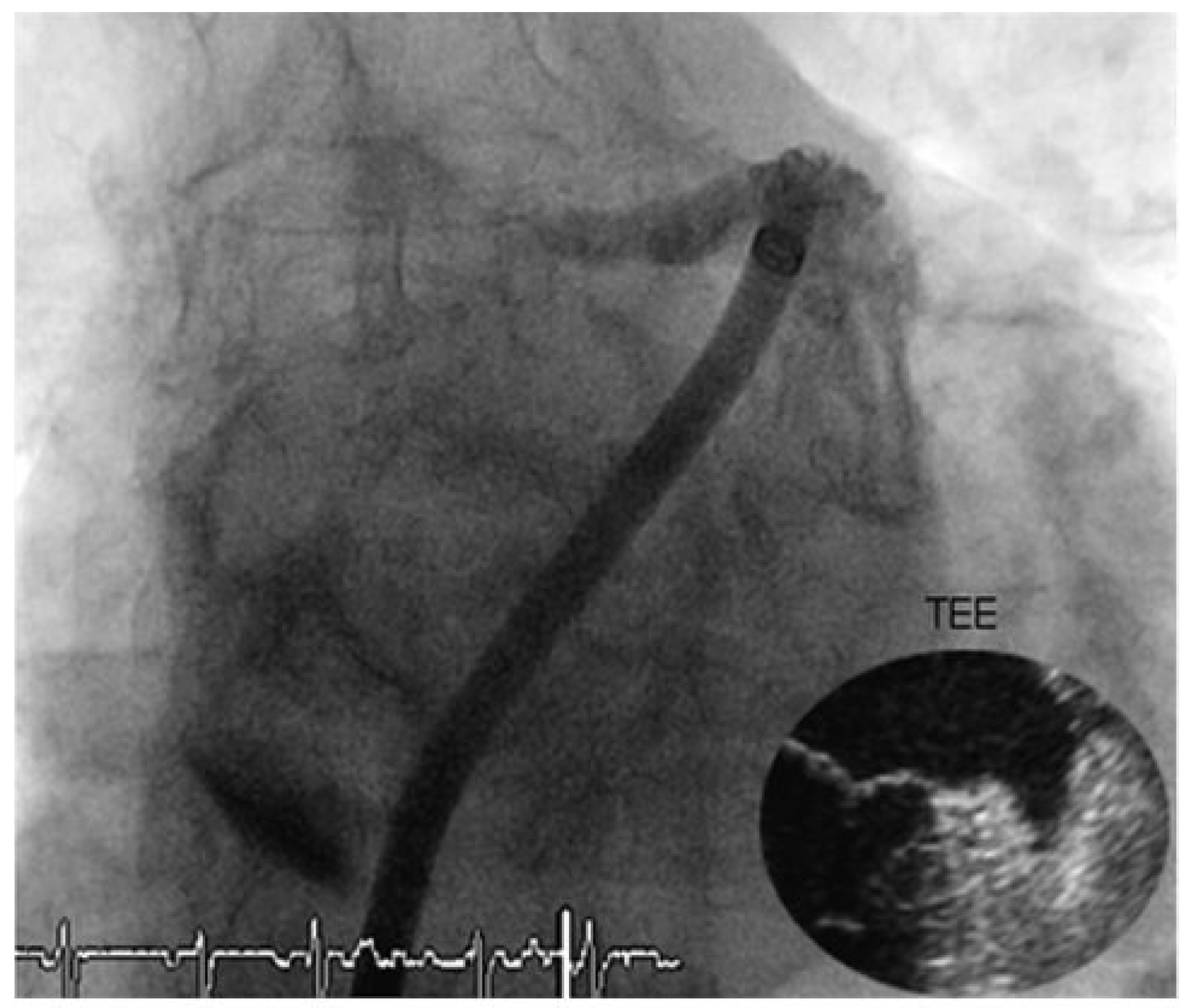
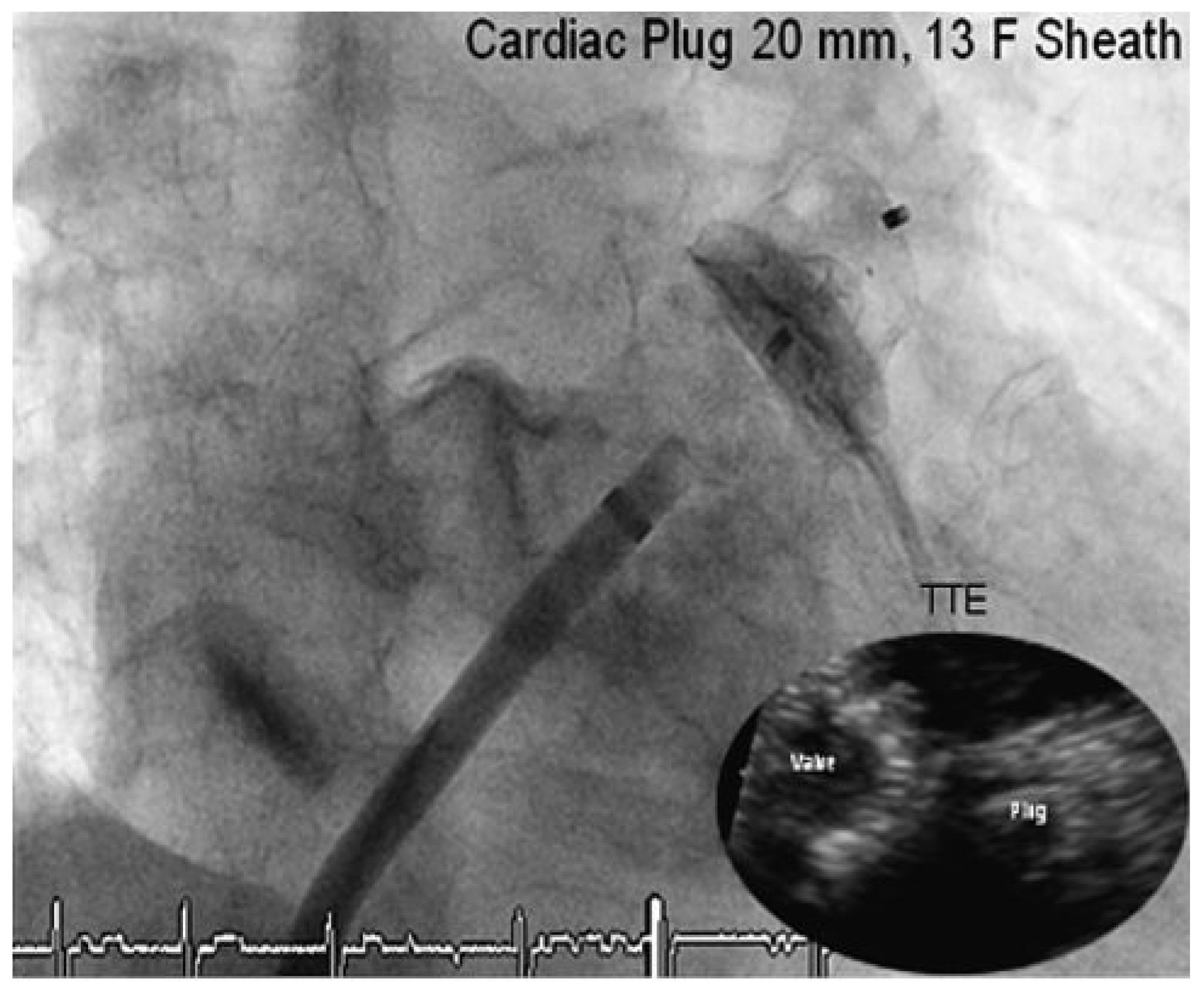
Through a transfemoral venous approach and transseptal puncture, the left atrial appendage was identified and an Amplatzer cardiac Plug 20 mm was positioned in the entry of the appendage. A stable position of the device and complete occlusion of the retroverted, single-lobulated appendage were verified by angiography before the device was released from the catheter (
Figure 1 and
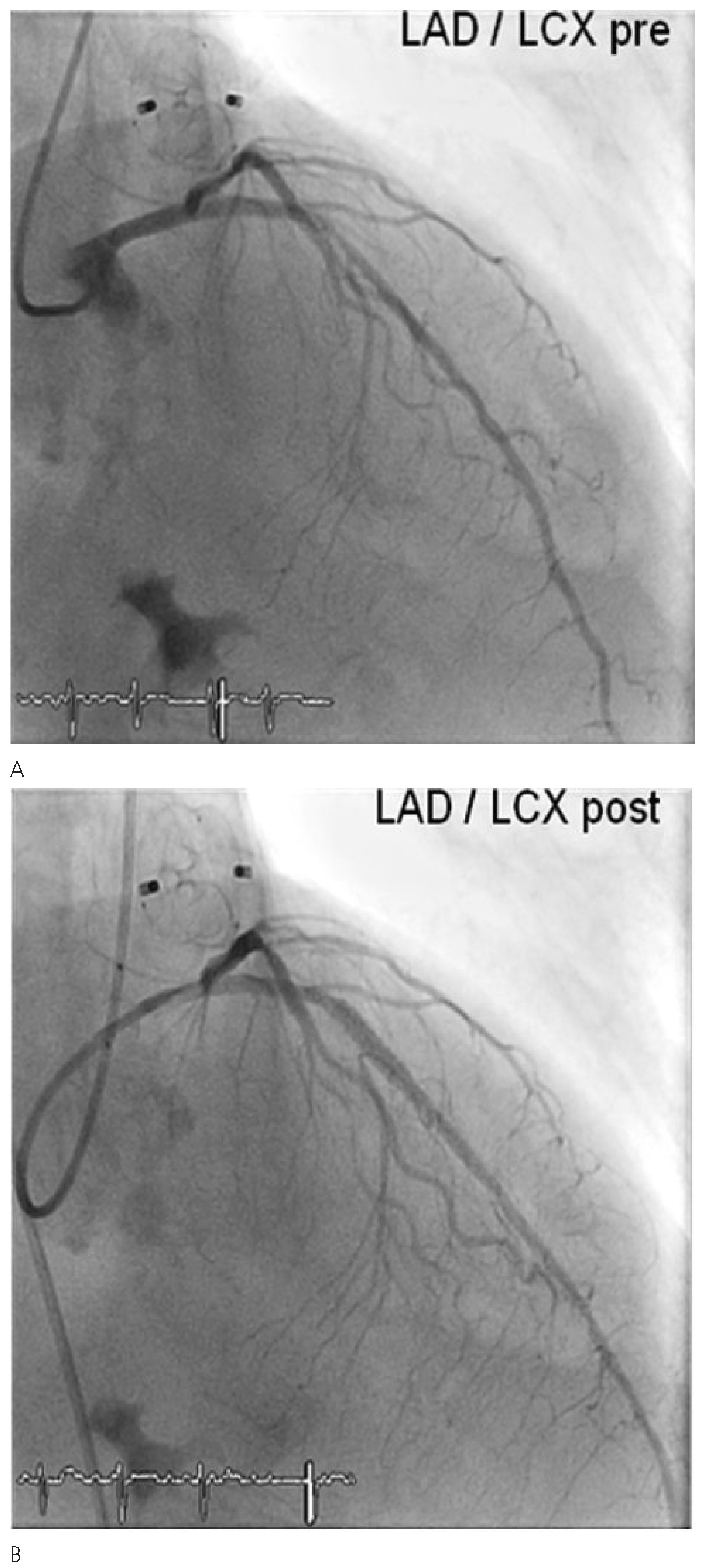
Figure 2). Thereafter, coronary angiography was performed which showed significant stenosis of the mid left anterior descending coronary artery (LAD) and the proximal left circumflex coronary artery (LCX). Following successful treatment with two everolimus-eluting stents, respectively (
Figure 3), angiography of the aorta and iliac artery was performed to measure the aortic valvar annulus and assess the peripheral access site. The patient qualified for implantation of a Medtronic CoreValve bioprosthesis and a 18 French sheath was introduced in the right femoral artery, as well as a temporary transvenous pacemaker through a right jugular access. After balloon dilatation of the degenerative aortic valve with a Nucleus balloon 25 × 40 mm under rapid pacing, the self-expandable bioprosthesis was deployed under fluoroscopic guidance (
Figure 4). Periinterventional transoesophageal echocardiography demonstrated an excellent result with negligible paravalvular regurgitation. Simultaneous invasive measurement demonstrated a decrease in the mean transvalvular pressure gradient from 56 to 5 mm Hg. Closure of the right femoral access site was performed under temporary balloon occlusion of the right external iliac artery, from a contralateral femoral access with a Prostar device. The intervention was performed under general anaesthesia.
The further hospital course was uneventful. Postinterventional transthoracic echocardiography confirmed the excellent periinterventional result and the patient was discharged home on the fourth postinterventional day, on double antiplatelet therapy with acetylsalicylic acid (100 mg per day) and Clopidogrel (75 mg per day).
Discussion
Percutaneous treatment strategies shorten hospitalisation duration, accelerate time to recovery and enhance patient comfort. They have proven to be a valuable alternative to open heart surgery in an ever growing field of cardiac interventions. Coronary artery disease and atrial fibrillation are common findings in elderly patients with severe aortic stenosis and are associated with an adverse prognosis [
1]. Comprehensive management in high-risk patients with aortic stenosis and coronary artery disease has been suggested using a hybrid approach with a staged procedure involving initial percutaneous coronary intervention (PCI) followed by valve replacement shortly thereafter [
2]. Recently, a combined approach using PCI and transcatheter aortic valve implantation has been proposed for patients with complex coronary artery disease and aortic valve stenosis in a small subset of patients [
3]. In our own experience of more than 160 patients undergoing transcatheter aortic valve implantation at our facility, 13% underwent concomitant PCI and 12% were treated in a staged procedure, both with favorable midterm results.
Atrial fibrillation increases the risk for embolic stroke with emboli mostly originating from the left atrial appendage. Whereas anticoagulation has proven to be effective in the prevention of thromboembolic events, it is associated with the hazard of severe bleeding [
4], particularly in elderly patients. Percutaneous closure of the left atrial appendage has been demonstrated to be not inferior to warfarin therapy in a recent multicentre, randomised trial [
5]. The technique used here was derived from the well established closure technique for atrial shunts [
6].
This is, to our knowledge, the first case of a concomitant PCI, transfemoral aortic valve implantation and left atrial appendage closure in a single intervention and demonstrates the feasibility of a combination of different techniques during a single intervention in appropriate patients. Even though such a combined intervention is not in accordance with current guidelines and hence cannot be recommended as a routine approach at this time, it is anticipated to be the next step in percutaneous cardiac treatment.