Abstract
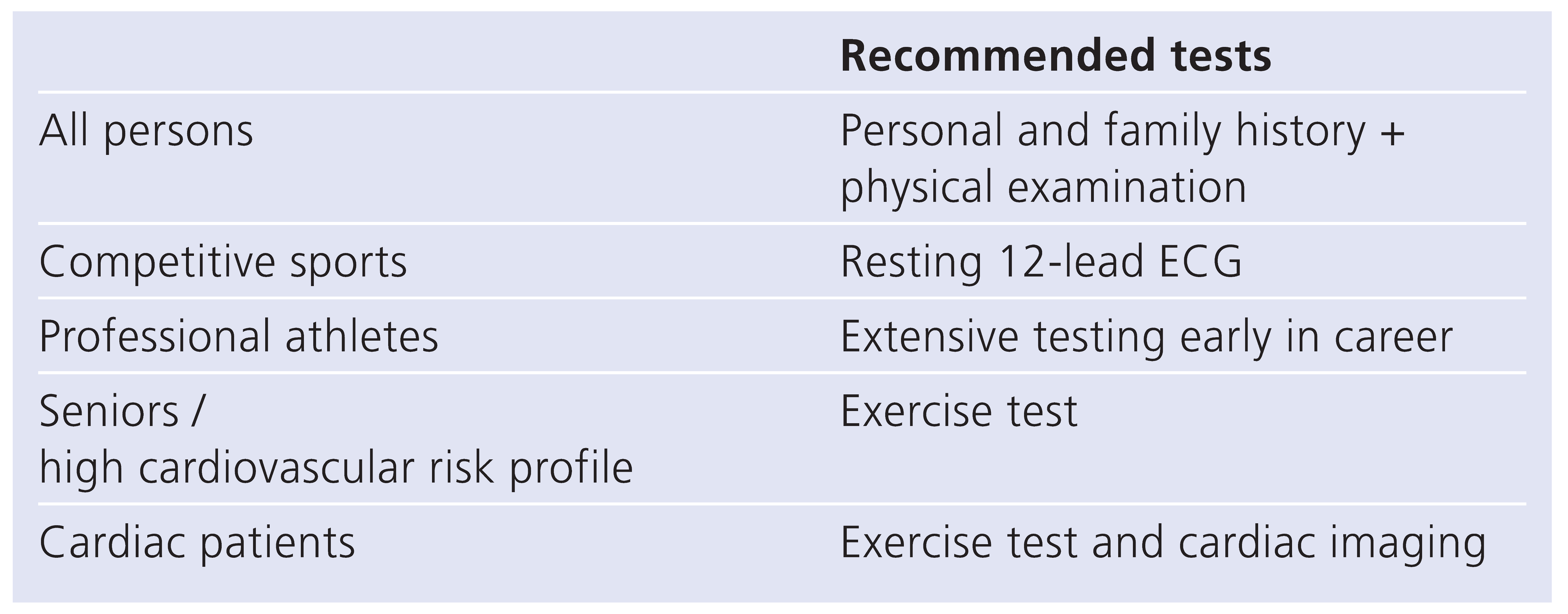
Physical activity protects against premature manifestations of many degenerative and especially cardiovascular diseases. On the other hand there is a slightly increased risk of cardiac death during activity, predominantly in untrained persons but also in previously healthy and well trained athletes. Since cardiologists advocate sports and physical activity they are called upon to recommend appropriate screening procedures to avoid some of these risks. Based on broad knowledge about the pathophysiology of sports related deaths a number of effective screening methods can be recommended which should be applied to individuals according to their level of activity and possible risk factors. We specifically recommend a thorough personal and family history on any person before taking up strenuous activity, searching for exercise related symptoms and cardiovascular risk factors as well as for cases of genetic heart disease or sudden death in families. Second a physical examination with blood pressure measurement and chest auscultation are mandatory to detect congenital abnormalities (outflow obstruction of the left ventricle such as aortic stenosis, hypertrophic cardiomyopathy, coarctation). Before engaging in competitive sports a resting 12-lead ECG is recommended to detect signs of cardiomyopathy or primary electrical disease. Any abnormal finding should be followed by detailed evaluation before clearing the athlete. For professional elite athletes it may be advisable to undertake a more detailed testing at the outset of a career involving high financial stakes in order to avoid economic consequences of later disqualification.
Exercise and health
During the last 60 years a broad knowledge has accumulated as to the health promoting effect of regular physical activity [1]. Exercise has beneficial effects not only on the cardiovascular system but also on other major organ systems and has been found to be protective for a variety of diseases. As a consequence sports activities have gained widespread acceptance in our society. Physical fitness is advocated not only by the medical profession but also by political authorities based on evidence-based scientific recommendations [2,3,4] (Figure 1). For the official recommendations by the Swiss government and health authority see website www.hepa.ch
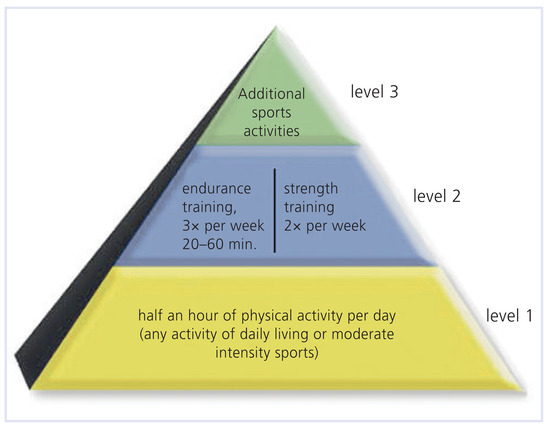
Figure 1.
The “pyramid of movement” as proposed by the BASPO (Swiss governmental agency of sports). (With kind permission to reprint from BASPO, http://www.sport.admin.ch/hepa/downloads/ Bewegung_pyramide_de.pdf, copyright © 2009.).
Sudden cardiac death occurring during sports is a rare but tragic event [5]. It is usually given great public attention especially when it occurs during competitions or games. These facts have led to a concept called “sports paradoxon” a term used to summarise that although exercise promotes health it can also provoke death. These two facts however do not necessarily contradict each other, as the preventive benefit refers to the population at large, whereas the momentary risk of a complication during activity—although present in any individual—varies greatly according to the level of training or habitual activity and does never outweigh the benefit mentioned in the first place [6,7].
The cardiologists’ role
It is easily conceivable that not every heart is apt to any amount of physical challenges. The risk of sudden cardiac death (SCD) during exercise not only strongly depends on the presence of a known or hidden disease or malformation, but also on the type of activity performed. Daily low-level exercise like walking or cycling is not the same as high level competition when extreme dynamic and or isometric physical exertion may be associated with considerable mental stress. In healthy populations the annual incidence of SCD is estimated to be up to 1 in 50,000 competition-hours or 1 in 200,000 organised sports participants [8], whereas among patients in cardiac rehabilitation a rate of 1.3 cardiac arrests in one million patient-exercise-hours has been reported [9]. Numerous studies have been conducted to clarify the causes or circumstances responsible for SCD during exercise [5,10,11,12].
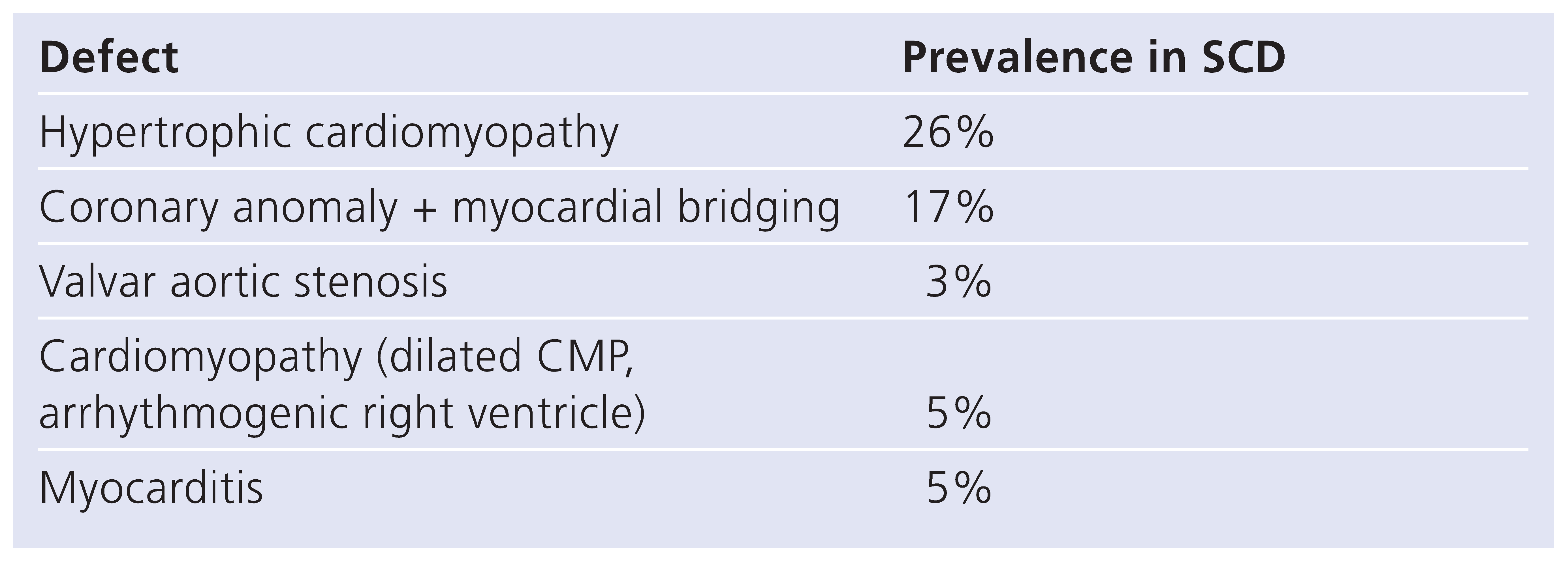
These can be placed into three main categories (Table 1):

Table 1.
Common congenital cardiac malformations associated with sudden death in athletes (according to [10]).
- In the truly healthy there is a rare condition called commotio cordis which can cause SCD by a blunt blow to the chest mechanically triggering ventricular fibrillation (VF).
- In people older than 35 years SCD generally is due to coronary artery disease, either known or unknown.
- In persons younger than 35 the cause of SCD most often is an underlying congenital defect.
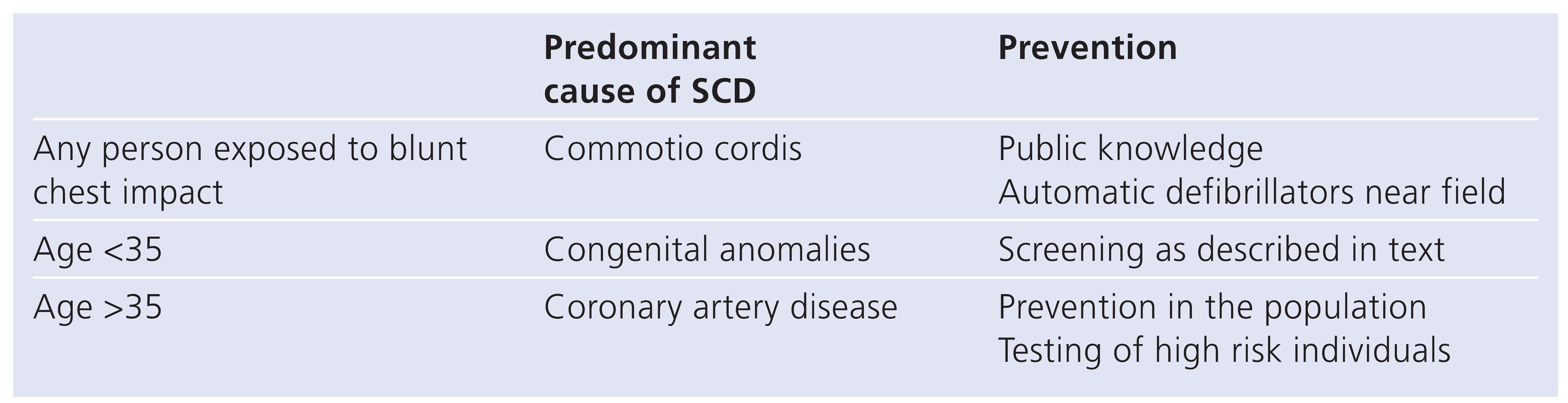
Considering these three major mechanisms, it is possible to envisage the most effective strategies for prevention as outlined in Table 2 and illustrated in Figure 2:

Table 2.
Causes of sudden death during exercise and prevention strategies.
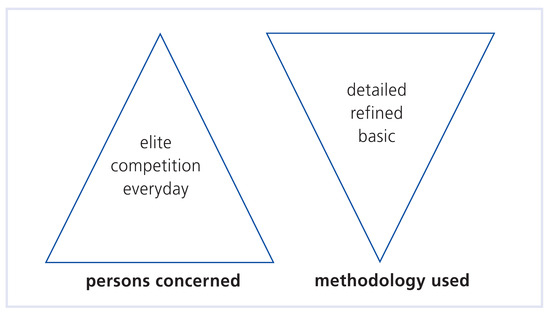
Figure 2.
Screening philosophy depicting the scope of testing according to the type of persons concerned.
- To prevent death from mechanical impact causing VF, this condition albeit rare has to bee known to trainers and supporters. In addition automatic defibrillators should be available in arenas where hockey and ball games are held.
- In order to lower the risk of deaths from coronary heart disease every effort should be made to inform the public about the risk factors for atherosclerosis, its manifestations and the early signs of coronary disease. Individuals with a high risk profile should undergo more in depth testing.
- Lastly, screening for hidden cardiac diseases should be considered in well-defined circumstances, taking into account the potential to detect relevant disease at a reasonable cost and without creating too many false positive findings.
When asked to counsel on physical activity cardiologists should refer to published recommendations but at the same time make specific prescriptions to healthy individuals as well as to cardiac patients [3,4,8,13,14]. It is assumed that cardiologists should rule out most of the known potential risks which means that they also must not overlook extracardiac domains [15,16].
The meaning of screening
Screening implies that effective test methods as well as treatments influencing outcome are at hand, which is true for most of the cardiac problems.
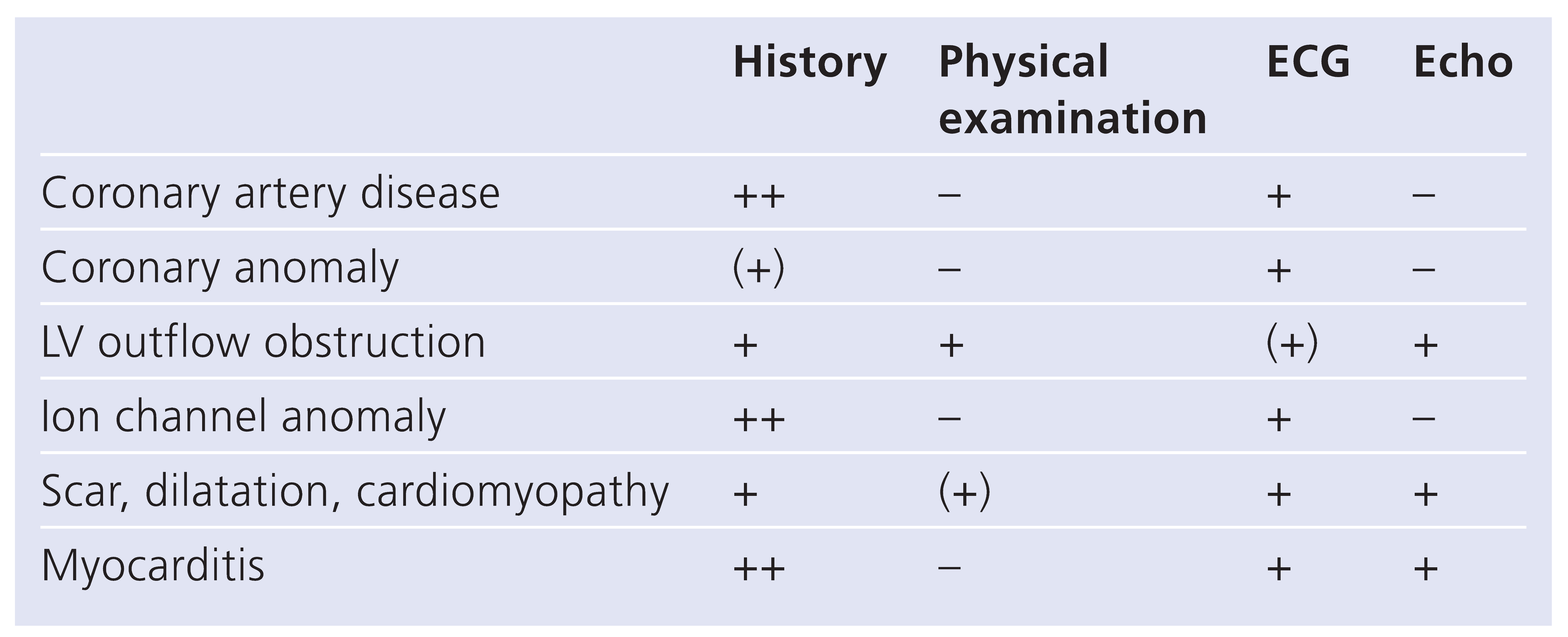
Table 3 shows the relative value of various investigations regarding the main anomalies and pathologies with a risk for SCD during exercise.

Table 3.
Potential value of investigations to detect anomalies predisposing to sudden cardiac death during exercise.
From this overview it is very obvious that a careful history is of key importance. This should elucidate a personal history of any symptoms (chest pain, shortness of breath, malaise, dizziness, syncope) occurring during exercise as well as any personal cardiovascular risk factors such as hypertension, smoking, hyperlipidaemia. The family history of SCD or cases of cardiomyopathies and of any premature manifestation of atherosclerotic disease is also of great importance. Physical examination complemented in doubtful cases by echocardiography can help to detect LVOT obstruction by valvular or subvalvular aortic stenosis and to rule out other major valve disease. It should also be used to evaluate patients with suspected or known heart failure.
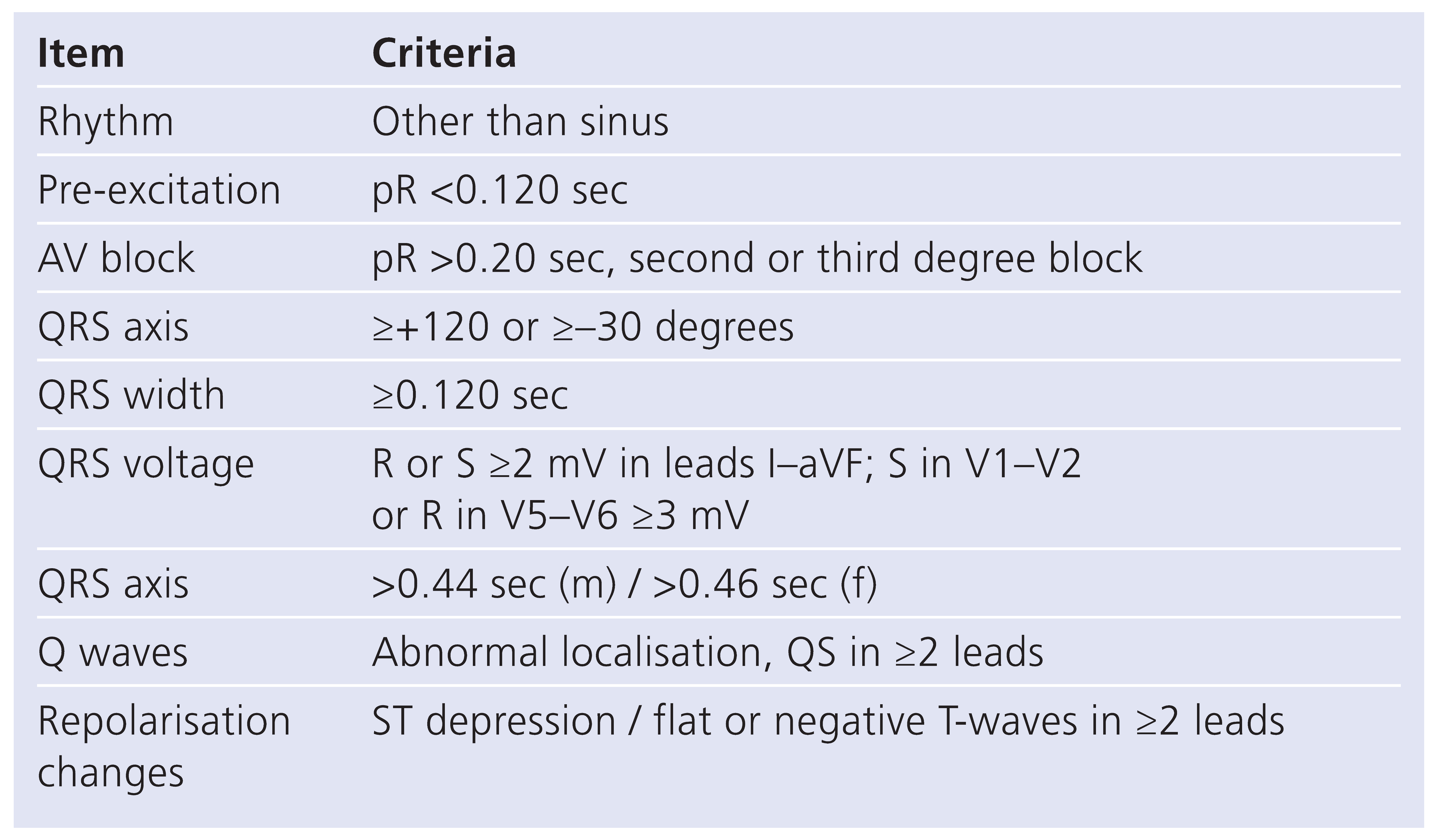
An electrocardiogram may show anomalies in almost any of the circumstances confering a risk for SCD during exercise, when analysed carefully according to the criteria listed in Table 4 [17,18]. The prevalence of ECG anomalies in unselected populations of athletes has been reported by several groups to be around 10% [18]. The majority (about 80%) of the anomalies are minor (sinus bradycardia, first degree AV-block, incomplete RBBB, early repolarisation, high QRS-voltage). These findings, when isolated, need no further evaluation, as they are commonly (99%) not associated with structural heart disease [19]. All other anomalies need further testing.

Table 4.
Criteria for ECG screening before engaging in sports (according to [17,18]).
In athletic populations screened by this clinical and ECG testing strategy the incidence of SCD dropped even slightly below the level of the general population [19,20] (Figure 3).
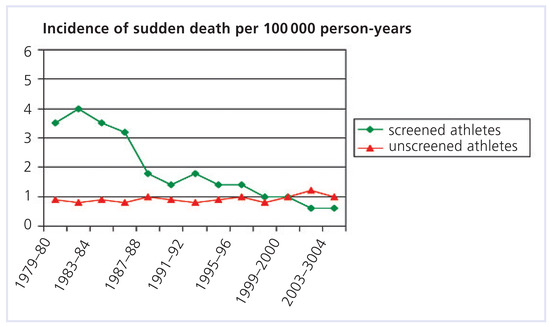
Figure 3.
Incidence of sudden cardiac death during sports in screened athletes and unscreened population. Screening was introduced in the early 1980s (adapted from [20]).
The screening philosophy should also take into account two aspects: the number of persons concerned and the methodology used. Their relative connection is illustrated in Figure 2. Methods can be kept simple when everyday physical activities in large populations are concerned but should to be more refined in professional top-elite athletes exposed to extreme forms of physical and emotional stress. In these cases a selective screening should preferably be performed at the start of a career before financial stakes may be compromised by medical recommendations or disqualification.
Specific tests
Exercise tests are not generally recommended for basic levels of activity as there is broad consensus about the very low diagnostic yield of this test in healthy individuals [21]. Exercise testing is however very useful in cases of known heart disease to elicit physical capacity, signs of ischaemia, conduction disturbances or arrhythmias and to study the course of blood pressure and heart rate allowing the detailed prescription of exercise based upon these data [2,14].
Echocardiography is extremely helpful in any cases of suspected structural heart disease or anomaly, especially for further evaluation of abnormal physical or ECG findings.
Other tests such as electrophysiological studies, MR, CT or nuclear imaging and coronary angiography may be needed according to clinical indications in specific cases.
A summary of recommendations about the use of various screening methods in predefined populations is shown in Table 5 [2,4,13,15,22]. For recommendations adapted to the Swiss health care system see also website www.sakr.ch.

Table 5.
Recommended screening in various subgroups before engaging in sports.
Effectiveness of screening programs
Whereas based on a recent meta analysis [23] the value of physical examination as a sreening test has been questioned, the incidence of SCD in athletes has been shown to be dramatically reduced after the introduction of legislation for ECG screening in Italy [20]. Critics argue that this merely represents a shift of cases from the athletic into the general population where these few cases do not alter statistics. Screening perhaps does not lead to a real reduction of SCD, but at least they do not occur during sports any more. A word of caution is also appropriate as to the negative effects on people’s life when false positive findings entail a host of further investigations or when they are given diagnoses without prognostic relevance.
Who pays?
The costs of any screening procedure in a person without health complaints should not be covered by basic health insurances but rather by the individual or an association or organising body. Further testing which is necessary because of abnormal initial findings is subject to coverage by health insurances.
Conclusion
Physical activity although promoting health may also provoke sudden death. In healthy individuals the risks of low-level athletic activities can be minimised by a careful personal and family history and physical examination. Before engaging in competitive sports a resting ECG is recommended to detect some rare anomalies with increased risk during heavy exertion. Anomalous findings then need meticulous further evaluation. In patients with known heart disease or with multiple cardiovascular risk factors exercise testing and imaging tests are recommended according to clinical needs.
References
- Batty, G.D.; Lee, I.M. Physical activity and coronary heart disease: 50 years of research confirms inverse relationship. BMJ 2004, 328, 1089–1090. [Google Scholar] [CrossRef] [PubMed]
- Borjesson, M.; Assanelli, D.; Carre, F.; Dugmore, D.; Panhuyzen-Goedkoop, N.M.; Seiler, C.; et al. (ESC Study Group of Sports Cardiology). Recommendations for participation in leisure-time physical activity and competitive sports for patients with ischemic heart disease. Eur. J. Cardiovasc. Prev. Rehabil. 2006, 13, 133–136. [Google Scholar] [CrossRef]
- Haskell, W.L.; Lee, I.M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med. Sci. Sports Exerc. 2007, 39, 1423–1434. [Google Scholar] [CrossRef] [PubMed]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.; Duncan, P.W.; Judge, J.O.; King, A.C.; et al. Physical activity and public health in older adults. Circulation 2007, 116, 1094–1105. [Google Scholar] [CrossRef] [PubMed]
- Maron, B.J. Sudden death in young athletes. New Engl. J. Med. 2003, 349, 1064–1075. [Google Scholar] [CrossRef]
- Franklin, B.A. Cardiovascular events associated with exercise. The riskprotection paradox. J. Cardiopulm. Rehabil. 2005, 25, 189–195. [Google Scholar] [CrossRef]
- Thompson, P.D.; Franklin, B.A.; Balady, G.J.; Blair, S.N.; Corrado, D.; Estes, N.A.M.; et al. Exercise and acute cardiovascular events (AHA scientific statement). Circulation 2007, 115, 2358–2368. [Google Scholar]
- Maron, B.J.; Araujo, C.G.S.; Thompson, P.D.; Fletcher, G.F.; Bayes de Luna, A.; Fleg, J.L.; et al. Recommendations for preparticipation screening and the assessment of cardiovascular disease in masters athletes. Circulation 2001, 103, 327–334. [Google Scholar] [CrossRef]
- Pavy, B.; Iliou, M.C.; Meurin, P.; Tabet, J.Y.; Corone, S. Safety of exercise training for cardiac patients: results of the French registry of complications during cardiac rehabilitation. Arch. Intern. Med. 2006, 166, 2329–2334. [Google Scholar] [CrossRef]
- Maron, B.J.; Shirani, J.; Poliac, L.C.; Mathenge, R.; Roberts, W.C.; Mueller, F.O. Sudden death in young competitive athletes: clinical, demographic, and pathological profile. JAMA 1996, 276, 199–204. [Google Scholar] [CrossRef]
- Corrado, D.; Migliore, F.; Basso, C.; Thiene, G. Exercise and the risk of sudden cardiac death. Herz 2006, 31, 553–558. [Google Scholar] [CrossRef]
- Link, M.S.; Estes, N.A.M. Sudden cardiac death in athletes. Prog. Cardiovasc. Dis. 2008, 51, 44–57. [Google Scholar] [CrossRef]
- Maron, B.J.; Chaitman, B.R.; Ackermann, M.J.; Bayes de Luna, A.; Corrado, D.; Crosson, J.E.; et al. Recommendations for physical activity and recreational sports participation for young patients with genetic cardiovascular diseases. Circulation 2004, 109, 2807–2816. [Google Scholar] [CrossRef]
- Pellicia, A.; Fagard, R.; Bjornstad, H.H.; Anastassakis, A.; Arbustini, E.; Assanelli, D.; et al. (Consensus document of the ESC). Recommendations for competitive sports participation in athletes with cardiovascular disease. Eur. Heart J. 2005, 26, 1422–1445. [Google Scholar]
- Löllgen, H.; Hansel JBoldt, F.; et al. (Arbeitsgruppe der DGSP). Leitlinie Vorsorgeuntersuchung im Sport DGSP 2007. Available online: website www.dgsp.de (accessed on 16 May 2009).
- Hoffmann, A.; Isler, R. Kardiale Beurteilung der Sporttauglichkeit. Schweiz. Med. Forum. 2007, 44, 889–894. [Google Scholar] [CrossRef]
- Corrado, D.; McKenna, W. Appropriate interpretation of the athlete’s electrocardiogram saves lives as well as money. Eur. Heart J. 2007, 28, 1920–1922. [Google Scholar] [CrossRef]
- Pellicia, A.; Culasso, F.; DiPaolo, F.M.; Accettura, D.; Cantore, R.; Castagna, W.; et al. Prevalence of abnormal electrocardiograms in a large unselected population undergoing preparticipation cardiovascular screening. Eur. Heart J. 2007, 28, 2006–2010. [Google Scholar] [CrossRef] [PubMed]
- Pellicia, A.; DiPaolo, F.M.; Corrado, D. Evidence for efficacy of the Italian national preparticipation screening programme for identification of hypertrophic cardiomyopathy in competitive athletes. Eur. Heart J. 2006, 27, 2196–2200. [Google Scholar] [CrossRef] [PubMed]
- Corrado, D.; Basso, C.; Pavei, A.; Michieli, P.; Schiavon, M.; Thiene, G. Trends in sudden cardiovascular death in young competitive athletes after implementation of a preparticipation screening program. JAMA 2006, 296, 1593–1601. [Google Scholar] [CrossRef] [PubMed]
- Lauer, M.; Froelicher, E.S.; Williams, M.; Kligfield, P. Exercise testing in asymptomatic adults (AHA scientific statement). Circulation 2005, 112, 771–776. [Google Scholar] [CrossRef]
- Maron, B.J.; Thompson, P.D.; Puffer, J.C.; McGrew, C.A.; Strong, W.B.; Douglas, P.S.; et al. (AHA statement for health professionals). Cardiovascular preparticipation screening of competitive athletes. Circulation 1996, 94, 850–856. [Google Scholar] [CrossRef] [PubMed]
- Carek, P.J.; Mainous, A. The preparticipation physical examination for athletics: a systematic review of current recommendations. BMJ 2003, 327, E170. [Google Scholar]
© 2025 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).