Survival Analysis
During a mean follow-up of 6.1 ± 1.5 years, the following events were observed: 32 cardiac deaths and 12 non-fatal myocardial infarctions.
Patients with versus without MACE are shown in
Table 1. Patients without MACE reached a higher peak heart rate, a higher peak systolic blood pressure, higher peak double product, higher peak work load and higher duration of exercise.
Individuals with MACE had a higher mean LHR as compared to subjects without MACE (0.44 ± 0.12 vs 0.40 ± 0.08, p = 0.0022), had a higher ungated left ventricular volume after exercise (109 ± 80 ml vs 62 ± 33 ml, p <0.0001) and before exercise (104 ± 74 ml vs 63 ± 31, p <0.0001), but TID showed only marginal statistical significance (1.02 ± 0.12 vs 0.97 ± 0.13, p = 0.0203). Perfusion defect size after exercise as well as at rest were also significant predictors of MACE (SSS: 11 ± 10 vs 6 ± 8, p <0.0001 and SRS: 7 ± 9 vs 3 ± 6, p <0.0001), however, summed difference scores (SDS) reflecting exercise induced ischaemia were not significant (SDS: 4 ± 9 vs 3 ± 6, p = 0.0597).
Table 2.
Event rates for MACE in relation to SSS, peak heart rate, and history of coronary artery disease.
Table 2.
Event rates for MACE in relation to SSS, peak heart rate, and history of coronary artery disease.
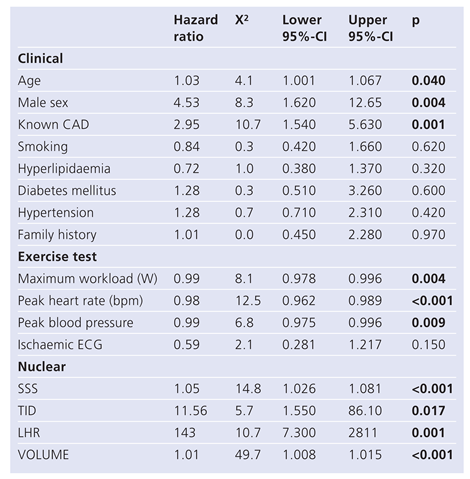
The hazard ratios (HR) for MACE (
Table 3) were significant for age (1.03, p = 0.040), for gender (4.53, p = 0.004), for known CAD (2.95, p = 0.001), for maximum workload achieved in Watt (0.99, p = 0.004), for peak heart rate (0.98, p <0.001), for peak blood pressure (0.99, p = 0.009), for SSS (1.05, p <0.001), for TID (11.56, p = 0.017), for LHR (143, 0.001) and for ungated left ventricular volumes (1.01, p <0.001).
Table 3.
Univariate predictors of MACE based on hazard ratios.
Table 3.
Univariate predictors of MACE based on hazard ratios.
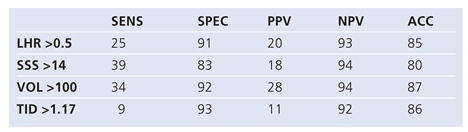
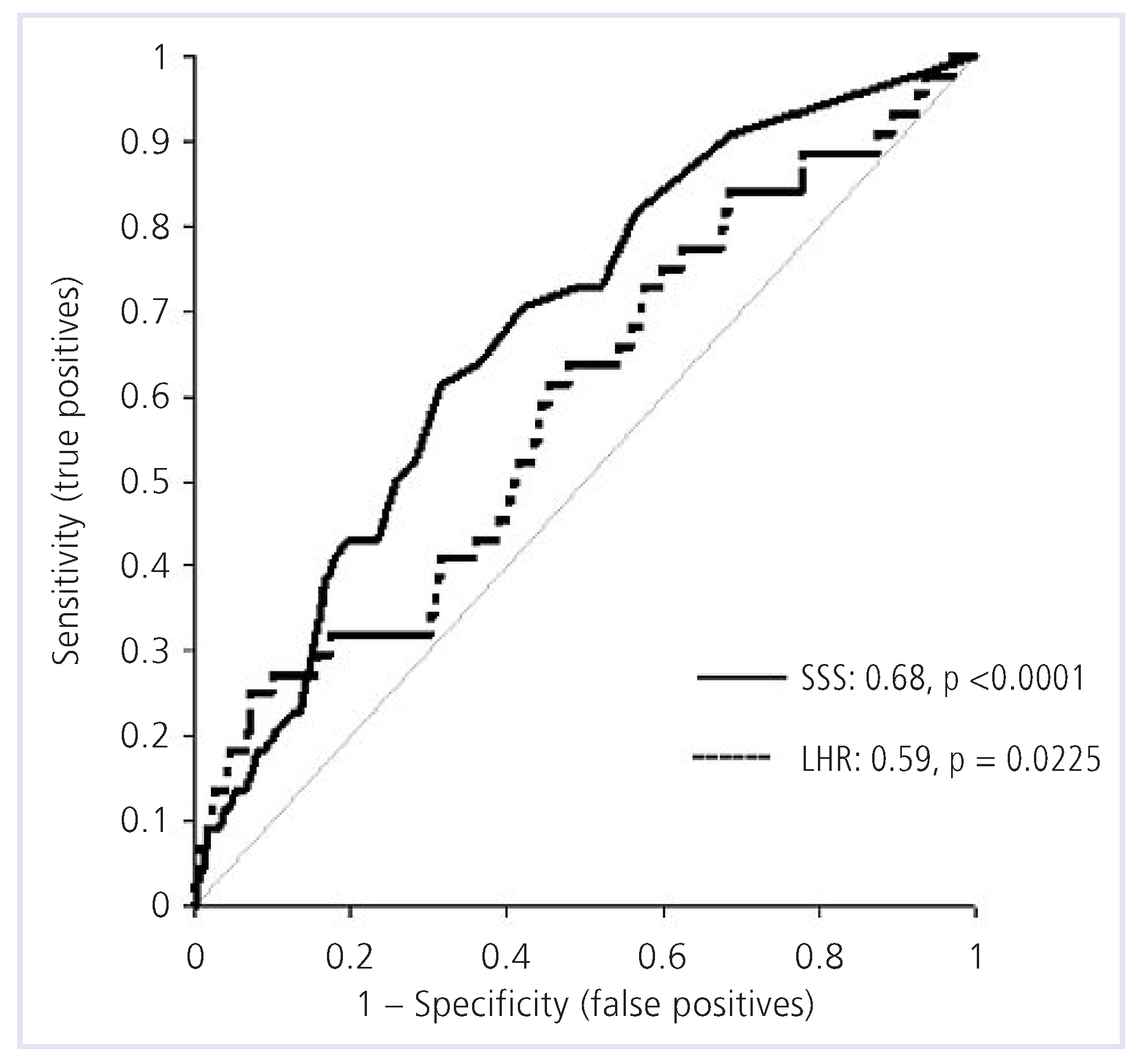
Using ROC analysis (
Table 4A), the highest areas under the curve for MACE were found for exercise double product (AUC 0.67), for SSS (AUC 0.68) and for ungated left ventricular volumes (0.68). Based on our previously published normal values for TID (cut-off defining abnormality: 1.17 [
7]) and LHR (cut-off defining abnormality: 0.5) the sensitivity and specificity to detect MACE was 9% and 93% for TID and 25% and 91% for LHR (
Table 4B). Cut-offs for SSS were based on the literature [
1,
2,
3,
4] and for VOL on a ROC analysis (ROC data not shown). SSS >14 had a sensitivity and specificity of 39% and 83% to detect MACE, respectively, and VOL ≥100 ml had a sensitivity and specificity of 34% and 93%, respectively.
The ROC curve for SSS and LHR is displayed in
Figure 1. The contrast between the two tests was 9% (p = 0.086), therefore, based on ROC analysis in this patient group, LHR did not add significant diagnostic information over SSS.
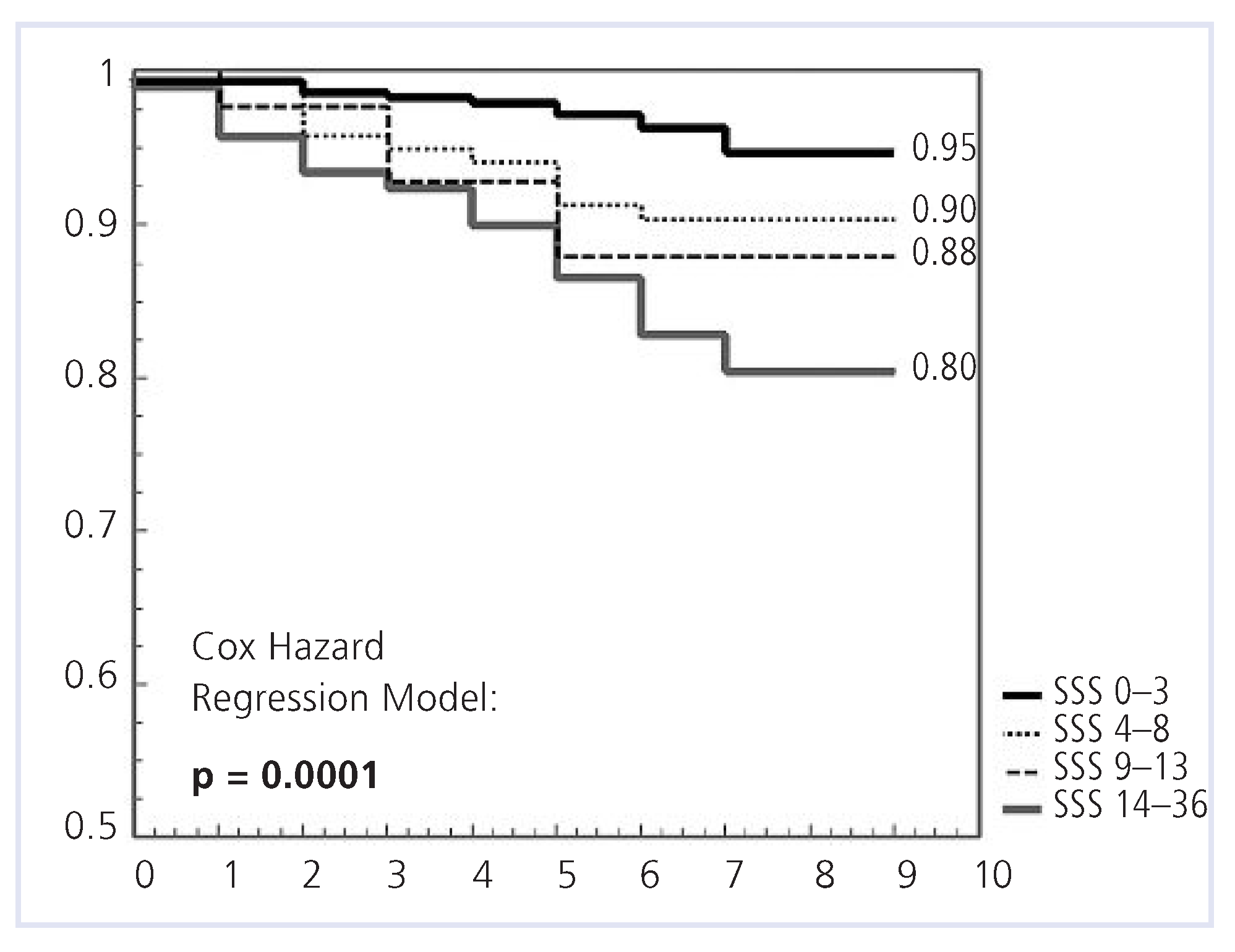
Cox analysis showed no significant predictive value of EST regarding MACE-free survival (p = 0.86). MACE-free survival was high with SSS <4 (95%) and significantly lower with SSS >13 (80%, p = 0.0001,
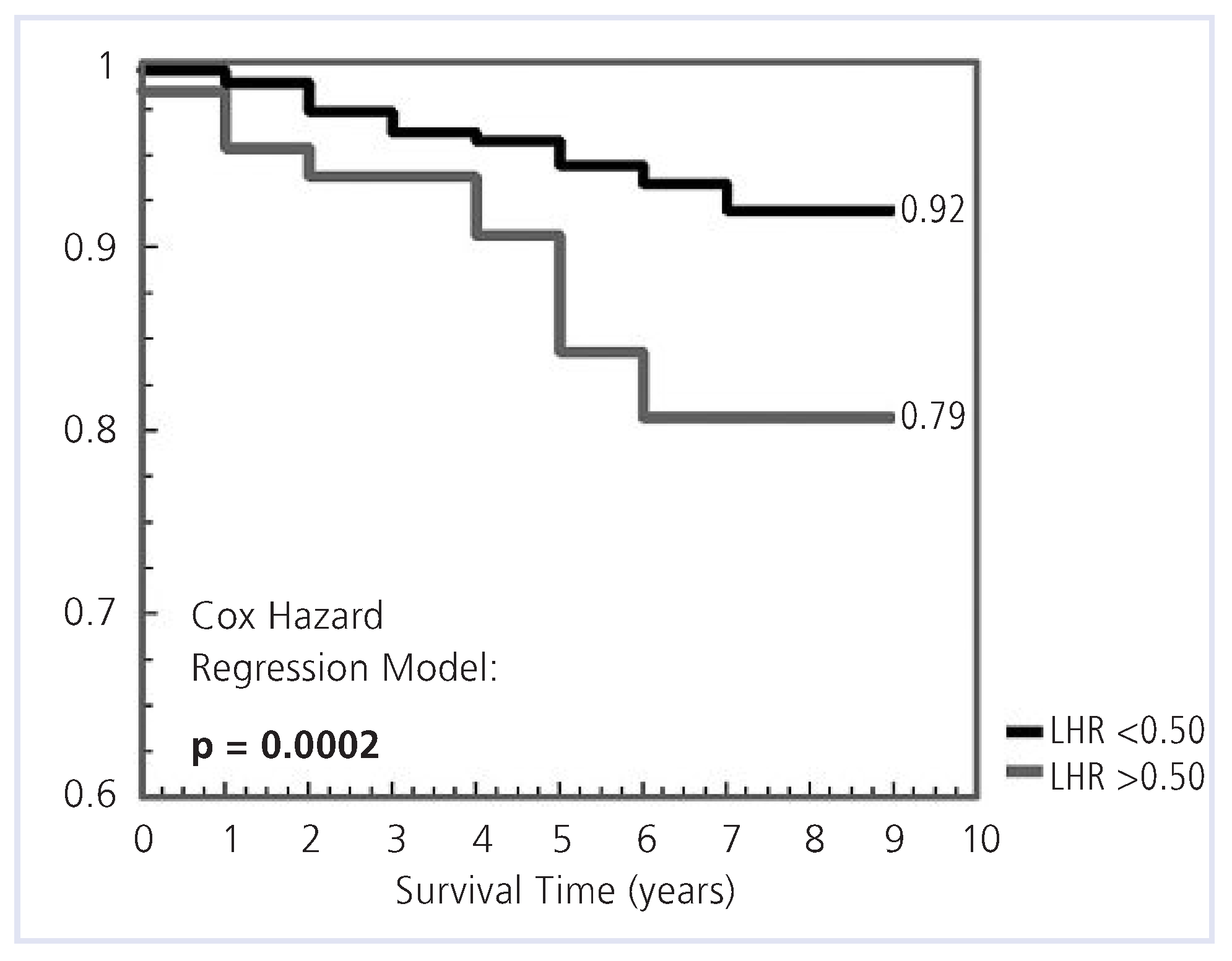
Figure 2). Similarly, LHR risk stratified patients effectively. Patient with a LHR <0.5 and >0.5 had a survival of 92% and 79%, respectively (p = 0.0002,
Figure 3). For a TID <0.98, survival was 94%; and for a TID >0.98, survival was 86% (p = 0.007). For VOL <100, survival was 93%; whereas for VOL ≥100, MACE-free survival was only 70% (p <0.001).
Table 4A.
Major variables predicting MACE in ROC analysis.
Table 4A.
Major variables predicting MACE in ROC analysis.
Table 4B.
Accuracies of LHR, SSS, VOL, TID, to detect MACE.
Table 4B.
Accuracies of LHR, SSS, VOL, TID, to detect MACE.
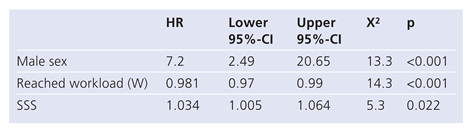
By including the information that was derived from baseline characteristics, EST, SSS, and LHR using Cox-multivariate predictors of MACE in the final model, only male gender, the cardiac workload level attained, and the SSS remained significant independent predictors for MACE (
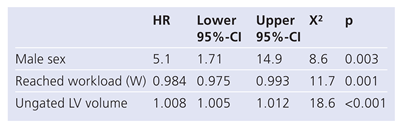
Table 5). When the new variable, VOL, was incorporated in the final model, male gender, the cardiac workload level attained, and VOL were identified as independent predictors of MACE (
Table 6).
Table 5.
Final COX model with standard variables.
Table 5.
Final COX model with standard variables.
Table 6.
Final COX model that incorporates VOL.
Table 6.
Final COX model that incorporates VOL.