Pulse: From Very Young to Very Old †
Abstract
Introduction
The physiological basis
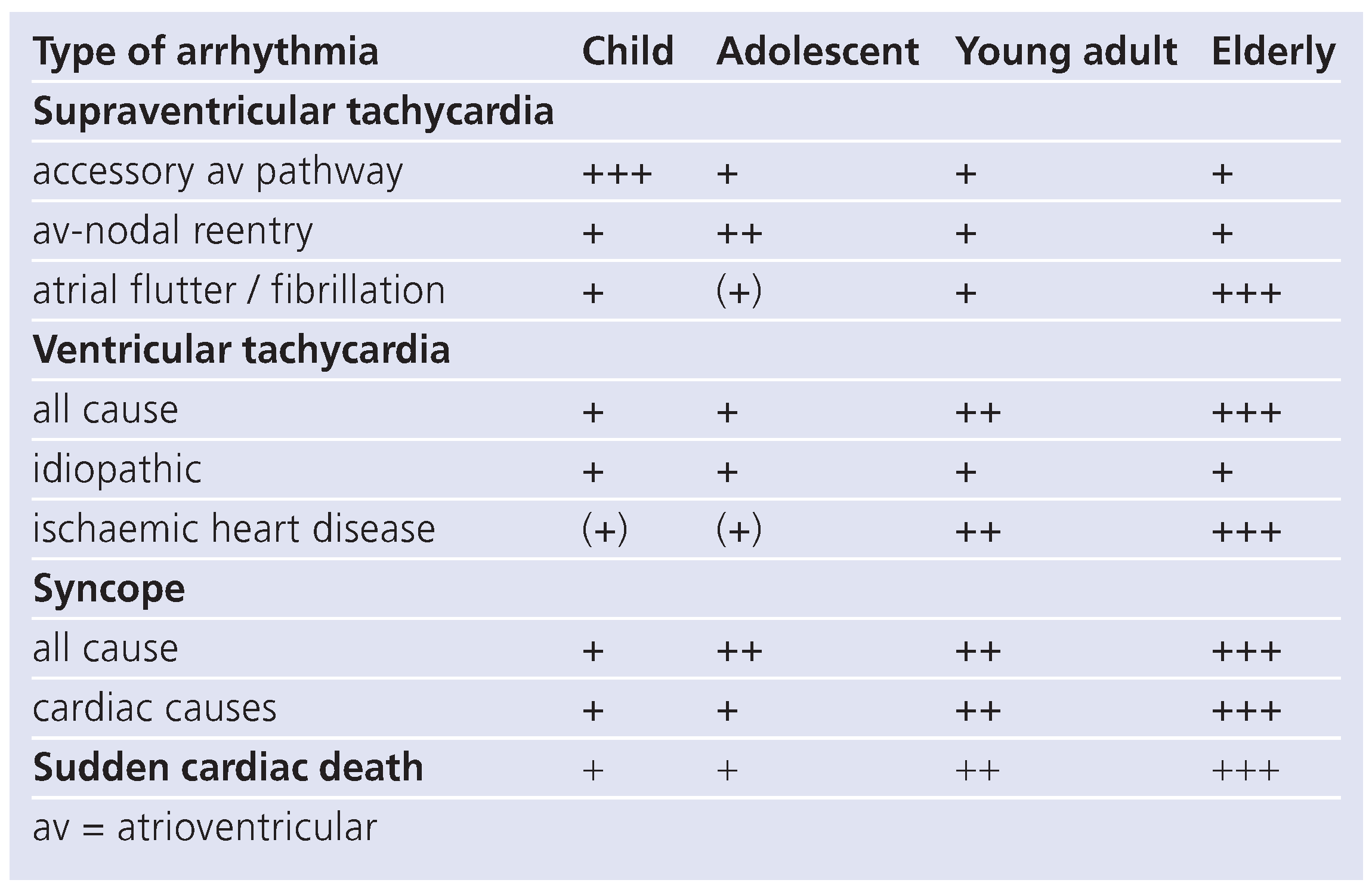
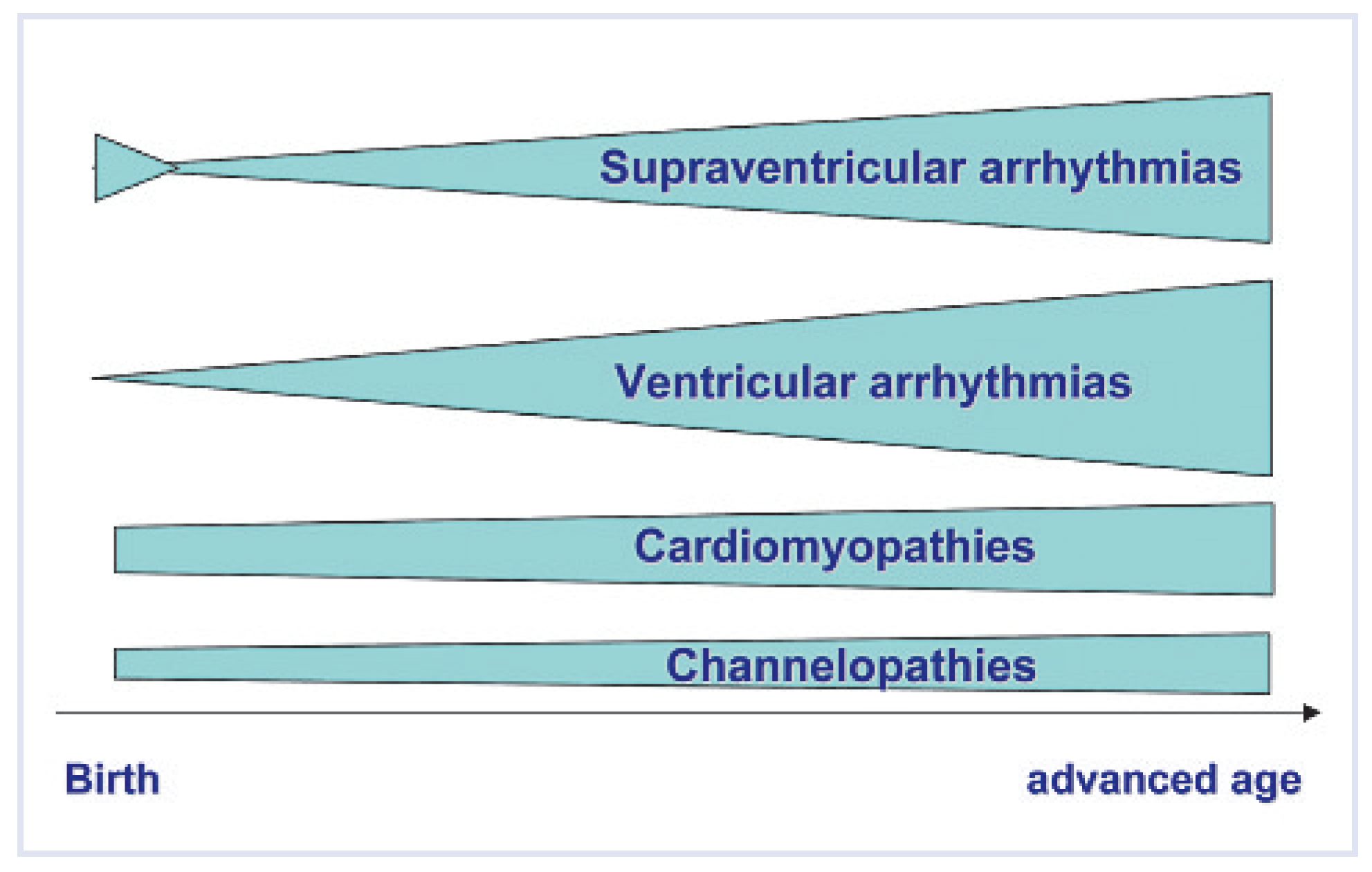
Distribution of types of arrhythmias trough all ages
- congenital malformations of the conduction system
- acquired disturbances of the conduction system
- predisposing genetic disease (channelopathies, cardiomyopathies)
- alterations in cardiac haemodynamics
- aging of the heart itself
- co-morbidities
Supraventricular arrhythmias in the different age groups
Ventricular arrhythmias in the different age groups
 |
Rhythmologic emergencies in the different age groups
Syncope in childhood and old age
Sudden cardiac death throughout all ages
Conflicts of Interest
References
- Jones, S.A.; Boyett, M.R.; Lancaster, M.K. Declining into failure: the age dependent loss of L-type calcium channel within the sinoatrial node. Circulation. 2007, 115, 1183–1190. [Google Scholar] [CrossRef]
- Kostin, S.; Klein, G.; Szalay, Z.; Hein, S.; Bauer, E.P.; Schaper, J. Structural correlate of atrial fibrillation in human patients. Cardiovasc Res. 2002, 54, 361–379. [Google Scholar] [CrossRef]
- Stein, M.; Noorman, M.; van Veen, T.; Herold, E.; Engelen, M.A.; Boulaksil, M.; et al. Dominant arrhythmia vulnerability of the right ventricle in senescent mice. Heart Rhythm. 2008, 5, 438–448. [Google Scholar] [CrossRef]
- Kojodjojo, P.; Kanagaratnam, P.; Markides, V.; Davies, W.; Peters, N. Age related changes in human left and right atrial conduction. J Cardiovasc Electrophysiol. 2006, 17, 120–127. [Google Scholar] [CrossRef]
- Lakireddy, D.R.; Clark, R.A.; Mohiuddin, S.M. Electrocardiographic findings in patients >100 years of age without clinical evidence of cardiac disease. Am J Cardiol. 2003, 92, 1249–1251. [Google Scholar] [CrossRef]
- Hornberger, L.K.; Sahn, D.J. Rhythm abnormalities of the fetus. Heart. 2007, 93, 1294–1300. [Google Scholar] [CrossRef]
- Kolditz, D.P.; Wijffels, M.C.; Blom, N.A.; van der Larse, A.; Markwald, R.R.; Schalij, M.J.; et al. Persistence of functional atrioventricular accessory pathways in postseptated embryonic avian hearts. Circulation. 2007, 115, 17–26. [Google Scholar] [CrossRef]
- Hahurij, N.D.; Gittenberger de Groot, A.C.; Kolditz, D.P.; Bökenkamp, R.; Schalij, M.J.; Poelmann, R.E.; et al. Accessory atrioventricular myocardial connections in the developing human heart. Circulation 2008, 117, 2850–2858. [Google Scholar] [CrossRef][Green Version]
- Ko, J.K.; Deal, B.J.; Strasburger, J.F.; Benson, W.D. Supraventricular tachycardia mechanisms and their age distribution in pediatric patients. Am J Cardiol. 1992, 69, 1028–1032. [Google Scholar] [CrossRef]
- Tortoriello, T.A.; Snyder, C.S.; Smith, E.; Fenrich, A.L.; Friedman, R.A.; Kertesz, N.J. Frequency of recurrence among infants with supraventricular tachycardia and comparison of recurrence rates among those with and without preexcitation. Am J Cardiol. 2003, 92, 1045–1049. [Google Scholar] [CrossRef]
- Kalusche, D.; Ott, P.; Arentz, T.; Stockinger, J.; Betz, P.; Roskamm, H. AV nodal reentry tachycardia in elderly patients: clinical presentation and results of radiofrequency catheter ablation. Coron Artery Dis. 1998, 9, 359–363. [Google Scholar] [CrossRef]
- Blaufox, A.D.; Paul, T.; Saul, J.P. Radiofrequency catheter ablation in small children. PACE. 2004, 27, 224–229. [Google Scholar] [CrossRef]
- Kolditz, D.P.; Blom, N.A.; Bökenkamp, R.; Schalij, M.J. Low-energy radiofrequency catheter ablation as therapy for supraventricular tachycardia in a premature neonate. Eur J Pediatr. 2005, 164, 559–562. [Google Scholar] [CrossRef]
- Bauersfeld, U.; Pfammatter, J.P.; Jaeggi, E. Treatment of supraventricular tachycardias in the new millenium: drugs or radiofrequency catheter ablation? Eur J Pediatr. 2001, 160, 1–9. [Google Scholar] [CrossRef]
- Meiltz, A.; Zimmermann, M. Atrioventricular nodal reentrant tachycardia in the elderly: efficacy and safety of radiofrequency catheter ablation. PACE. 2007, 30 (Suppl), S103–S107. [Google Scholar] [CrossRef]
- Roggen, A.; Pavlovic, M.; Pfammatter, J.P. Frequency of spontaneous ventricular tachycardia in a pediatric population. Am J Cardiol. 2008, 101, 852–854. [Google Scholar] [CrossRef]
- Davis, A.M.; Gow, R.M.; McCrindle, B.W.; Hamilton, R.M. Clinical spectrum, therapeutic management and follow-up of ventricular tachycardia in infants and young children. Am Heart J. 1996, 131, 186–191. [Google Scholar] [CrossRef]
- Pfammatter, J.P.; Paul, T. Idiopathic ventricular tachycardia in infancy and childhood. J Am Coll Cardiol. 1999, 33, 2067–2072. [Google Scholar] [CrossRef]
- Henkel, D.M.; Witt, B.J.; Gersh, B.J.; Jacobsen, S.J.; Weston, S.A.; Meverden, R.A.; et al. Ventricular arrhythmias after acute myocardial infarction: a 20 year community study. Am Heart J. 2006, 151, 806–812. [Google Scholar] [CrossRef]
- Simpson, J.M.; Garland, G.K. Fetal tachycardias: management and outcome of 127 consecutive cases. Heart. 1998, 79, 576–581. [Google Scholar] [CrossRef]
- Driscoll, D.J.; Jacobsen, S.J.; Porter, C.J.; Wollan, P.C. Syncope in children and adolescents. J Am Coll Cardiol. 1997, 29, 1039–1045. [Google Scholar] [CrossRef]
- Massin, M.M.; Bourguignont, A.; Coremans, C.; Comte, L.; Lepage, P.; Gerard, P. Syncope in pediatric patients presenting to an emergency department. J Pediatr. 2004, 145, 223–228. [Google Scholar] [CrossRef]
- Del Rosso, A.; Alboni, P.; Brignole, M.; Menozzi, C.; Raviele, A. Relation of clinical presentation of syncope to the age of patients. Am J Cardiol. 2005, 96, 1431–1435. [Google Scholar]
- Zipes, D.P.; Wellens, H.J.J. Sudden cardiac death. Circulation. 1998, 98, 2334–2351. [Google Scholar]
- Bauersfeld, U.; Tomaske, M.; Dodge-Khatami, A.; Rahn, M.; Kellenberger, C.J.; Pretre, R. Initial experience with implantable cardioverter defibrillator systems using epicardial and pleural electrodes in pediatric patients. Ann Thorac Surg. 2007, 84, 303–305. [Google Scholar] [CrossRef]
- Lotfi, K.; White, L.; Rea, T.; Cobb, L.; Copass, M.; Yin, L.; et al. Cardiac arrests in school. Circulation 2007, 116, 1374–1379. [Google Scholar] [CrossRef]

© 2009 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Pfammatter, J.-P. Pulse: From Very Young to Very Old. Cardiovasc. Med. 2009, 12, 13. https://doi.org/10.4414/cvm.2009.01382
Pfammatter J-P. Pulse: From Very Young to Very Old. Cardiovascular Medicine. 2009; 12(1):13. https://doi.org/10.4414/cvm.2009.01382
Chicago/Turabian StylePfammatter, Jean-Pierre. 2009. "Pulse: From Very Young to Very Old" Cardiovascular Medicine 12, no. 1: 13. https://doi.org/10.4414/cvm.2009.01382
APA StylePfammatter, J.-P. (2009). Pulse: From Very Young to Very Old. Cardiovascular Medicine, 12(1), 13. https://doi.org/10.4414/cvm.2009.01382




