Résumé
La relation entre le foramen ovale perméable est la migraine a été établie récemment. Nous avons évalué l’effet de la fermeture d’un foramen ovale perméable dans un groupe de patients qui nous a été référé pour bénéficier de cette intervention.
Tous les malades ont rempli un questionnaire afin d’évaluer leur status migraineux avant l’intervention, 6 mois et 1 an après la fermeture du foramen ovale. Avant l’intervention, chaque patient a bénéficié d’une évaluation clinique et d’un échocardiogramme transthoracique et transoesophagien. Nous avons traité 123 malades (58 hommes et 65 femmes) avec un âge moyen de 51 ± 10 ans. Vingt-huit d’entre eux (16%) (16 femmes et 12 hommes) souffraient de migraine typique avant l’intervention. Tous recevaient, avant la fermeture, un traitement anti-migraineux d’anti-inflammatoire et/ou de triptans. Six mois après l’intervention, le foramen était complètement fermé à l’état basal chez 94% des patients et un minime shunt de degré 1 à l’épreuve de Valsalva était présent chez 14% des patients. Un traitement de clopidogrel et d’acide acétylsalicylique (AAS) a été administré à tous les patients pendant 6 mois. Parmi les 28 patients souffrant de migraine, 10 (37%) n’ont plus présenté d’épisodes migraineux. Dix autres patients (37%) ont constaté une amélioration significative de leur symptômes avec une diminution d’au moins 50% de la fréquence des crises de migraine, avec également des crises moins douloureuses. Cinq patients (19%) n’ont pas signalé de changement et un patient (7%) a remarqué une aggravation de ses symptômes. Finalement un patient sans migraine avant la fermeture de son foramen ovale perméable a signalé l’apparition de migraine après l’intervention. Parmi les quatre malades avec migraine qui avaient un shunt résiduel après la fermeture du foramen ovale perméable, deux signalaient une amélioration de leur symptômes et deux aucun changement.
Au vu de ces résultats, nous concluons à un probable effet positif de la fermeture du foramen ovale perméable sur la fréquence et l’intensité des crises de migraine.
Mot-clefs: migraine; foramen ovale perméable
Introduction
The pathophysiological mechanism of the beneficial effects of PFO closure in patients with stroke and migraine remains unclear but a common pathway between thrombus and migraine may exist. PFO closure has a beneficial effect in some sub-groups of patients with migraine.
It has recently been shown that patent foramen ovale (PFO) may be involved in the development of migraine in some patients [
1], and that percutaneous closure of PFO may have significant beneficial effects in the outcome of this patient group [
2,
3,
4,
5,
6,
7,
8]. A causal relationship between PFO and migraine has been proposed. In individuals with a right-to-left shunt, a lower dose of venous trigger substances may be needed to induce migraine because the shunt permits the pulmonary filter to be bypassed [
9]. We evaluated the possible beneficial role of PFO closure in patients referred to our institution for this intervention.
Methods
All patients referred to our clinic between January 2000 and April 2006 for percutaneous closure of patent foramen ovale were included in a registry concerning the possible effect of PFO closure on the incidence of migraine attacks. All patients were fully informed and signed the appropriate consent form. Additionally, each patient completed the international headache questionnaire (see appendix) to determine their migraine status before treatment and again at 6 months and 1 year after PFO closure. Before intervention, all patients were evaluated clinically by transthoracic and transoesophageal echocardiography to demonstrate the PFO. All patients who underwent percutaneous closure of PFO were included in the registry.
Closure of the PFO was performed via the right femoral vein with transoesophageal echocardiography control under complete anaesthesia. The device implanted was the Intrasept (Cardia, Eagan, MN, USA). Artificial ventilation was assured with a laryngeal mask in order to avoid intubation. A 7 French introducer was placed in the femoral vein and the interatrial septum was crossed with a multipurpose catheter. At that time 70 U/kg of heparin was administered with 500 mg of ASA. Using an exchange wire, an 11 to 13 French Mullins catheter was advanced into the left atrium. Balloon sizing of the PFO was not performed. Device size was selected based on echocardiography aspects. A 25 mm diameter device was implanted in patients without aneurysm of the interatrial septum and a 30 or 35 mm diameter device in those with an aneurysm. The device was then folded and inserted into a 12 French introducer, loaded in the guiding catheter, and gently advanced to the tip of the Mullins. When correctly placed in the left atrium, the distal wing of the umbrella was opened under echocardiography control and applied against the left side of the interatrial septum. While maintaining slight traction in this position, the proximal wing was then opened in the right atrium. With both wings conforming flat against the septum and the defect fully covered, the device was release by opening the delivery forceps. Patients were then awakened and transferred to an intermediate care unit for 3 hours and then discharged on a chronic treatment of ASA and clopidogrel. A control echocardiography was performed the next morning or a dew days later for those who have left the hospital the same day. Antiplatelet therapy was maintained for 6 months and stopped unless a complication occurred. At follow-up transthoracic echocardiography with microbubble injection at rest and during the Valsalva maneuver was performed at 1, 30 and 180 days. Residual shunt was defined as follow: Grade 1 = no bubbles, grade 2 = 0–10 bubbles, grade 3 = 10–20 bubbles, grade 4 = more than 20 bubbles. Antibiotic prophylaxis was recommended for 6 months after implantation. The corresponding home physician and cardiologist followed each patient. Migraine relief definition was: 1 = complete absence of migraine; 2 = reduction in frequency (50% less episodes); 3 = no change or deterioration.
Results
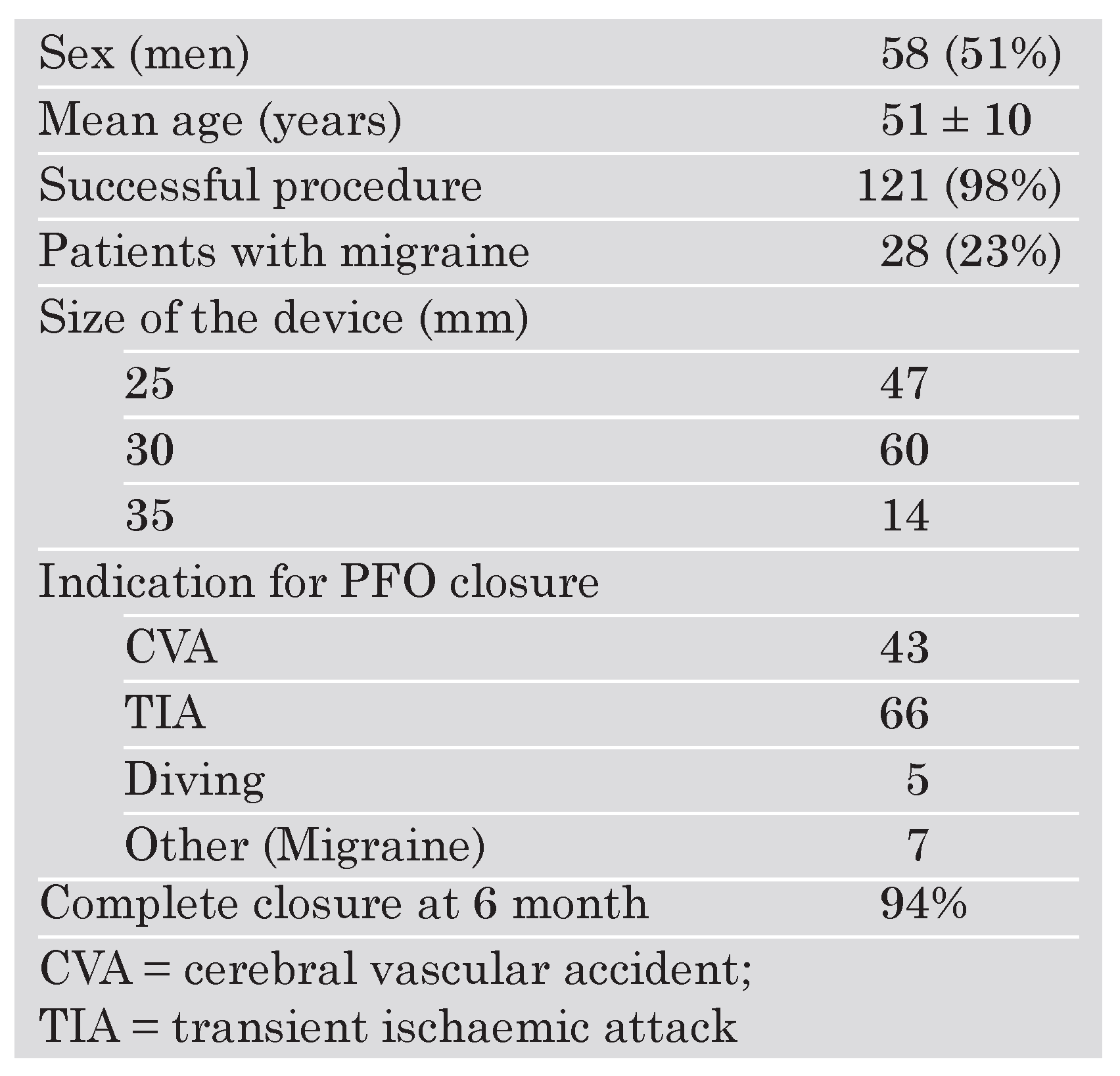
Closure of PFO was attempted in 123 patients (58 men and 65 women) with a mean age of 51 ± 10 years. The indication for PFO closure is indicated in
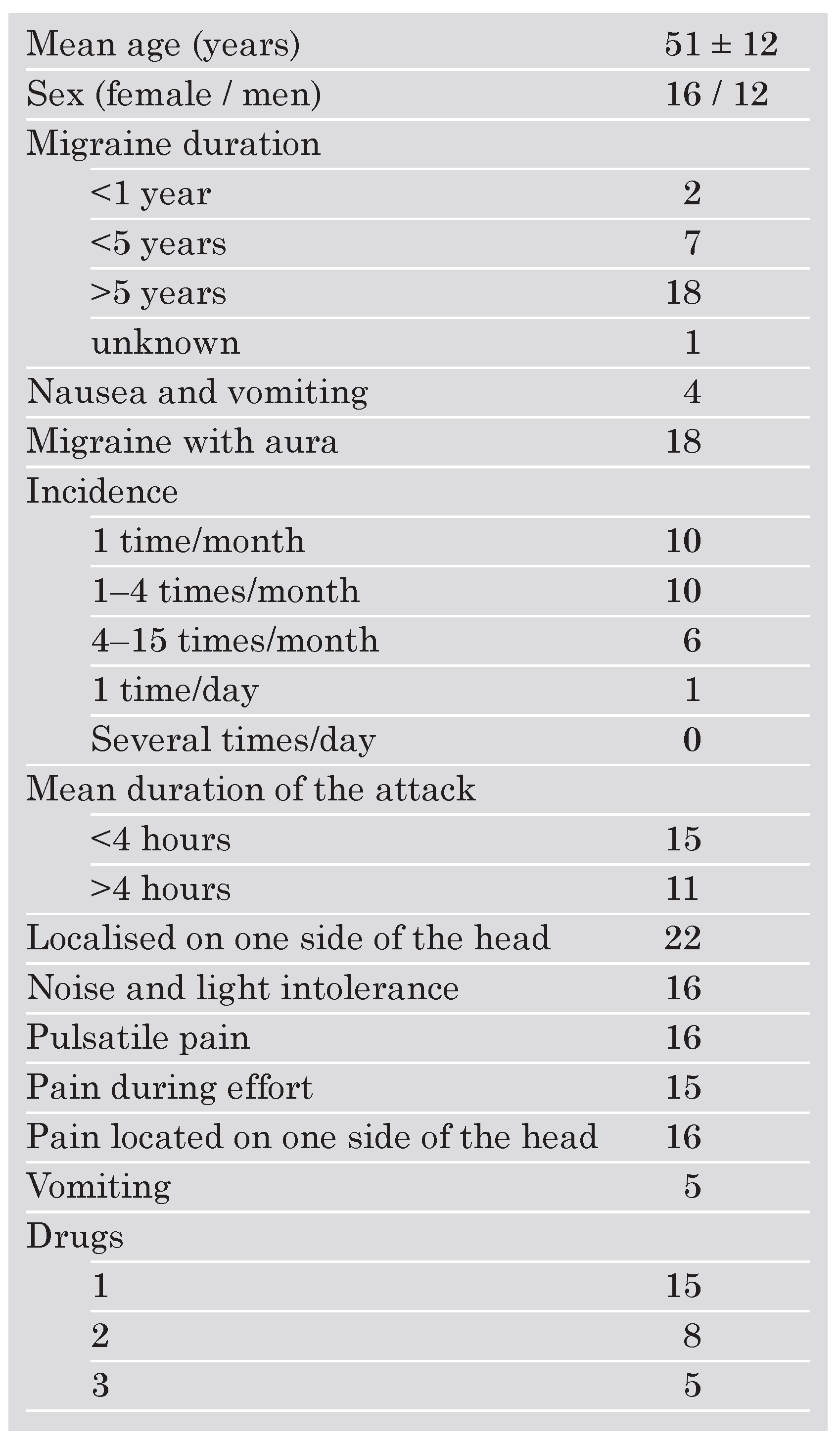
Table 1. Twenty-eight of these patients (23%) (16 women and 12 men) had true migraine attacks prior to intervention. The characteristics of these patients and the type of migraine are summarised in
Table 2. All patients were treated medically with anti-inflammatory drugs or triptan derivates before the intervention. They were also under ASA as a chronic treatment following their transient ischaemic attack. The device was successfully deployed and implanted in all patients except two (98%) in which the guiding catheter could not be positioned across the septum. The device sizes used (n = 121) were 25 mm in 47 patients (39%), 30 mm in 60 patients (49.5%) and 35 mm in 14 patients (11.5%). In-hospital complications occurred in four patients and consisted of air embolism in the right coronary artery in three patients. A transient (3 to 5 minutes) ST segment elevation was present in the inferior leads. No CK elevation was documented. In the fourth patient a transient amnesia occurred after the intervention but subsided after a few hours.
Table 1.
Characteristics of PFO patients (n = 123).
Table 1.
Characteristics of PFO patients (n = 123).
Table 2.
Characteristics of the patients with migraine (n = 28).
Table 2.
Characteristics of the patients with migraine (n = 28).
At 6 month follow-up the PFO was completely closed at rest in 94%. In the remaining patients a small (grade I), but non-significant residual shunt was present. At one year a complete follow-up was obtained for all patients and showed no dislodgement, perforation or thrombus present. The PFO was completely closed at rest in 106 of the 108 patients available for follow-up (99%). With Valsalva maneuver a grade 1 shunt was present in 15 patients (14%). Only one patient had a major bleeding incident probably related to the antiplatelet therapy. Among the 28 patients with migraine, 10 (37%) were completely free of migraine and another 10 patients (37%) reported a significant improvement in their symptoms with less attacks, less pain and were taking less medication. Five patients (19%) had no change and one patient (7%) had a significant worsening of symptoms. Finally one patient (1%) without migraine before the intervention started to have migraine attacks during follow-up. Among the 7 patients with migraine as primary indication to close the PFO, 4 were cured, 1 had some improvement and 2 did not report any changes.
Discussion
The prevalence of migraine in patients with cryptogenic stroke and PFO is higher than in normal subjects and occurs in approximately 30 to 40% of this group [
2,
3,
6,
7]. In our series only 23% of the base group were migraineurs. This difference may be related to the use of very severe inclusion criteria in our cohort of patients. Moreover, ours is a prospective registry compared to retrospective analysis in the previously mentioned trials. Despite this difference, we found a significant benefit of PFO closure. Even with our small number of patients we noted a remarkable effect of PFO closure with almost 37% of patients completely cured of their migraine attacks and another 37% significantly improved at time of follow-up. Similar to previously published reports, a significant reduction in overall frequency of migraine events was observed in almost 80% of the patients [
2,
3,
4,
5,
7]. Only one trial reports only a small clinical benefit with an improvement in 50% of the patients [
6]. However, this trial was conducted in patients with ASD, and not all patients had demonstrated stroke before ASD closure. This is clearly a different subset of patients than those included in the PFO trials. Even when a placebo effect is reported in trials on migraine treatment, it occurs in a lower proportion of patients (20–40%) [
9,
10].
In the preliminary data of the MIST (Migraine Intervention with Starflex Technology) trial, a 50% reduction in headache days frequency was achieved by 42% of patients who had PFO closure and the headache burden (frequency times duration) was reduced by 37% [
11]. The differences between our data and those of MIST may be due to the higher percent of women enrolled in the MIST trial (86%
vs 49%), and a lower percent of migraineurs in our total patient population (23%
vs 100%). Moreover, the residual shunt after closure (not indicated for MIST and only 6% in our trial) and a different treatment during follow-up (ASA and clopidogrel: 3 months versus 6 months) may partially explain the differences.
The pathophysiological mechanism of the beneficial effects of PFO closure in patients with stroke and migraine remains unclear but a common pathway between thrombus and migraine may exist. One can argue that the introduction of a double antiplatelet therapy (combination of aspirin and clopidogrel) may explain the favorable outcome. This is very improbable since, at 6 months, antiplatelet medication was stopped without recurrence of symptoms. The main limitation of this registry is its non-randomised design and the small number of patients. However, this study and others support and appear to demonstrate some beneficial effects of PFO closure on migraine attacks. Randomised, prospective trials are clearly warranted to confirm this beneficial effect and to elucidate its patho-physiological mechanism.