Variation on the Anchor Balloon Technique for Difficult Stent Delivery
Summary
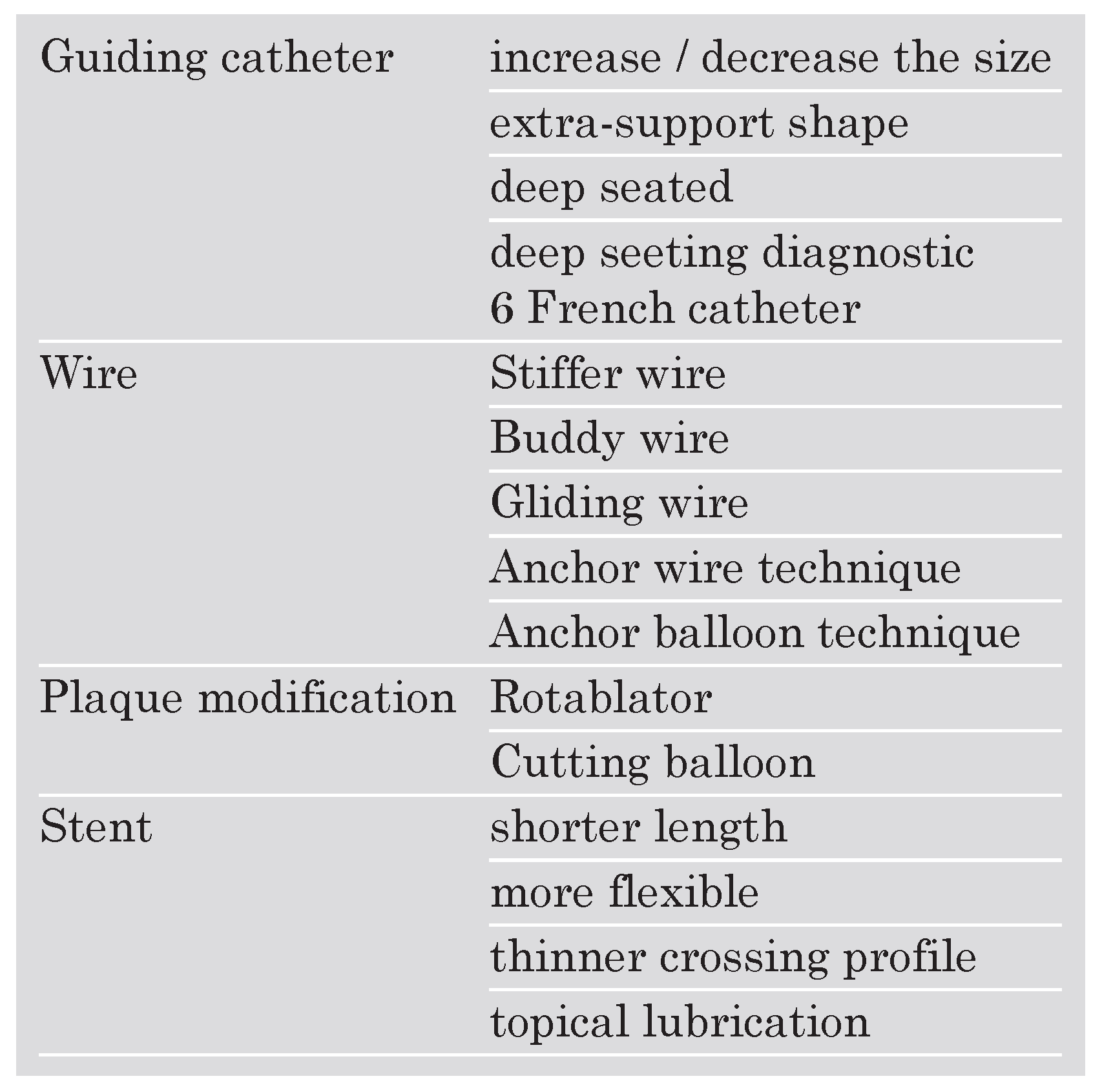
Introduction
 |
Case report
Discussion
Conflicts of Interest
References
- Cantor, W.J.; Lazzam, C.; Cohen, E.A.; Bowman, K.A.; Dolman, S.; Mackie, K.; et al. Failed coronary stent deployment. Am Heart J. 1998, 136, 1088–95. [Google Scholar] [CrossRef] [PubMed]
- Lohavanichbutr, K.; Webb, J.G.; Carere, R.G.; Solankhi, N.; Jarochowski, M.; D’Yachkova, Y.; et al. Mechanisms, management, and outcome of failure of delivery of coronary stents. Am J Cardiol. 1999, 83, 779–81, A779. [Google Scholar] [CrossRef] [PubMed]
- Fujita, S.; Tamai, H.; Kyo, E.; Kosuga, K.; Hata, T.; Okada, M.; et al. New technique for superior guiding catheter support during advancement of a balloon in coronary angioplasty: the anchor technique. Catheter Cardiovasc Interv. 2003, 59, 482–8. [Google Scholar] [CrossRef] [PubMed]
- Hirokami, M.; Saito, S.; Muto, H. Anchoring technique to improve guiding catheter support in coronary angioplasty of chronic total occlusions. Catheter Cardiovasc Interv. 2006, 67, 366–71. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.; Sulke, N.; Taub, N.; Sowton, E. Clinical and lesion morphologic determinants of coronary angioplasty success and complications: current experience. J Am Coll Cardiol. 1995, 25, 855–65. [Google Scholar] [CrossRef] [PubMed]
- Bartorelli, A.L.; Lavarra, F.; Trabattoni, D.; Fabbiocchi, F.; Loaldi, A.; Galli, S.; et al. Successful stent delivery with deep seating of 6 French guiding catheters in difficult coronary anatomy. Catheter Cardiovasc Interv. 1999, 48, 279–84. [Google Scholar] [CrossRef]
- Keller, P.F.; Gosselin, G.; Gregoire, J.; Guedes, A.; Verin, V. Feasibility of the PCI through 6F diagnostic catheters. Catheter Cardiovasc Interv. 2007, 69, 410–5. [Google Scholar] [CrossRef] [PubMed]
- Chan, A.W.; Ramee, S.R.; Collins, T.; Quintana, H.; White, C.J. Rotaglide-facilitated stent delivery: mission accomplished. Catheter Cardiovasc Interv. 2003, 59, 477–81. [Google Scholar] [CrossRef] [PubMed]


© 2007 by the authors. Attribution - Non-Commercial - NoDerivatives 4.0.
Share and Cite
Surmely, J.-F.; Cook, S. Variation on the Anchor Balloon Technique for Difficult Stent Delivery. Cardiovasc. Med. 2007, 10, 397. https://doi.org/10.4414/cvm.2007.01284
Surmely J-F, Cook S. Variation on the Anchor Balloon Technique for Difficult Stent Delivery. Cardiovascular Medicine. 2007; 10(12):397. https://doi.org/10.4414/cvm.2007.01284
Chicago/Turabian StyleSurmely, Jean-François, and Stéphane Cook. 2007. "Variation on the Anchor Balloon Technique for Difficult Stent Delivery" Cardiovascular Medicine 10, no. 12: 397. https://doi.org/10.4414/cvm.2007.01284
APA StyleSurmely, J.-F., & Cook, S. (2007). Variation on the Anchor Balloon Technique for Difficult Stent Delivery. Cardiovascular Medicine, 10(12), 397. https://doi.org/10.4414/cvm.2007.01284




