Estimated Time for Occurrence of Smoking-Related Consequences among Pregnant and Non-Pregnant Women
Abstract
:Objectives:
Methods:
Results:
Conclusion:
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Statistical Methods and Data Management
3. Results
3.1. Specification of the Sample
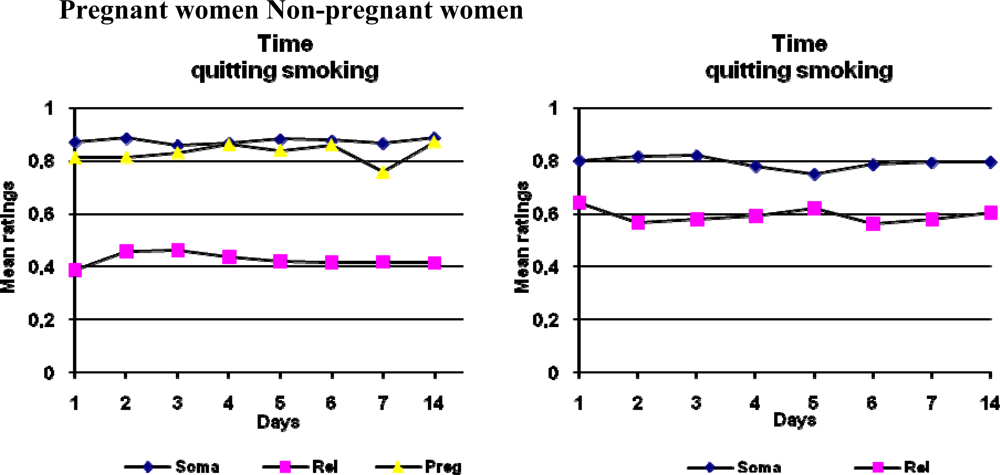
3.2. Estimated Time for Consequences to Occur Given Continuing or Quitting Smoking
4. Discussion
5. Conclusions
References
- Raatikainen, K; Huurinainen, P; Heinonen, S. Smoking in early gestation or through pregnancy: a decision crucial to pregnancy outcome. Prev. Med 2007, 44, 59–63. [Google Scholar]
- Reichert, VC; Seltzer, V; Efferen, LS; Kohn, N. Women and tobacco dependence. Med. Clin. North. Am 2004, 88, 1467–1481. [Google Scholar]
- Lawrence, T; Aveyard, P; Cheng, KK; Griffin, C; Johnson, C; Croghan, E. Does stage-based smoking cessation advice in pregnancy result in long-term quitters? 18-month postpartum followup of a randomized controlled trial. Addiction 2005, 100, 107–116. [Google Scholar]
- DiClemente, CC; Schlundt, D; Gemmell, L. Readiness and stages of change in addiction treatment. Am. J. Addict 2004, 13, 103–119. [Google Scholar]
- Droomers, M; Schrijvers, CT; Mackenbach, JP. Educational differences in the intention to stop smoking: explanations based on the Theory of Planned Behaviour. Eur. J. Public Health 2004, 14, 194–198. [Google Scholar]
- Bretteville-Jensen, AL. Addiction and discounting. J. Health Econ 1999, 18, 393–407. [Google Scholar]
- Ferguson, BS. Economic modeling of the rational consumption of addictive substances. Subst. Use Misuse 2006, 41, 573–603. [Google Scholar]
- Doran, N; McChargue, D; Cohen, L. Impulsivity and the reinforcing value of cigarette smoking. Addict. Behav 2007, 32, 90–98. [Google Scholar]
- Reynolds, B; Richards, JB; Horn, K; Karraker, K. Delay discounting and probability discounting as related to cigarette smoking status in adults. Behav. Process 2004, 65, 35–42. [Google Scholar]
- Yoon, JH; Higgins, ST; Heil, SH; Sugarbaker, RJ; Thomas, CS; Badger, GJ. Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Exp. Clin. Psychopharmacol 2007, 15, 176–186. [Google Scholar]
- Baker, F; Johnson, MW; Bickel, WK. Delay discounting in current and never-before cigarette smokers: similarities and differences across commodity, sign, and magnitude. J. Abnorm. Psychol 2003, 112, 382–392. [Google Scholar]
- Reynolds, B; Karraker, K; Horn, K; Richards, JB. Delay and probability discounting as related to different stages of adolescent smoking and non-smoking. Behav. Process 2003, 64, 333–344. [Google Scholar]
- Hughes, JR; Keely, JP; Fagerstrom, KO; Callas, PW. Intentions to quit smoking change over short periods of time. Addict. Behav 2005, 30, 653–662. [Google Scholar]
- Daniel, WW. Biostatistics: A foundation for analysis in the health sciences, 6th ed; John Wiley & Sons: New York, NY, USA, 1995. [Google Scholar]
- Pickett, KE; Wakschlag, LS; Dai, L; Leventhal, BL. Fluctuations of maternal smoking during pregnancy. Obstet. Gynecol 2003, 101, 140–147. [Google Scholar]
- Larabie, LC. To what extent do smokers plan quit attempts? Tob. Control 2005, 14, 425–428. [Google Scholar]
- Odum, AL; Madden, GJ; Bickel, WK. Discounting of delayed health gains and losses by current, never- and ex-smokers of cigarettes. Nicotine Tob. Res 2002, 4, 295–303. [Google Scholar]
- Lumley, J; Oliver, SS; Chamberlain, C; Oakley, L. Interventions for promoting smoking cessation during pregnancy. Cochrane Database Syst Rev 2004, 18, CD001055. [Google Scholar]
- Mullen, PD. How can more smoking suspension during pregnancy become lifelong abstinence? Lessons learned about predictors, interventions, and gaps in our accumulated knowledge. Nicotine Tob. Res 2004, 6, 217–238. [Google Scholar]
- Judge, K; Bauld, L; Chesterman, J; Ferguson, J. The English smoking treatment services: shortterm outcomes. Addiction 2005, 100, 46–58. [Google Scholar]
- Abdullah, AS; Yam, HK. Intention to quit smoking, attempts to quit, and successful quitting among Hong Kong Chinese smokers: population prevalence and predictors. Am. J. Health Promot 2005, 19, 346–354. [Google Scholar]
- McDermott, L; Dobson, A; Owen, N. Determinants of continuity and change over 10 years in young women’s smoking. Addiction 2009, 104, 478–487. [Google Scholar]
- Balabanova, D; Bobak, M; McKee, M. Patterns of smoking in Bulgaria. Tob. Control 1998, 7, 383–385. [Google Scholar]
- Etter, JF. Associations between smoking prevalence, stages of change, cigarette consumption, and quit attempts across the United States. Prev. Med 2004, 38, 369–373. [Google Scholar]
- Kralikova, E; Bajerova, J; Raslova, N; Rames, J; Himmerova, V. Smoking and pregnancy: prevalence, knowledge, anthropometry, risk communication. Prague Med. Rep 2005, 106, 195–200. [Google Scholar]
- Yoon, JH; Higgins, ST; Hell, SH; Sugarbaker, RJ; Thomas, CS; Badger, GJ. Delay discounting predicts postpartum relapse to cigarette smoking among pregnant women. Exp. Clin. Psychopharmacol 2007, 15, 176–186. [Google Scholar]
- Khwaja, A; Silverman, D; Sloan, F. Time preference, time discounting, and smoking decisions. J. Health Econ 2007, 26, 927–949. [Google Scholar]

| Somatic health consequences |
| Your physical condition becomes worse |
| You are afflicted with heart disease |
| You feel pain in your chest |
| You get lung cancer |
| Your life expectancy becomes shorter |
| You lose some of your physical strength
|
| Consequences related to mood and social relations |
| Others like you |
| You have good relations with others |
| You feel free to do whatever you wish |
| Your self-confidence improves |
| You satisfy others who worry about your health |
| You feel pleasure and satisfaction
|
| Consequences related to pregnancy |
| You worry about the future health of your unborn child |
| You influence the condition of your fetus in a negative manner |
| Your home environment is unhealthy for children |
| Your own health during pregnancy is at risk |
| Your home environment can cause allergy in children |
| Your child will become a smoker |
| You have a miscarriage |
| You have a child with a low birth weight |
| You have a difficult child delivery |
| Mean | SD | Median | Range | |
|---|---|---|---|---|
Pregnant women not intending to quit (n=20) | ||||
| Age | 24.1 | 3.28 | 24.0 | 20–30 |
| Number of years of smoking | 5.1 | 3.15 | 4.5 | 1–11 |
| Number of earlier attempts | 1.8 | 2.63 | 1.0 | 0–10 |
Pregnant women intending to quit (n=20) | ||||
| Age | 25.2 | 3.96 | 24.5 | 20–31 |
| Number of years of smoking | 5.8 | 2.51 | 5.0 | 3–13 |
| Number of earlier attempts | 2.4 | 2.22 | 2.0 | 0–10 |
| Number of cigarettes per day | 11.2 | 4.66 | 10.0 | 4–20 |
Non-pregnant women not intending to quit (n=20) | ||||
| Age | 26.7 | 3.86 | 27.5 | 20–31 |
| Number of years of smoking | 8.7 | 4.22 | 9.5 | 2–16 |
| Number of earlier attempts | 4.0 | 2.96 | 3.5 | 0–12 |
| Number of cigarettes per day | 10.2 | 3.86 | 10.0 | 4–20 |
Total (n=80) | ||||
| Age | 25.1 | 3.79 | 25.0 | 20–31 |
| Number of years of smoking | 6.5 | 3.51 | 6.0 | 1–16 |
| Number of earlier attempts | 2.5 | 2.52 | 2.0 | 0–12 |
| Number of cigarettes per day | 10.5 | 4.58 | 10.0 | 4–20 |
| Kruskal-Wallis test for group differences | Chi-Square | df | p-value | |
| Age | 4.805 | 3 | 0.187 | |
| Number of years of smoking | 7.223 | 3 | 0.065 | |
| Number of earlier attempts | 13.797 | 3 | 0.003** | |
| Number of cigarettes per day | 2.429 | 3 | 0.488 | |
| Somatic health | Mood and social relations | Pregnancy | ||||
|---|---|---|---|---|---|---|
| F-value | Probability | F-value | Probability | F-value | Probability | |
TIME | ||||||
| continuing smoking | ||||||
| PREGNANT | 2.19 | 0.14 | 8.16 | 0.0055* | – | – |
| QUITTING | 4.41 | 0.0391* | 0.07 | 0.79 | 0.77 | 0.38 |
| PREGNANT*QUITTING | 0.51 | 0.83 | 0.14 | 0.99 | 12.45 | 0.0001* |
| DAYS | 0.51 | 0.83 | 0.14 | 0.99 | 12.45 | 0.0001* |
| PREGNANT*QUITTING | 0.12 | 0.74 | 0.17 | 0.68 | – | – |
| PREGNANT*DAYS | 0.71 | 0.67 | 0.63 | 0.73 | – | – |
| QUITTING*DAYS | 0.75 | 0.63 | 1.20 | 0.30 | 1.94 | 0.06 |
TIME | ||||||
| quitting smoking | ||||||
| PREGNANT | 0.50 | 0.48 | 9.03 | 0.0036* | – | – |
| QUITTING | 0.03 | 0.86 | 5.21 | 0.0252* | 0.08 | 0.78 |
| DAYS | 0.47 | 0.86 | 0.73 | 0.65 | 2.35 | 0.0240 |
| PREGNANT*QUITTING | 0.45 | 0.50 | 0.15 | 0.70 | – | – |
| PREGNANT*DAYS | 1.01 | 0.42 | 1.20 | 0.30 | – | – |
| QUITTING*DAYS | 0.92 | 0.49 | 1.43 | 0.19 | 2.18 | 0.359* |
| PREGNANT*QUITTING*DAYS | 1.19 | 0.30 | 0.46 | 0.86 | – | – |
© 2009 by the authors; licensee Molecular Diversity Preservation International, Basel, Switzerland. This article is an open-access article distributed under the terms and conditions of the Creative Commons Attribution license (http://creativecommons.org/licenses/by/3.0/).
Share and Cite
Ortendahl, M.; Uttermalm, A.; Simonsson, B.; Näsman, P.; Wallsten, T. Estimated Time for Occurrence of Smoking-Related Consequences among Pregnant and Non-Pregnant Women. Int. J. Environ. Res. Public Health 2009, 6, 1665-1675. https://doi.org/10.3390/ijerph6051665
Ortendahl M, Uttermalm A, Simonsson B, Näsman P, Wallsten T. Estimated Time for Occurrence of Smoking-Related Consequences among Pregnant and Non-Pregnant Women. International Journal of Environmental Research and Public Health. 2009; 6(5):1665-1675. https://doi.org/10.3390/ijerph6051665
Chicago/Turabian StyleOrtendahl, Monica, Alf Uttermalm, Bo Simonsson, Per Näsman, and Tuula Wallsten. 2009. "Estimated Time for Occurrence of Smoking-Related Consequences among Pregnant and Non-Pregnant Women" International Journal of Environmental Research and Public Health 6, no. 5: 1665-1675. https://doi.org/10.3390/ijerph6051665
APA StyleOrtendahl, M., Uttermalm, A., Simonsson, B., Näsman, P., & Wallsten, T. (2009). Estimated Time for Occurrence of Smoking-Related Consequences among Pregnant and Non-Pregnant Women. International Journal of Environmental Research and Public Health, 6(5), 1665-1675. https://doi.org/10.3390/ijerph6051665




