1. Introduction
Communicating risk during disasters is always a significant challenge for public health researchers, policymakers, and practitioners. For researchers, understanding how people perceive risk requires analyzing the many factors that shape these perceptions. These factors include resistance to pharmaceutical interventions (e.g., vaccines), the spread of misinformation, cultural influences, health literacy levels, and alternative worldviews [
1,
2]. Policymakers and organizations face a similar challenge. They must establish clear communication channels, provide accurate and timely recommendations, maintain public trust, navigate evolving media landscapes, and craft effective risk messages [
3]. Meanwhile, practitioners must quickly and clearly convey complex information to audiences who are encountering the risk and uncertainty [
4].
These challenges highlight the difficulty of building community resilience during pandemics and encouraging preventive behaviors like handwashing and mask-wearing. Since public health recommendations rely on persuasion rather than mandates, communicators must use theory and real-time assessment to guide their messaging [
5]. Theories give communicators a framework to work from, helping them figure out what to say and how to say it [
6]. At the same time, each pandemic presents unique challenges. During the 2004 Severe Acute Respiratory Syndrome (SARS) outbreak, the demand for information far outpaced its availability [
7]. The 2009 H1N1 pandemic saw a surge in rumors, which negatively affected trust in health authorities, as unclear messaging left room for speculation [
1]. The rise of social media further complicated risk communication during COVID-19, amplifying misinformation and making it harder to control the narrative [
8]. COVID-19 posed new challenges for health communicators, especially in early 2020. A perceived lack of government control fueled public anxiety, leading some to act against their own interests [
9]. Objections to guidelines adherence occurred in countries such as the United Kingdom and Canada, the anti-vaccine movement regained momentum, and disparities in adherence to preventive measures persisted [
10,
11].
Pandemics typically begin with uncertainty, limited evidence on intervention effectiveness, and the absence of a vaccine or treatment [
12]. In these early stages, health communicators must work with incomplete data to promote non-pharmaceutical interventions (NPIs) and curb disease spread. Effective communication is crucial, and a conceptual model can provide public health professionals with a structured approach to risk messaging at the onset of a pandemic. This paper provides a conceptual model to explain the decision-making processes behind recommending non-pharmaceutical interventions (NPIs) during pandemics. By critically evaluating key risk communication theories and incorporating lessons from COVID-19, this model provides a structured framework for public health professionals to enhance messaging strategies in future health crises.
2. Methods
To explore how risk is communicated during pandemics, this study draws on Jabareen’s conceptual framework analysis, which is rooted in grounded theory [
13]. This approach is designed to identify, develop, and connect key concepts that collectively form a theoretical framework for understanding a phenomenon. Unlike a mere collection of related concepts, a conceptual framework is “a network, or a plane, of interlinked concepts that together provide a comprehensive understanding of a phenomenon or phenomena [
13]”. Because the communication landscape shifts during a pandemic, this flexible approach is well-suited for analyzing how messaging evolves over time.
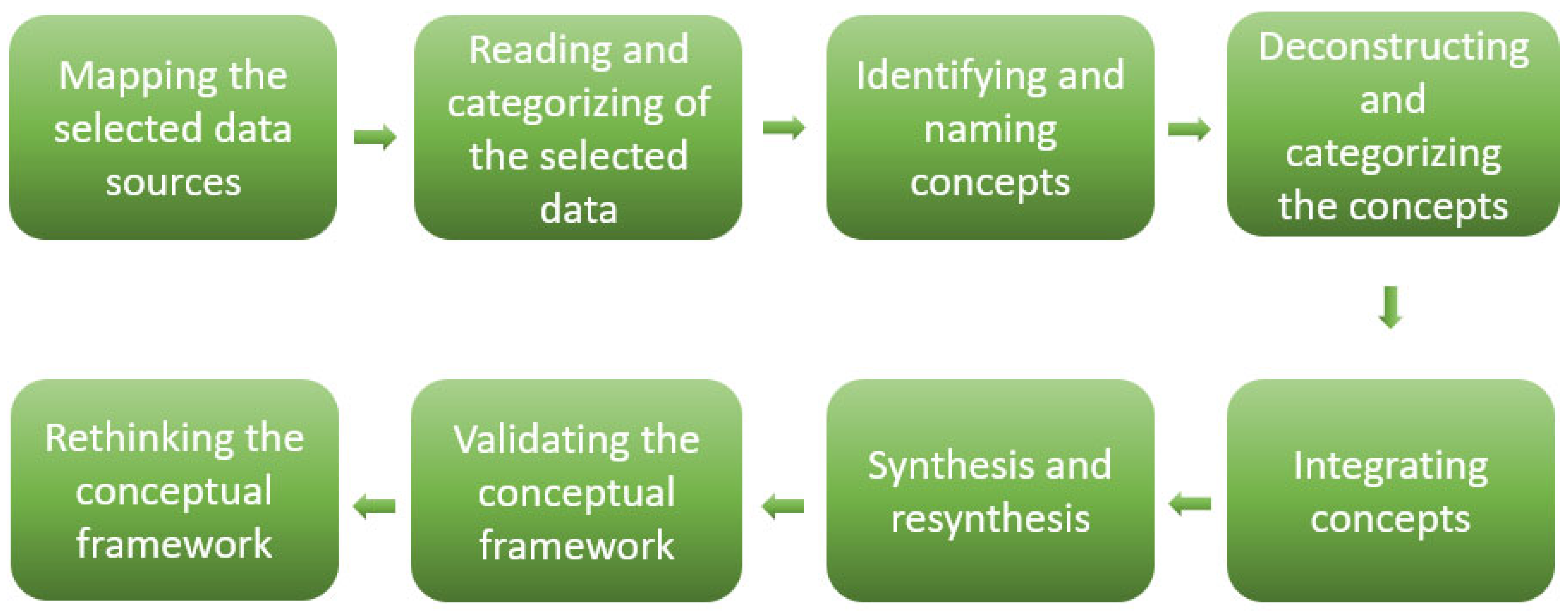
Jabareen’s conceptual framework analysis consists of eight phases: (1) mapping data sources from multiple disciplines, (2) conducting a literature review and categorizing data, (3) identifying and labeling relevant concepts, (4) deconstructing and organizing these concepts, (5) integrating them into a coherent structure, (6) synthesizing and ensuring consistency, (7) validating the framework, and (8) refining the framework as needed [
12]. To better align with the current study’s objectives, some of these phases were condensed during analysis [
Figure 1].
Each concept within the framework is examined in terms of its distinct characteristics, assumptions, limitations, and role in shaping the broader understanding of risk communication. The framework development process involves a comprehensive review and categorization of literature spanning the psychological, environmental, and social dimensions of risk communication. To build a strong multidisciplinary base, the framework incorporates literature from fields like public health, psychology, and communication studies.
2.1. Phases 1 and 2: Mapping and Categorizing Selected Data Sources—Theoretical Background
The first stages of this study involved reviewing and categorizing multidisciplinary literature to construct a conceptual framework for pandemic risk communication [
14]. This framework is grounded in three key theoretical approaches that inform the communication of non-pharmaceutical interventions (NPIs) during pandemics. The first approach is the Crisis and Emergency Risk Communication (CERC) model, developed by the CDC, which provides a structured communication strategy applicable to all phases of a pandemic. The second approach is the Social Amplification of Risk Perception Framework (SARF), which highlights how media strategies shape public risk perception and influence communication effectiveness. The third approach is Social Cognitive Theory (SCT), which examines the reciprocal relationship between individuals and their environment, emphasizing community participation as a fundamental motivator for adopting preventive behaviors. Together, these theories build a more complete picture of how pandemic risk is communicated, each adding different insights on behavior, messaging, and perception.
2.1.1. Phases of Crisis and Emergency Risk Communication
Promoting time-sensitive behaviors such as NPIs requires a well-structured communication strategy that is responsive to the different phases of a pandemic [
15]. CERC stands out from other crisis models because it is more adaptable and accounts for the many layers of a public health emergency. Unlike the Three-Stage Model of Crisis Communication and Turner’s Six-Stage Man-Made Disasters model, which are often criticized for being overly simplistic or lacking specificity, the CERC model offers a more adaptable structure that considers the evolving nature of pandemics [
16,
17]. The CERC model’s strength lies in its ability to account for multiple dimensions of a pandemic, including its physical, health, social, and psychological impacts [
15].
A common pitfall in pandemic preparedness is the assumption that future risk can be accurately anticipated based on past events. This assumption often leads to inadequate responses when confronted with unprecedented crises [
18]. Preparing communities for NPIs requires proactive engagement across all phases of a pandemic to enhance long-term resilience [
19]. The CERC model is based on two fundamental assumptions. First, it conceptualizes pandemics as complex, dynamic events influenced by multiple interacting factors rather than simple cause–effect relationships [
20]. Second, it acknowledges that pandemics are time-order and time-sensitive events shaped by how individuals experience and recall them [
21]. Personal narratives of the COVID-19 pandemic illustrate this phenomenon, with affected individuals often describing their experiences in ways that reflect deep psychological and social disruptions. One participant, for instance, recalled that “it felt like time stood still for many months while life was ‘on hold’ and every day was similar, with no punctuation by landmark events [
22] (p 1137)”. This time-oriented perception of pandemics underscores the necessity of adaptive communication strategies that resonate with the lived experiences of the public.
2.1.2. Socially Amplified Pandemic Risk Perception
The Social Amplification of Risk Framework (SARF) explains how risk perception is shaped by both social and individual processes [
23]. Since its initial conceptualization,
24 SARF has been widely applied to assess how public and individual responses to risk are influenced by various amplification channels, including social organizations, media platforms, and interpersonal interactions. The framework draws on classical communication theory, where amplification refers to the intensification or attenuation of a transmitted message, altering the amount of information retained from the original source [
24]. SARF posits that risk messages interact with psychological, social, and cultural factors, ultimately shaping behavior through a collectively constructed perception of risk [
23]. From this perspective, experiencing risk extends beyond the immediate physical threat of infection; it is also influenced by the subjective meanings and interpretations ascribed by individuals and communities [
25].
Risk communicators must recognize that the public’s perception of risk is not merely an inferior version of the expert’s objective assessment. Rather, SARF provides communicators with opportunities for intervention by identifying key points where risk perceptions can be influenced [
26]. The amplification or attenuation of risk occurs in two stages: the initial dissemination of information by official or unofficial sources, followed by the societal response, in which individuals translate risk messages into behavioral, economic, and social actions [
27]. Early messaging is affected by how much information is shared, how consistent and clear it is, and whether it feels exaggerated or emotionally charged [
25]. As individuals receive and process NPIs-related information, they become amplification stations, further shaping public perception through their behavioral responses and interpersonal communication [
28]. These amplification stations, whether individuals, groups, or institutions, play a critical role in constructing collective risk perceptions.
SARF also highlights the conditions under which social amplification is most pronounced. Risk perception tends to be amplified or heightened in situations characterized by high uncertainty and perceived personal threat, where individuals rely more on external information sources than on prior knowledge [
23,
29]. In the context of NPIs communication, SARF informs the understanding of how individuals cognitively and affectively process messages and develop stable beliefs regarding preventive behaviors. This framework accounts for the transformation of individual perceptions into shared social understandings of risk [
28].
A crucial component of SARF is its attention to how small groups such as marginalized and at-risk populations have a different risk perception than the general population. The inclusion of message targeting ensures that risk messages resonate with specific population segments based on shared characteristics such as race, socioeconomic status, and health vulnerabilities [
30]. Before implementing targeted messages, communicators must conduct audience segmentation to identify the most vulnerable groups and tailor messages to their needs and concerns [
31]. The COVID-19 pandemic demonstrated the importance of this approach, as African American populations in the United States experienced disproportionately higher fatality rates compared to White populations [
32]. This disparity cannot be attributed solely to race or access to healthcare but must also consider underlying health conditions such as hypertension, diabetes, and cardiovascular disease [
32,
33]. Effective NPIs communication requires a deliberate focus on these at-risk groups, ensuring that they receive comprehensive and contextually relevant information to guide their behavioral decisions.
At the same time, communicators need to be alert to the potential stigmatizing effects of targeted messaging. The 2009 H1N1 pandemic had the unfortunate moniker “swine flu”; U.S.-based agricultural labor, especially Mexican migrant or seasonal farmworkers, experienced significant discrimination from people who mistakenly attributed the cause of the pandemic to pork processing [
34]. Asians around the world experienced discrimination and violence during the COVID-19 pandemic due to its origination in China [
35,
36].
2.1.3. Social Cognitive Influences on NPIs Behavior
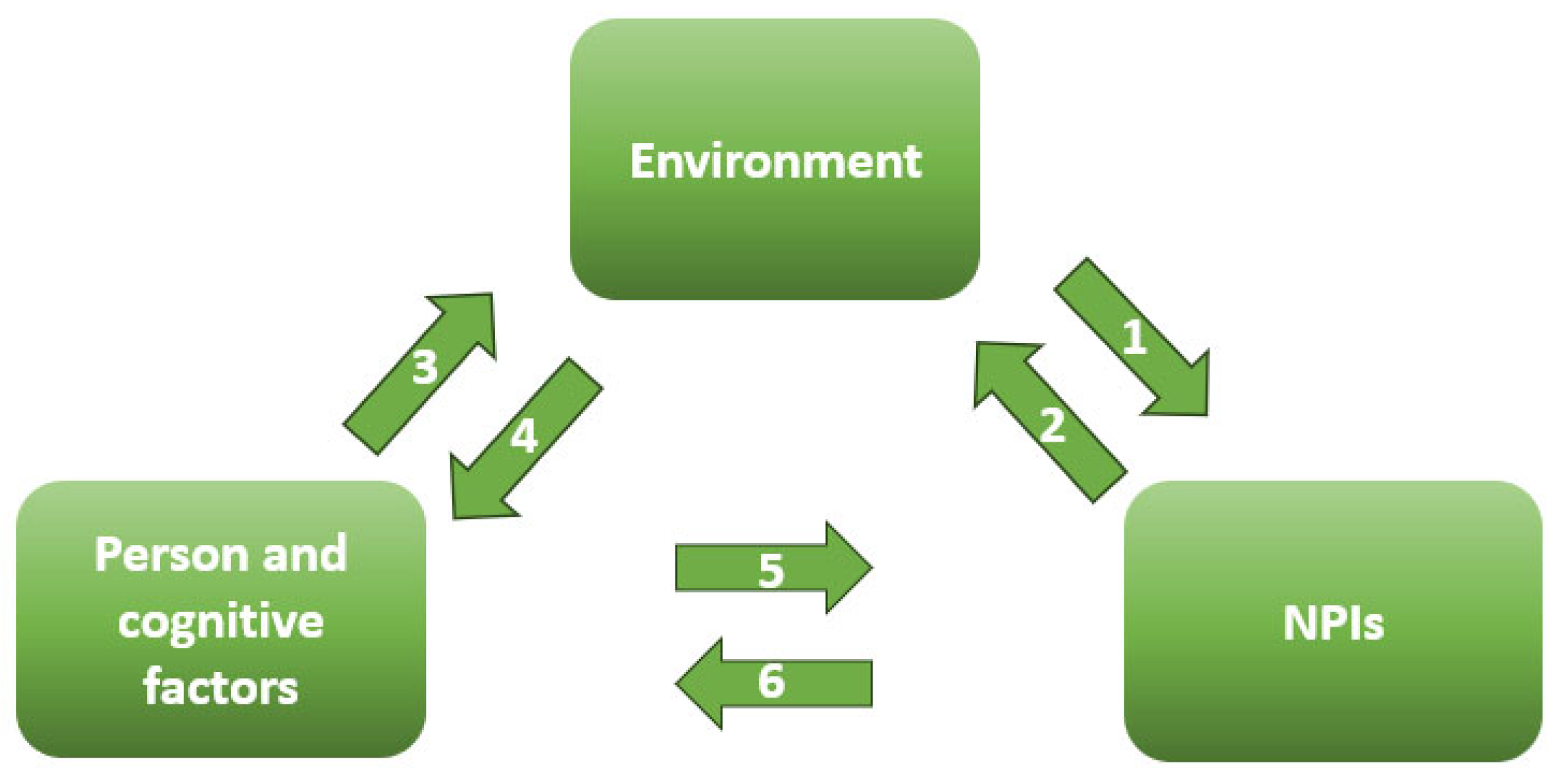
Social Cognitive Theory (SCT) plays a critical role in this framework by explaining the triadic reciprocal determinism that shapes NPIs adoption. This dynamic process involves the interaction of behavior, environmental influences, and individual psychological processes [
37]. While CERC and SARF address the timing and cognitive mechanisms of risk communication, SCT provides insight into how personal and environmental factors interact to influence behavior [
Figure 2].
The interactions between Bandura’s triad show up in many forms, as behavior, thoughts, and environment keep influencing each other. The social, economic, and political context can prompt individuals to adopt NPIs, while personal behaviors, such as aligning with a political ideology, can shape the broader environment. Individuals also influence their sociocultural surroundings through shared beliefs and collective cognition. At the same time, environmental factors can alter cognitive attributes like self-efficacy, just as a person’s cognitive state governs their engagement with preventive behaviors. In turn, sustained adherence to NPIs can further influence one’s cognitive perceptions, creating a continuous feedback loop [
38]. Risk communication strategies primarily target personal and cognitive factors, aiming to drive changes in the other components of this triadic system [
39]. This framework positions the individual as the central focus of NPIs messaging. By improving knowledge, enhancing self-efficacy, and fostering positive outcome expectancies, pre-pandemic education and real-time messaging can strengthen public engagement with NPIs. Since self-efficacy is enhanced through vicarious learning and verbal persuasion, communicators can use role models and authoritative figures to reinforce NPIs adoption [
40,
41].
2.2. Phase 3: Identifying and Naming Concepts
In this phase, the theoretical models previously discussed were examined in greater depth through an extensive review of relevant literature. Once their relevance to pandemic mitigation was established, the next step involved identifying specific concepts that influence health communication during pandemics. Using CERC as a base, we adopted its phase structure to match how messaging around NPIs changes throughout a pandemic [
42] [
Table 1].
To effectively promote NPIs, health communicators must understand not only how individuals receive and interpret messages but also how they act as amplification or attenuating points within their social networks. The Social Amplification of Risk Framework (SARF) serves here as a conceptual lens through which these amplification processes are understood. We adopt and adapt the steps outlined by Renn et al. [
28] to describe how individuals process information and how these insights can be applied to the targeted communication of NPIs among specific subgroups [
Table 2].
2.3. Phases 4 and 5: Deconstructing, Categorizing, and Integrating the Concepts
Building on the concepts identified in the previous phase, this step involved organizing and integrating them into a unified framework. Each concept was categorized according to its ontological, epistemological, or methodological role within the overall structure [
13]. Certain concepts, such as self-efficacy, were found to be central across all three theoretical models. These shared concepts were defined and positioned within the conceptual framework according to their distinct functions and theoretical contributions [
Table 3].
2.4. Phase 6: Synthesizing, Re-Synthesizing, and Ensuring Coherence
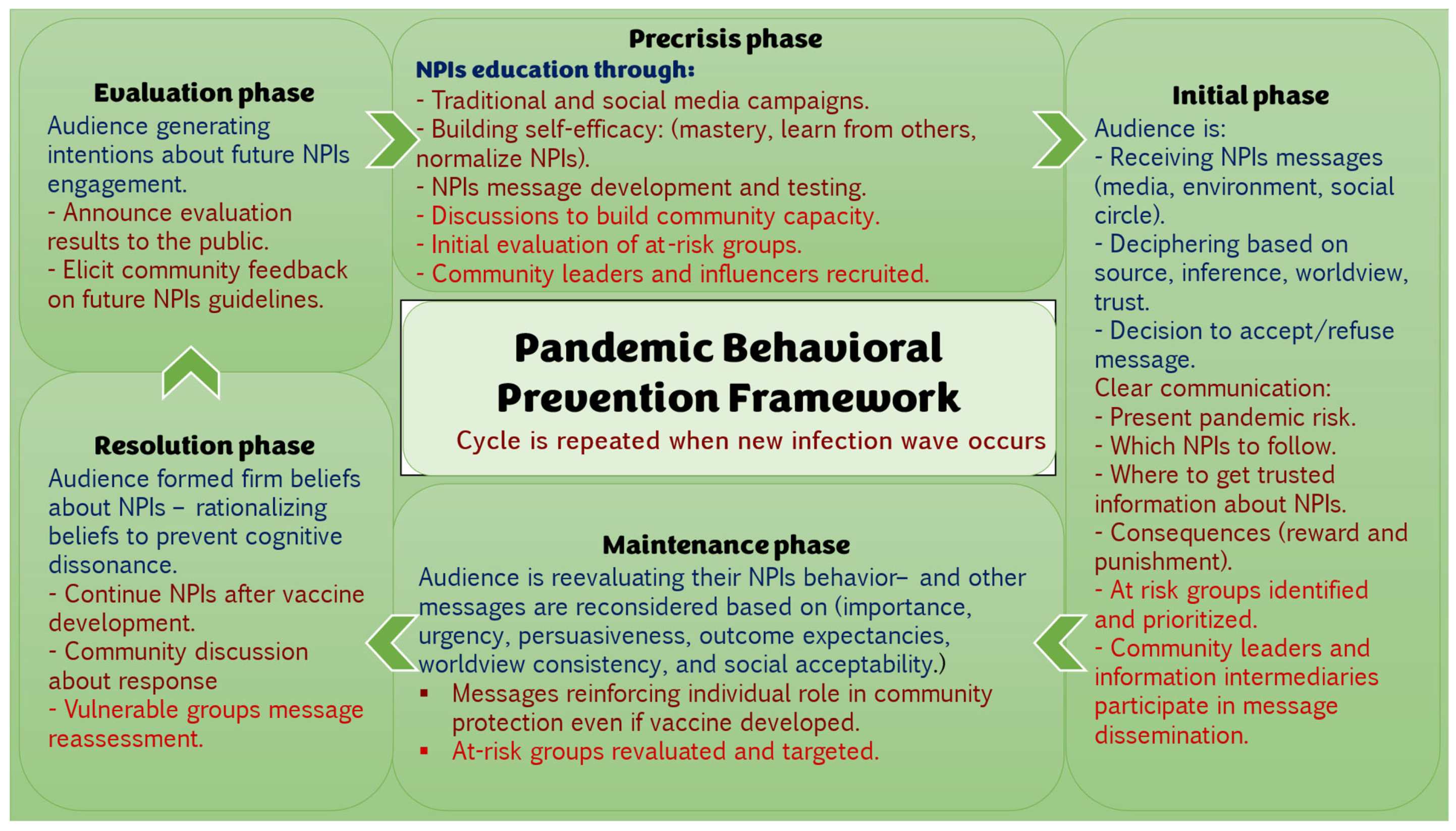
This stage involved synthesizing the conceptual elements into a coherent whole. To ensure the framework coherence, the different concepts were adjusted and aligned more tightly. The final framework segments NPIs communication into five phases, each marked by specific messaging strategies and expected audience behaviors. The framework centers on vulnerable populations, positioning them as a core focus of pandemic communication efforts and emphasizing their role in determining the success of public health interventions.
2.5. Phases 7 and 8: Validating and Rethinking the Conceptual Framework
In the final phases, the PBPF undergoes preliminary validation through evaluation by public health practitioners unaffiliated with its development. The goal of these evaluations is to see if the framework holds together, covers the key areas, and makes sense in real-world settings. As part of this process, we plan to present the framework to larger audiences, including at academic conferences and scientific meetings. Open-ended feedback will be solicited regarding its feasibility, utility, and areas for refinement. This input will guide future iterations of the framework and support its continued development.
3. Results
The
Pandemic Behavioral Prevention Framework is designed to address all layers of an infectious disease crisis by structuring the response into five distinct phases, shaping appropriate and socially accepted risk perceptions, and prioritizing the most vulnerable populations. An integral part of the success of this framework is the recruitment of credible, trustworthy, communicators; these are the leaders of the community, the local public health agency team, and local gatekeepers. Locality here is important; the local public health agency is often the most informed entity of the community needs, and their strong ties to the public should be in-place [
Figure 3].
In a future pandemic, public health teams could start by using familiar voices and social media to help people understand and accept protective behaviors like mask-wearing and handwashing. As the situation unfolds, clear and trustworthy messages would guide people on what to do, why it matters, and where to obtain reliable information. Over time, as fatigue sets in, reminders would help people stay motivated, especially those at higher risk. When vaccines or treatments become available, the focus would shift to addressing concerns and encouraging informed decisions. Finally, listening to the public’s experiences and feedback would help improve future responses. This step-by-step approach keeps communication grounded, responsive, and people-centered through every phase of the crisis.
4. Discussion—Lessons Learned
The Pandemic Behavioral Prevention Framework is designed with an awareness of how audiences process information, ensuring that communication efforts align with individuals’ cognitive, affective, and behavioral responses at different pandemic phases. For example, during the maintenance phase (e.g., past the peak of the epidemic curve), health communication is strategically directed to reinforce continued adherence to NPIs. Additionally, the framework prioritizes identifying and targeting vulnerable populations as a fundamental component of effective pandemic communication. The proposed framework tries to fill in the gaps that past pandemic messaging efforts often missed.
4.1. Integrating Risk and Emergency Communication with Health Communication
During infectious disease outbreaks, public health organizations rely primarily on two established frameworks: the Crisis and Emergency Risk Communication (CERC) model developed by the CDC and the Outbreak Communication Guidelines established by the WHO [
44]. These models were designed to manage the urgency, uncertainty, and time constraints that define health crises [
15]. Their relevance is evident when considering the crises that shaped their development, such as the 2001 World Trade Center attacks and the anthrax bioterrorism incidents [
45]. However, pandemics pose distinct challenges that go beyond isolated bioterrorism events, as they are ongoing, unpredictable, and spread rapidly across global populations [
45].
Existing risk and emergency communication frameworks are well-suited for the early stages of an outbreak, when containment efforts focus on minimizing harm at the community level. However, these models are less effective in managing the prolonged and unpredictable nature of pandemics [
46]. The COVID-19 pandemic highlighted the limitations of traditional crisis communication approaches, as the virus continuously mutated, altered transmission patterns, and created varying degrees of disease severity across different regions and timeframes [
47]. To close that gap, the PBPF brings in communication strategies that begin even before a crisis starts, aiming to build up public resilience ahead of time. Establishing behavioral norms such as proper cough etiquette, hand hygiene, and acceptance of NPIs before a crisis emerges can enhance public responsiveness and preparedness during a pandemic [
46]. Post-pandemic communications should highlight evidence that reinforces the effectiveness of the promoted behavior.
4.2. Utilizing Effective Communication Channels
As pandemics spread rapidly, communication efforts must leverage fast and adaptive channels. The 2009 H1N1 pandemic was the first to unfold with widespread global access to the Internet, revealing both the potential and challenges of online communication [
48]. However, public health communicators struggled to adapt to the Internet’s disruption of traditional sender–receiver communication models. The emergence of blogs, social media, and digital platforms removed the clear line between expert-driven communication and user-generated content, challenging the authority of public health messaging [
49]. The COVID-19 pandemic further exacerbated these challenges, as social media became the dominant space where individuals received, transmitted, and discussed pandemic-related information [
50].
Effective pandemic communication must take place on platforms where the public is already engaging. Due to the widespread connectivity, an infodemic took off and often spread faster than official health advice could keep up [
50]. Additionally, the blurred boundaries between health professionals’ personal and professional identities have created a disconnect between expert opinion and public perception [
51]. The
Pandemic Behavioral Prevention Framework (PBPF) emphasizes the need to fully integrate widely used digital communication platforms into risk messaging strategies to enhance reach and effectiveness.
4.3. Building Trust Before It Is Compromised
Building trust is a core objective of risk communication. Both the CDC and WHO recognize it as the foundation of effective public health messaging [
15,
44]. Trust is often regarded as the most valuable asset in a crisis; once lost, efforts to persuade the public to adopt preventive behaviors become significantly more difficult [
52]. However, trust cannot be built spontaneously during an emergency; it is largely shaped by society’s pre-existing confidence in institutions and leadership [
53].
In modern societies, public trust in policymakers and governmental institutions has been steadily declining, leading to what some describe as post-trust societies [
53,
54]. A failure to establish trust before a crisis undermines public confidence in official risk communication efforts, as seen during COVID-19, where inconsistent messaging and political divisions heightened public skepticism [
55]. Trust is built through objectivity, openness, honesty, competency, fairness, and consistency, all of which must be demonstrated in long-term public health communication strategies [
56]. The
Pandemic Behavioral Prevention Framework supports pre- and post-crisis trust-building through education and calls for transparent, clear messaging throughout all pandemic phases. Political environments further complicate trust-building efforts. How well a country manages a pandemic often depends on its political stability, leadership systems, and how its policies are put into action [
57]. While this study focuses on individual behaviors rather than policy reforms, it acknowledges the political dynamics that shape public engagement with NPIs.
4.4. Limiting the Consequences of Poor Responses for Vulnerable Populations
As with previous pandemics, COVID-19 disproportionately affected the most vulnerable populations [
58]. The pandemic exacerbated existing social, economic, and health inequities, placing marginalized communities at greater risk of severe illness and mortality [
58]. These disparities transcended national borders, affecting both high-income and low-income countries, highlighting the universal nature of pandemic-related vulnerabilities [
59].
The burden of pandemic response should not fall solely on at-risk individuals. Unlike other health crises that require access to specialized medical care or financial resources, NPIs involve behavioral changes with minimal material barriers. Addressing social determinants of health (SDOH) in pandemic response efforts is critical for ensuring equitable health outcomes [
60]. Effective communication is a key part of pandemic response, as it helps achieve satisfactory levels of testing, screening, and following safety guidelines [
60]. Health systems traditionally focus on structural factors such as healthcare access, but risk communication must be prioritized to prevent increasing health disparities [
61]. The
Pandemic Behavioral Prevention Framework underscores the importance of targeting underserved populations with tailored risk messages to mitigate the disproportionate impact of pandemics.
5. Strengths and Limitations
This study introduces a flexible grounded theory approach to develop a conceptual framework for NPIs communication in complex pandemic settings. A key strength of the PBPF is its focus on tailored messaging for vulnerable populations. While not yet tested in practice, this framework creates opportunities for future application, validation, and refinement through empirical studies and expert feedback, enhancing its relevance and impact in real-world public health contexts.
6. Conclusions
This paper integrates insights from multiple disciplines to enhance understanding of how to motivate individuals to adopt and maintain NPIs during a pandemic. The Pandemic Behavioral Prevention Framework provides a structured approach that incorporates how individuals process risk communication and interact with their environment across all pandemic phases. By equipping health communicators with a flexible and applicable tool, this framework offers a practical method for addressing the unpredictable nature of pandemics. Future research should test the framework in real-world applications through experimental studies to assess its impact on public adherence to NPIs.
Author Contributions
Conceptualization, A.A. and A.S.L.; methodology, A.A.; software, A.A.; validation, A.A. and A.S.L.; formal analysis, A.A.; investigation, A.A.; resources, A.A. and A.S.L.; data curation, A.A.; writing—original draft preparation, A.A.; writing—review and editing, A.A. and A.S.L.; visualization, A.A.; supervision, A.S.L.; project administration, A.A.; All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Barrelet, C.; Bourrier, M.; Burton-Jeangros, C.; Schindler, M. Unresolved issues in risk communication research: The case of the H1N1 pandemic (2009–2011). Influenza Other Respir. Viruses 2013, 7 (Suppl. 2), 114–119. [Google Scholar] [CrossRef]
- Jackson, D.N.; Trivedi, N.; Baur, C. Re-Prioritizing Digital Health and Health Literacy in Healthy People 2030 to Affect Health Equity. Health Commun. 2021, 36, 1155–1162. [Google Scholar] [CrossRef]
- Berg, S.H.; O’hara, J.K.; Shortt, M.T.; Thune, H.; Brønnick, K.K.; Lungu, D.A.; Røislien, J.; Wiig, S. Health authorities’ health risk communication with the public during pandemics: A rapid scoping review. BMC Public Health 2021, 21, 1401. [Google Scholar] [CrossRef] [PubMed]
- Chess, C.; Clarke, L. Facilitation of risk communication during the anthrax attacks of 2001: The organizational backstory. Am. J. Public Health 2007, 97, 1578–1583. [Google Scholar] [CrossRef]
- Utych, S.M. Messaging Mask Wearing During the COVID-19 Crisis: Ideological Differences. J. Exp. Political Sci. 2021, 8, 91–101. [Google Scholar] [CrossRef]
- Bartholomew, L.K.; Mullen, P.D. Five roles for using theory and evidence in the design and testing of behavior change interventions. J. Public Health Dent. 2011, 71 (Suppl. 1), S20–S33. [Google Scholar] [CrossRef]
- Arguin, P.M.; Navin, A.W.; Steele, S.F.; Weld, L.H.; Kozarsky, P.E. Health communication during SARS. Emerg. Infect. Dis. 2004, 10, 377–380. [Google Scholar] [CrossRef]
- Malecki, K.M.C.; Keating, J.A.; Safdar, N. Crisis Communication and Public Perception of COVID-19 Risk in the Era of Social Media. Clin. Infect. Dis. 2021, 72, 697–702. [Google Scholar] [CrossRef]
- Cheung, A.T.M.; Parent, B. Mistrust and inconsistency during COVID-19: Considerations for resource allocation guidelines that prioritise healthcare workers. J. Med. Ethics 2021, 47, 73–77. [Google Scholar] [CrossRef]
- Martin, S.; Vanderslott, S. “Any idea how fast ‘It’s just a mask!’ can turn into ‘It’s just a vaccine!’”: From mask mandates to vaccine mandates during the COVID-19 pandemic. Vaccine 2022, 40, 7488–7499. [Google Scholar] [CrossRef]
- Weiss, B.D.; Paasche-Orlow, M.K. Disparities in Adherence to COVID-19 Public Health Recommendations. Health Lit. Res. Pract. 2020, 4, e171–e173. [Google Scholar] [CrossRef]
- Carvalho, T.; Krammer, F.; Iwasaki, A. The first 12 months of COVID-19: A timeline of immunological insights. Nat. Rev. Immunol. 2021, 21, 245–256. [Google Scholar] [CrossRef] [PubMed]
- Jabareen, Y. Building a Conceptual Framework: Philosophy, Definitions, and Procedure. Int. J. Qual. Methods 2009, 8, 49–62. [Google Scholar] [CrossRef]
- Jabareen, Y. Towards a Sustainability Education Framework: Challenges, Concepts and Strategies—The Contribution from Urban Planning Perspectives. Sustainability 2012, 4, 2247–2269. [Google Scholar] [CrossRef]
- Seeger, M.; Reynolds, B.; Day, A. Crisis and Emergency Risk Communication: Past, present, and future. In Crisis and Emergency Risk Communication; Frandsen, F., Johansen, W., Eds.; De Gruyter Mouton: Berlin, Germany; Boston, MA, USA, 2020; pp. 401–418. [Google Scholar] [CrossRef]
- Bills, K.; Costello, L.; Cattani, M. Barry Turner: The Under-Acknowledged Safety Pioneer. Safety 2023, 9, 68. [Google Scholar] [CrossRef]
- Pedersen, C.L.; Ritter, T.; Di Benedetto, C.A. Managing through a crisis: Managerial implications for business-to-business firms. Ind. Mark. Manag. 2020, 88, 314–322. [Google Scholar] [CrossRef]
- Aven, T. The concept of antifragility and its implications for the practice of risk analysis. Risk Anal. 2015, 35, 476–483. [Google Scholar] [CrossRef]
- Marcassoli, A.; Leonardi, M.; Passavanti, M.; De Angelis, V.; Bentivegna, E.; Martelletti, P.; Raggi, A. Lessons Learned from the Lessons Learned in Public Health during the First Years of COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2023, 20, 1785. [Google Scholar] [CrossRef]
- Matthew, W.S.; Sellnow, T.L.; Ulmer, R.R. Communication, Organization, and Crisis. In Communication Yearbook; Routledge: Abingdon-on-Thames, UK, 2012; pp. 231–275. [Google Scholar]
- Veil, S.; Reynolds, B.; Sellnow, T.L.; Seeger, M.W. CERC as a theoretical framework for research and practice. Health Promot. Pract. 2008, 9 (Suppl. 4), 26S–34S. [Google Scholar] [CrossRef]
- Velasco, P.F.; Perroy, B.; Gurchani, U.; Casati, R. Lost in pandemic time: A phenomenological analysis of temporal disorientation during the COVID-19 crisis. Phenomenol. Cogn. Sci. 2023, 22, 1121–1144. [Google Scholar] [CrossRef]
- Kasperson, J.X.; Kasperson, R.E.; Pidgeon, N.; Slovic, P. The Social Amplification of Risk: Assessing 15 Years of Research and Theory. Soc. Contours Risk 2012, 27, 202–229. [Google Scholar]
- Kasperson, R.E.; Renn, O.; Slovic, P.; Brown, H.S.; Emel, J.; Goble, R.; Kasperson, J.X.; Ratick, S. The social amplification of risk: A conceptual framework. Risk Anal. 1988, 8, 177–187. [Google Scholar] [CrossRef]
- Hopfer, S.; Fields, E.J.; Lu, Y.; Ramakrishnan, G.; Grover, T.; Bai, Q.; Huang, Y.; Li, C.; Mark, G. The social amplification and attenuation of COVID-19 risk perception shaping mask wearing behavior: A longitudinal twitter analysis. PLoS ONE 2021, 16, e0257428. [Google Scholar] [CrossRef]
- Kasperson, R.E.; Webler, T.; Ram, B.; Sutton, J. The social amplification of risk framework: New perspectives. Risk Anal. 2022, 42, 1367–1380. [Google Scholar] [CrossRef]
- Pidgeon, N.; Kasperson, R.E.; Slovic, P. (Eds.) The Social Amplification of Risk; Cambridge University Press: Cambridge, UK, 2003. [Google Scholar]
- Renn, O.; Burns, W.J.; Kasperson, J.X.; Kasperson, R.E.; Slovic, P. The social amplification of risk: Theoretical foundations and empirical applications. J. Soc. Issues 1992, 48, 137–160. [Google Scholar] [CrossRef]
- Slovic, P. Perception of risk. Science 1987, 236, 280–285. [Google Scholar] [CrossRef] [PubMed]
- Schiavo, R. Health Communication: From Theory to Practice; John Wiley & Sons: Hoboken, NJ, USA, 2013. [Google Scholar]
- Thompson, T.L.; Parrott, R.; Nussbaum, J.F. (Eds.) The Routledge Handbook of Health Communication, 2nd edTaylor & Francis: New York, NY, USA, 2022. [Google Scholar]
- Yancy, C.W. COVID-19 and African Americans. JAMA 2020, 323, 1891–1892. [Google Scholar] [CrossRef]
- Braveman, P.; Gottlieb, L. The social determinants of health: It’s time to consider the causes of the causes. Public Health Rep. 2014, 129 (Suppl. 2), 19–31. [Google Scholar] [CrossRef]
- Schoch-Spana, M.; Bouri, N.; Rambhia, K.J.; Norwood, A. Stigma, health disparities, and the 2009 H1N1 influenza pandemic: How to protect Latino farmworkers in future health emergencies. Biosecur. Bioterror. 2010, 8, 243–254. [Google Scholar] [CrossRef]
- Liu, L.S.; Jia, X.; Zhu, A.; Ran, G.J.; Siegert, R.; French, N.; Johnston, D. Stigmatising and Racialising COVID-19: Asian People’s Experience in New Zealand. J. Racial Ethn. Health Disparities 2023, 10, 2704–2717. [Google Scholar] [CrossRef]
- Misra, S.; Le, P.D.; Goldmann, E.; Yang, L.H. Psychological impact of anti-Asian stigma due to the COVID-19 pandemic: A call for research, practice, and policy responses. Psychol. Trauma. 2020, 12, 461–464. [Google Scholar] [CrossRef]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef]
- DiClemente, R.J.; Salazar, L.F.; Crosby, R.A. Health Behavior Theory for Public Health: Principles, Foundations, and Applications; Jones & Bartlett Publishers: Burlington, MA, USA, 2013. [Google Scholar]
- Schwarzer, L. Social Cognitive Theory. In Predicting Health Behaviour, 2nd ed.; Conner, M., Norman, P., Eds.; Open University Press: Buckingham, UK, 2005; pp. 127–169. [Google Scholar]
- Schunk, D.H. Social cognitive theory. In APA Educational Psychology Handbook; Harris, K.R., Graham, S., Urdan, T., McCormick, C.B., Sinatra, G.M., Sweller, J., Eds.; Theories, Constructs, and Critical Issues; American Psychological Association: Washington, DC, USA, 2012; Volume 1, pp. 101–123. [Google Scholar]
- Hagger, M.S.; Hamilton, K. Social cognition theories and behavior change in COVID-19: A conceptual review. Behav. Res. Ther. 2022, 154, 104095. [Google Scholar] [CrossRef]
- Reynolds, B.; Seeger, W.M. Crisis and emergency risk communication as an integrative model. J. Health Commun. 2005, 10, 43–55, Erratum in J. Health Commun. 2007, 12, 313. [Google Scholar] [CrossRef] [PubMed]
- Zlatanović, L. Self-efficacy and health behaviour: Some implications for medical anthropology. Glas. Antropol. Drustva Srp. 2016, 51, 111–120. [Google Scholar] [CrossRef]
- World Health Organization. WHO Outbreak Communication Guidelines; World Health Organization: Geneva, Switzerland, 2005. [Google Scholar]
- Gostin, L.O.; Nuzzo, J.B. Twenty Years After the Anthrax Terrorist Attacks of 2001: Lessons Learned and Unlearned for the COVID-19 Response. JAMA 2021, 326, 2009–2010. [Google Scholar] [CrossRef]
- Khanna, R.C.; Cicinelli, M.V.; Gilbert, S.S.; Honavar, S.G.; Murthy, G.S.V. COVID-19 pandemic: Lessons learned and future directions. Indian. J. Ophthalmol. 2020, 68, 703–710. [Google Scholar] [CrossRef]
- Rahman, F.I.; Ether, S.A.; Islam, M.R. The “Delta Plus” COVID-19 variant has evolved to become the next potential variant of concern: Mutation history and measures of prevention. J. Basic. Clin. Physiol. Pharmacol. 2021, 33, 109–112. [Google Scholar] [CrossRef]
- Cloes, R.; Ahmad, A.; Reintjes, R. Risk communication during the 2009 influenza A (H1N1) pandemic: Stakeholder experiences from eight European countries. Disaster Med. Public. Health Prep. 2015, 9, 127–133. [Google Scholar] [CrossRef]
- Terry, K.; Yang, F.; Yao, Q.; Liu, C. The role of social media in public health crises caused by infectious disease: A scoping review. BMJ Glob. Health 2023, 8, e013515. [Google Scholar] [CrossRef]
- Vosoughi, S.; Roy, D.; Aral, S. The spread of true and false news online. Science 2018, 359, 1146–1151. [Google Scholar] [CrossRef]
- Topf, J.M.; Williams, P.N. COVID-19, Social Media, and the Role of the Public Physician. Blood Purif. 2021, 50, 595–601. [Google Scholar] [CrossRef] [PubMed]
- Betsch, C.; Wieler, L.H.; Habersaat, K.; COSMO Group. Monitoring behavioural insights related to COVID-19. Lancet 2020, 395, 1255–1256. [Google Scholar] [CrossRef] [PubMed]
- Bouder, F. Risk communication of vaccines: Challenges in the post-trust environment. Curr. Drug Saf. 2015, 10, 9–15. [Google Scholar] [CrossRef]
- Lofstedt, R.E. Risk Management in Post-Trust Societies; Routledge: Abingdon-on-Thames, UK, 2012. [Google Scholar]
- Jennings, W.; Stoker, G.; Valgarðsson, V.; Devine, D.; Gaskell, J. How trust, mistrust and distrust shape the governance of the COVID-19 crisis. J. Eur. Public Policy 2021, 28, 1174–1196. [Google Scholar] [CrossRef]
- Uslaner, E.M. (Ed.) The Oxford Handbook of Social and Political Trust; Oxford University Press: Oxford, UK, 2018. [Google Scholar]
- Kavanagh, M.M.; Singh, R. Democracy, Capacity, and Coercion in Pandemic Response: COVID-19 in Comparative Political Perspective. J. Health Polit. Policy Law 2020, 45, 997–1012. [Google Scholar] [CrossRef]
- da Silva Nunes, T.; Soliman, A.; Taguchi, K.; Matsoso, P.; Driece, R.A.; Tangcharoensathien, V. Addressing inequity: The world needs an ambitious Pandemic Accord. Lancet 2023, 402, 271–273. [Google Scholar] [CrossRef]
- Ismail, S.J.; Tunis, M.C.; Zhao, L.; Quach, C. Navigating inequities: A roadmap out of the pandemic. BMJ Glob. Health 2021, 6, e004087. [Google Scholar] [CrossRef]
- Goulbourne, T.; Yanovitzky, I. The Communication Infrastructure as a Social Determinant of Health: Implications for Health Policymaking and Practice. Milbank Q. 2021, 99, 24–40. [Google Scholar] [CrossRef]
- Yoo, W.; Hong, Y.; Oh, S.H. Communication inequalities in the COVID-19 pandemic: Socioeconomic differences and preventive behaviors in the United States and South Korea. BMC Public. Health 2023, 23, 1290. [Google Scholar] [CrossRef]
| Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).