Effectiveness of a Mind–Body Intervention at Improving Mental Health and Performance Among Career Firefighters
Abstract
1. Introduction
1.1. Exercise and Mental Health
1.2. Psychological Resilience and Mental Health
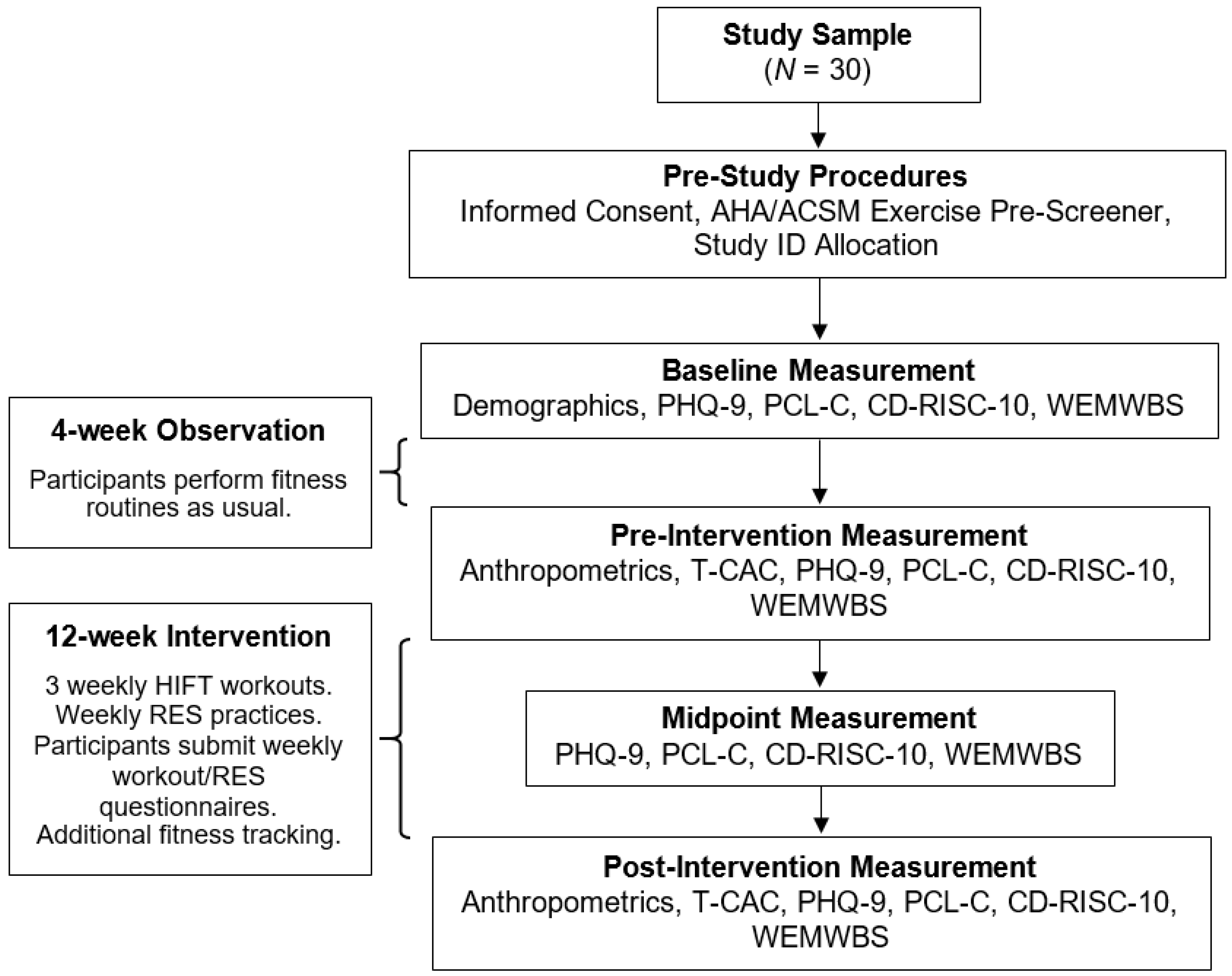
2. Materials and Methods
2.1. Participants and Exercise Pre-Screening
2.2. Pre- and Post-Intervention Procedures
2.3. Mental Health Outcome Measures
2.4. Intervention Protocols
2.5. Statistical Analyses
- Model 4 (AgeMC) controlled for participants’ mean-centered age at 39 years (M = 39.70 years, SD = 7.62, range = 23.00–57.00);
- Model 5 controlled for level of education, dichotomized into 0 (Some college but no degree [n = 2] or Associate degree [n = 13]) and 1 (Bachelor degree [n = 13] or Graduate degree [n = 2];
- Model 6 controlled for fire department rank, dichotomized into 0 (Firefighter [n = 8] or Engineer [n = 6]) and 1 (Captain [n = 10] or Battalion Chief [n = 6]);
- Model 7 (Years of serviceMC) controlled for years of service mean-centered at 15 (M = 15.43 years, SD = 8.27, range = 1.00–35.00);
- Model 8 controlled for participants’ combined race and ethnicity, dichotomized into 0 (Race: White [n = 1], Other [n = 1], Don’t know [n = 1], or Prefer not to say [n = 1]; Ethnicity: Hispanic [n = 3] or Prefer not to say [n = 1]) and 1 (Race: White [n = 26]; Ethnicity: Not Hispanic [n = 26]);
- Model 9 controlled for relationship status, dichotomized into 0 (Single [n = 3], In a relationship [n = 2], or Divorced [n = 1]) and 1 (Married [n = 24]);
- Model 10 controlled for participants’ biological sex as 0 (Male [n = 27]) and 1 (Female [n = 3]).
- Model 4 (Combined adherenceSTD) controlled for participants’ standardized combined adherence (see Tables S12–S15 for a description of variable standardization);
- Model 5 controlled for Combined adherenceSTD plus the Combined adherenceSTD × growth interaction;
- Model 6 controlled for Combined adherenceSTD, the Combined adherenceSTD × growth interaction, and additional fitness tracking variables (i.e., mean-centered additional weekly workouts, mean-centered additional weekly minutes of exercise, and mean-centered rating of perceived exertion [RPE] of additional workouts);
- Model 7 (HIFT adherenceSTD) controlled for participants’ standardized HIFT workout adherence;
- Model 8 controlled for HIFT adherenceSTD plus the HIFT adherenceSTD × growth interaction;
- Model 9 controlled for HIFT adherenceSTD, the HIFT adherenceSTD × growth interaction, and additional fitness tracking variables;
- Model 10 (RES adherenceSTD) controlled for participants’ standardized RES practice adherence;
- Model 11 controlled for RES adherenceSTD plus the RES adherenceSTD × growth interaction;
- Model 12 controlled for RES adherenceSTD, the RES adherenceSTD × growth interaction, and additional fitness tracking variables.
3. Results
3.1. Sample Characteristics
3.2. Anthropometric and Job-Task Performance Measurements
3.2.1. Group Differences Between Pre- and Post-Testing Samples
3.3. Intervention Adherence and Additional Fitness Tracking
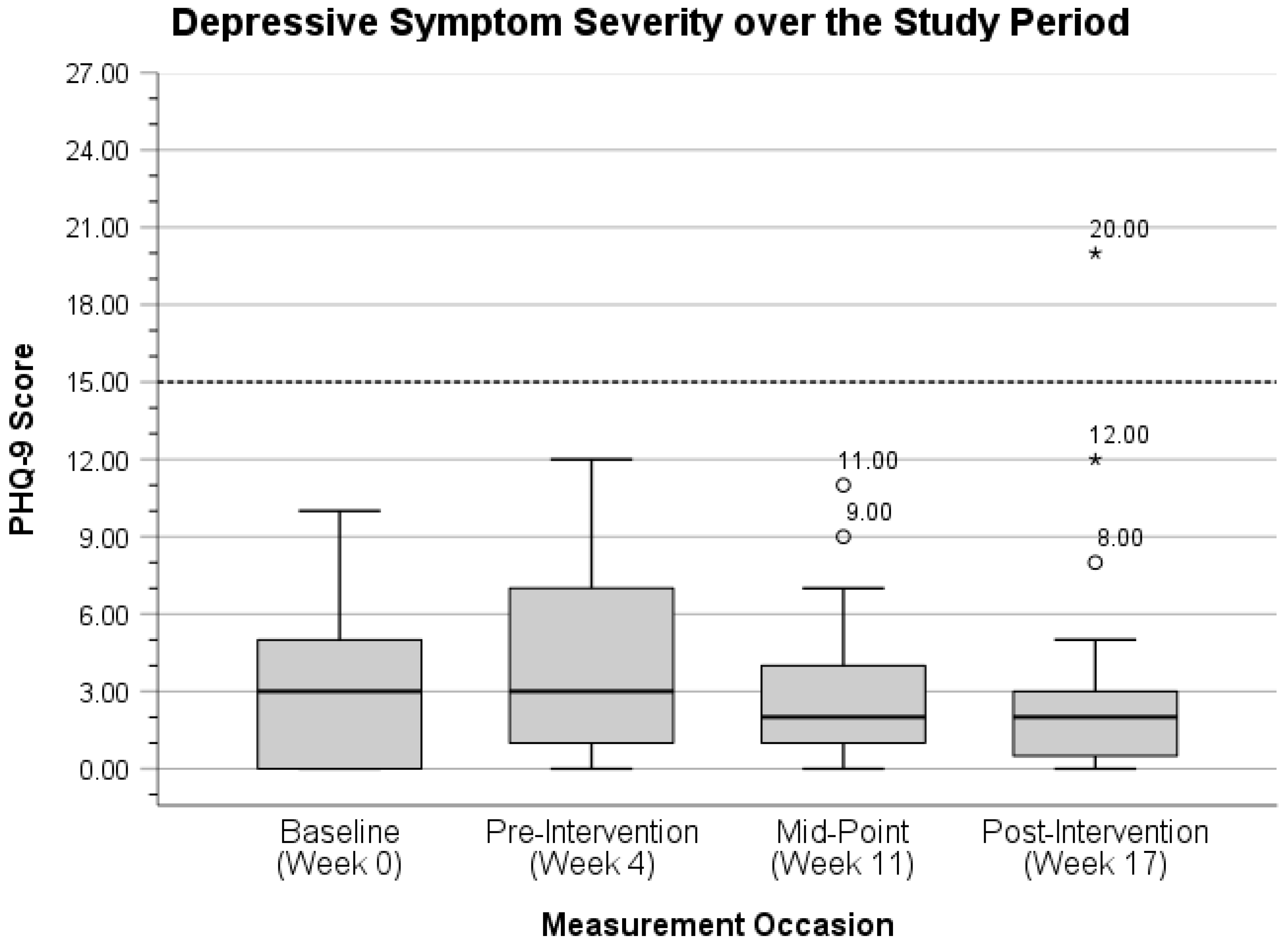
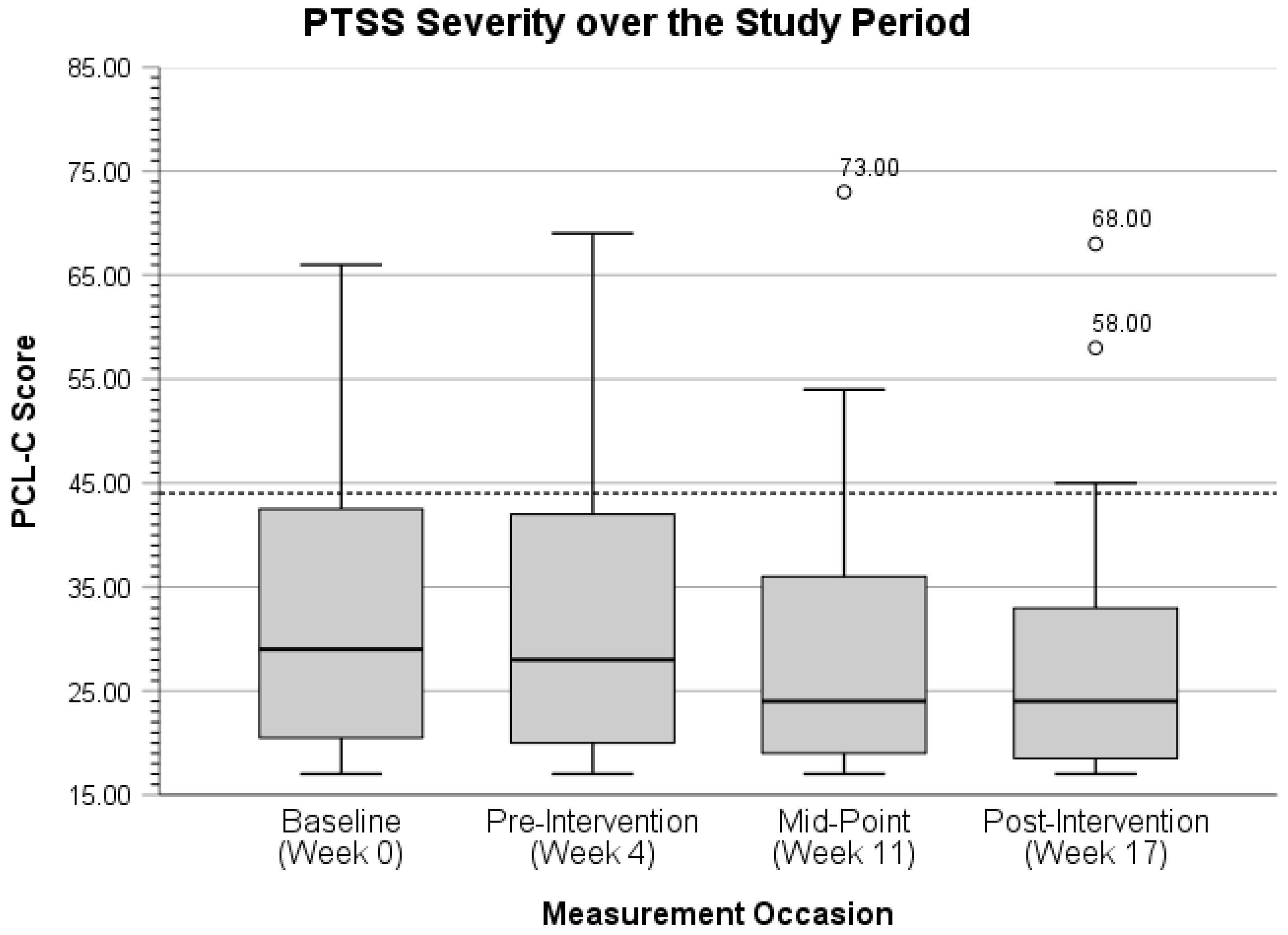
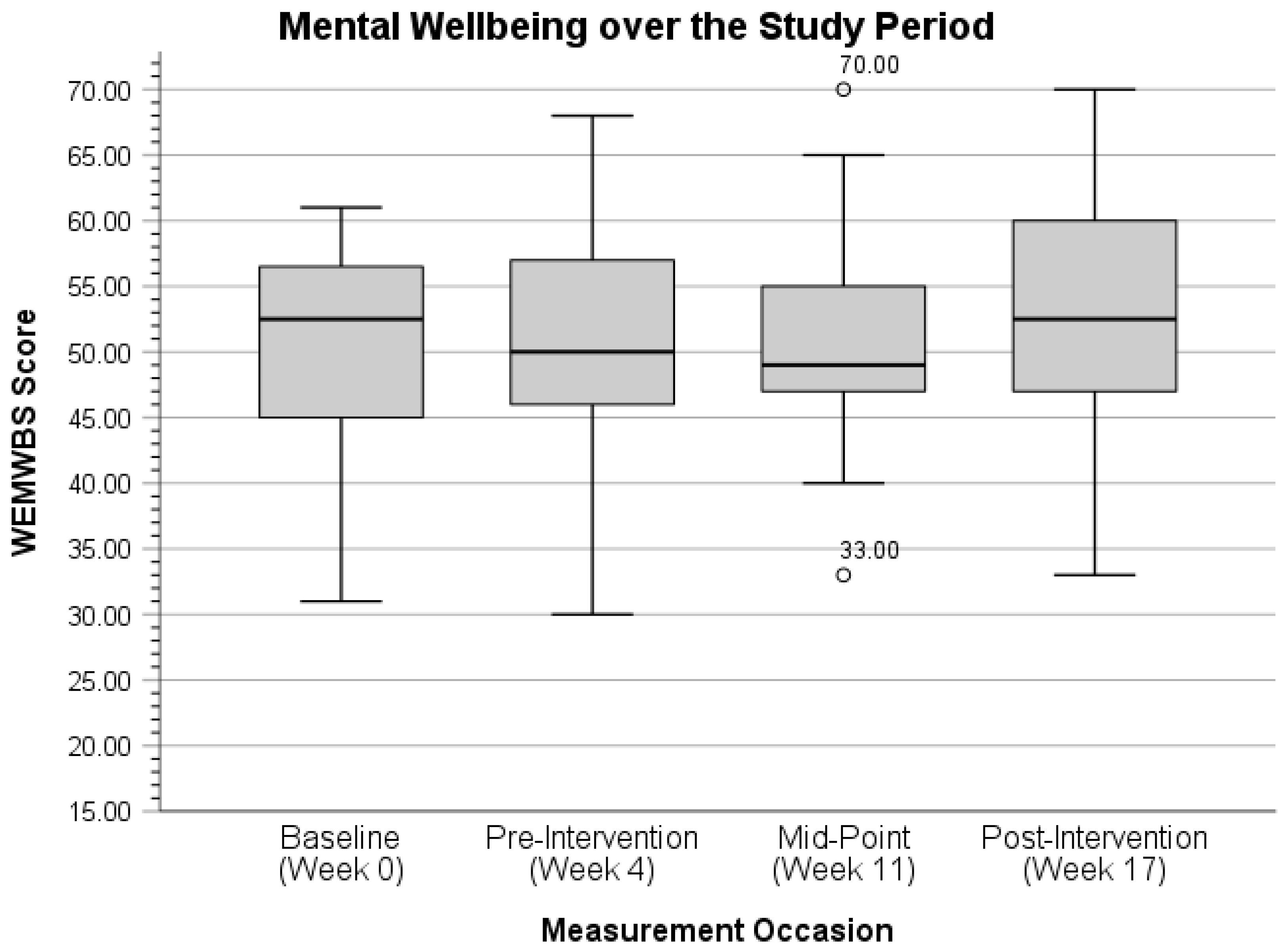
3.4. Mental Health Outcome Mean Values
3.5. Repeated-Measures T-Tests and Effect Sizes
3.6. Multilevel Modeling Results
3.6.1. Main Effects of Demographics on Mental Health Outcomes
3.6.2. Main Effects of Intervention Adherence and Additional Fitness Tracking on Anthropometrics and Job-Task Performance
3.6.3. Main Effects of Intervention Adherence and Additional Fitness Tracking on Mental Health Outcomes
3.7. Mental Health Outcome Measurement Distributions
3.8. Post Hoc Sample Size and Power Analyses Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Substance Abuse and Mental Health Services Administration. Disaster Technical Assistance Center Supplemental Research Bulletin First Responders: Behavioral Health Concerns, Emergency Response, and Trauma; Rockville, MD, 2018. Available online: https://www.samhsa.gov/sites/default/files/dtac/supplementalresearchbulletin-firstresponders-may2018.pdf (accessed on 7 April 2025).
- Walker, A.; McKune, A.; Ferguson, S.; Pyne, D.B.; Rattray, B. Chronic Occupational Exposures Can Influence the Rate of PTSD and Depressive Disorders in First Responders and Military Personnel. Extrem. Physiol. Med. 2016, 5, 8. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.C.; Vega, L.; Kohalmi, A.L.; Roth, J.C.; Howell, B.R.; Van Hasselt, V.B. Enhancing Mental Health Treatment for the Firefighter Population: Understanding Fire Culture, Treatment Barriers, Practice Implications, and Research Directions. Prof. Psychol. Res. Pract. 2020, 51, 304–311. [Google Scholar] [CrossRef]
- De Barros, V.V.; Fernandes Martins, L.; Saitz, R.; Rocha Bastos, R.; Mota Ronzani, T. Mental Health Conditions, Individual and Job Characteristics and Sleep Disturbances among Firefighters. J. Health Psychol. 2013, 18, 350–358. [Google Scholar] [CrossRef]
- Stanley, I.H.; Boffa, J.W.; Hom, M.A.; Kimbrel, N.A.; Joiner, T.E. Differences in Psychiatric Symptoms and Barriers to Mental Health Care between Volunteer and Career Firefighters. Psychiatry Res. 2017, 247, 236–242. [Google Scholar] [CrossRef] [PubMed]
- Gulliver, S.B.; Pennington, M.L.; Torres, V.A.; Steffen, L.E.; Mardikar, A.; Leto, F.; Ostiguy, W.; Zimering, R.T.; Kimbrel, N.A. Behavioral Health Programs in Fire Service: Surveying Access and Preferences. Psychol. Serv. 2019, 16, 340–345. [Google Scholar] [CrossRef]
- Stanley, I.H.; Hom, M.A.; Hagan, C.R.; Joiner, T.E. Career Prevalence and Correlates of Suicidal Thoughts and Behaviors among Firefighters. J. Affect. Disord. 2015, 187, 163–171. [Google Scholar] [CrossRef]
- Henderson, S.N.; van Hasselt, V.B.; LeDuc, T.J.; Couwels, J. Firefighter Suicide: Understanding Cultural Challenges for Mental Health Professionals. Prof. Psychol. Res. Pract. 2016, 47, 224–230. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, D.; Kim, J.; Jeon, K.; Sim, M. Duty-Related Trauma Exposure and Posttraumatic Stress Symptoms in Professional Firefighters. J. Trauma. Stress 2017, 30, 133–141. [Google Scholar] [CrossRef]
- Gulliver, S.B.; Zimering, R.T.; Knight, J.; Morissette, S.B.; Kamholz, B.W.; Pennington, M.L.; Dobani, F.; Carpenter, T.P.; Kimbrel, N.A.; Keane, T.M.; et al. A Prospective Study of Firefighters’ PTSD and Depression Symptoms: The First 3 Years of Service. Psychol. Trauma Theory, Res. Pract. Policy 2021, 13, 44–55. [Google Scholar] [CrossRef]
- Wolffe, T.A.M.; Robinson, A.; Clinton, A.; Turrell, L.; Stec, A.A. Mental Health of UK Firefighters. Sci. Rep. 2023, 13, 62. [Google Scholar] [CrossRef]
- Brudey, C.; Park, J.; Wiaderkiewicz, J.; Kobayashi, I.; Mellman, T.; Marvar, P.J. Autonomic and Inflammatory Consequences of Posttraumatic Stress Disorder and the Link to Cardiovascular Disease. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2015, 309, R315–R321. [Google Scholar] [CrossRef] [PubMed]
- Michopoulos, V.; Norrholm, S.D.; Jovanovic, T. Diagnostic Biomarkers for Posttraumatic Stress Disorder (PTSD): Promising Horizons from Translational Neuroscience Research. Biol. Psychol. 2015, 78, 344–353. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Blumenthal, J.A.; Babyak, M.A.; Moore, K.A.; Craighead, W.E.; Herman, S.; Khatri, P.; Waugh, R.; Napolitano, M.A.; Forman, L.M.; Appelbaum, M.; et al. Effects of Exercise Training on Older Patients with Major Depression. Arch. Intern. Med. 1999, 159, 2349–2356. [Google Scholar] [CrossRef] [PubMed]
- Brosse, A.L.; Sheets, E.S.; Lett, H.S.; Blumenthal, J.A. Exercise and the Treatment of Clinical Depression in Adults: Recent Findings and Future Directions. Sport. Med. 2002, 32, 741–760. [Google Scholar] [CrossRef]
- Stathopoulou, G.; Powers, M.B.; Berry, A.C.; Smits, J.A.J.; Otto, M.W. Exercise Interventions for Mental Health: A Quantitative and Qualitative Review. Clin. Psychol. Sci. Pract. 2006, 13, 179–193. [Google Scholar] [CrossRef]
- Rethorst, C.D.; Wipfli, B.M.; Landers, D.M. The Antidepressive Effects of Exercise: A Meta-Analysis of Randomized Trials. Sport. Med. 2009, 39, 491–511. [Google Scholar] [CrossRef]
- Stanton, R.; Reaburn, P. Exercise and the Treatment of Depression: A Review of the Exercise Program Variables. J. Sci. Med. Sport 2014, 17, 177–182. [Google Scholar] [CrossRef]
- Schuch, F.B.; Vancampfort, D.; Richards, J.; Rosenbaum, S.; Ward, P.B.; Stubbs, B. Exercise as a Treatment for Depression: A Meta-Analysis Adjusting for Publication Bias. J. Psychiatr. Res. 2016, 77, 42–51. [Google Scholar] [CrossRef]
- Schuch, F.B.; Deslandes, A.C.; Stubbs, B.; Gosmann, N.P.; da Silva, C.T.B.; de Almeida Fleck, M.P. Neurobiological Effects of Exercise on Major Depressive Disorder: A Systematic Review. Neurosci. Biobehav. Rev. 2016, 61, 1–11. [Google Scholar] [CrossRef]
- Blumenthal, J.A.; Smith, P.J.; Hoffman, B.M. Is Exercise a Viable Treatment for Depression? ACSM’s Health Fit. J. 2012, 16, 14–21. [Google Scholar] [CrossRef]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P. Quantity and Quality of Exercise for Developing and Maintaining Cardiorespiratory, Musculoskeletal, and Neuromotor Fitness in Apparently Healthy Adults: Guidance for Prescribing Exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Netz, Y. Is the Comparison between Exercise and Pharmacologic Treatment of Depression in the Clinical Practice Guideline of the American College of Physicians Evidence-Based? Front. Pharmacol. 2017, 8, 257. [Google Scholar] [CrossRef]
- Magyari, P.; Lite, R.; Killpatrick, M.W.; Schoffstall, J.E. (Eds.) ACSM’s Resources for the Exercise Physiologist, 2nd ed.; Wolters Kluwer: Philadelphia, PA, USA, 2018. [Google Scholar]
- Box, A.G.; Feito, Y.; Brown, C.; Heinrich, K.M.; Petruzzello, S.J. High Intensity Functional Training (HIFT) and Competitions: How Motives Differ by Length of Participation. PLoS ONE 2019, 14, e0213812. [Google Scholar] [CrossRef]
- Wankel, L.M. The Importance of Enjoyment to Adherence and Psychological Benefits from Physical Activity. Int. J. Sport Psychol. 1993, 24, 151–169. [Google Scholar]
- Singh, B.; Olds, T.; Curtis, R.; Dumuid, D.; Virgara, R.; Watson, A.; Szeto, K.; O’Connor, E.; Ferguson, T.; Eglitis, E.; et al. Effectiveness of Physical Activity Interventions for Improving Depression, Anxiety and Distress: An Overview of Systematic Reviews. Br. J. Sports Med. 2023, 57, 1203–1209. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.B.; Silva, E.S.; Hallgren, M.; De Leon, A.P.; Dunn, A.L.; Deslandes, A.C.; et al. Physical Activity and Incident Depression: A Meta-Analysis of Prospective Cohort Studies. Am. J. Psychiatry 2018, 175, 631–648. [Google Scholar] [CrossRef] [PubMed]
- Mikkelsen, K.; Stojanovska, L.; Polenakovic, M.; Bosevski, M.; Apostolopoulos, V. Exercise and Mental Health. Maturitas 2017, 106, 48–56. [Google Scholar] [CrossRef]
- Sornborger, J.; Fann, A.; Serpa, J.G.; Ventrelle, J.; R.D.N., M.S.; Ming Foynes, M.; Carleton, M.; Sherrill, A.M.; Kao, L.K.; Jakubovic, R.; et al. Integrative Therapy Approaches for Posttraumatic Stress Disorder: A Special Focus on Treating Veterans. Focus (Madison) 2017, 15, 390–398. [Google Scholar] [CrossRef]
- Whitworth, J.W.; Craft, L.L.; Dunsiger, S.I.; Ciccolo, J.T. Direct and Indirect Effects of Exercise on Posttraumatic Stress Disorder Symptoms: A Longitudinal Study. Gen. Hosp. Psychiatry 2017, 49, 56–62. [Google Scholar] [CrossRef]
- Hruby, A.; Lieberman, H.R.; Smith, T.J. Symptoms of Depression, Anxiety, and Post-Traumatic Stress Disorder and Their Relationship to Health-Related Behaviors in over 12,000 US Military Personnel: Bi-Directional Associations. J. Affect. Disord. 2021, 283, 84–93. [Google Scholar] [CrossRef]
- Strohacker, K.; Fazzino, D.; Breslin, W.L.; Xu, X. The Use of Periodization in Exercise Prescriptions for Inactive Adults: A Systematic Review. Prev. Med. Reports 2015, 2, 385–396. [Google Scholar] [CrossRef]
- McKeon, G.; Steel, Z.; Wells, R.; Newby, J.; Hadzi-Pavlovic, D.; Vancampfort, D.; Rosenbaum, S. A Mental Health–Informed Physical Activity Intervention for First Responders and Their Partners Delivered Using Facebook: Mixed Methods Pilot Study. JMIR Form. Res. 2021, 5, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, S.; Sherrington, C.; Tiedemann, A. Exercise Augmentation Compared with Usual Care for Post-Traumatic Stress Disorder: A Randomized Controlled Trial. Acta Psychiatr. Scand. 2015, 131, 350–359. [Google Scholar] [CrossRef] [PubMed]
- Ashdown-Franks, G.; Firth, J.; Carney, R.; Carvalho, A.F.; Hallgren, M.; Koyanagi, A.; Rosenbaum, S.; Schuch, F.B.; Smith, L.; Solmi, M.; et al. Exercise as Medicine for Mental and Substance Use Disorders: A Meta-Review of the Benefits for Neuropsychiatric and Cognitive Outcomes. Sport. Med. 2020, 50, 151–170. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, S.; Vancampfort, D.; Steel, Z.; Newby, J.; Ward, P.B.; Stubbs, B. Physical Activity in the Treatment of Post-Traumatic Stress Disorder: A Systematic Review and Meta-Analysis. Psychiatry Res. 2015, 230, 130–136. [Google Scholar] [CrossRef] [PubMed]
- Feito, Y.; Heinrich, K.M.; Butcher, S.J.; Poston, W.S.C. High-Intensity Functional Training (HIFT): Definition and Research Implications for Improved Fitness. Sports 2018, 6, 76. [Google Scholar] [CrossRef]
- Bycura, D.K.; Repka, C.P.; Santos, A.C.; Lopez, N.V. Training Implications for Firefighters through Objective Measurement of the Physiological Demands of Firefighter Job Tasks. Am. J. Biomed. Sci. Res. 2019, 3, 447–452. [Google Scholar] [CrossRef]
- Haddock, C.K.; Poston, W.S.C.; Heinrich, K.M.; Jahnke, S.A.; Jitnarin, N. The Benefits of High Intensity Functional Training (HIFT) Fitness Programs for Military Personnel. Mil. Med. 2016, 181, e1508–e1514. [Google Scholar] [CrossRef]
- Smith, D.L. Firefighter Fitness: Improving Performance and Preventing Injuries and Fatalities. Curr. Sports Med. Rep. 2011, 10, 167–172. [Google Scholar] [CrossRef]
- Bycura, D.K.; Dmitrieva, N.O.; Santos, A.C.; Waugh, K.L.; Ritchey, K.M. Efficacy of a Goal Setting and Implementation Planning Intervention on Firefighters’ Cardiorespiratory Fitness. J. Strength Cond. Res. 2019, 33, 3151–3161. [Google Scholar] [CrossRef]
- Smith, B.W.; Ortiz, J.A.; Steffen, L.E.; Tooley, E.M.; Wiggins, K.T.; Yeater, E.A.; Montoya, J.D.; Bernard, M.L. Mindfulness Is Associated with Fewer PTSD Symptoms, Depressive Symptoms, Physical Symptoms, and Alcohol Problems in Urban Firefighters. J. Consult. Clin. Psychol. 2011, 79, 613–617. [Google Scholar] [CrossRef]
- Skeffington, P.M.; Rees, C.S.; Mazzucchelli, T.G.; Kane, R.T. The Primary Prevention of PTSD in Firefighters: Preliminary Results of an RCT with 12-Month Follow-Up. PLoS ONE 2016, 11, e0155873. [Google Scholar] [CrossRef] [PubMed]
- Boffa, J.W.; Stanley, I.H.; Hom, M.A.; Norr, A.M.; Joiner, T.E.; Schmidt, N.B. PTSD Symptoms and Suicidal Thoughts and Behaviors among Firefighters. J. Psychiatr. Res. 2017, 84, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Haglund, M.E.M.; Nestadt, P.S.; Cooper, N.S.; Southwick, S.M.; Charney, D.S. Psychobiological Mechanisms of Resilience: Relevance to Prevention and Treatment of Stress-Related Psychopathology. Dev. Psychopathol. 2007, 19, 889–920. [Google Scholar] [CrossRef]
- Schäfer, S.K.; Sopp, M.R.; Staginnus, M.; Lass-Hennemann, J.; Michael, T. Correlates of Mental Health in Occupations at Risk for Traumatization: A Cross-Sectional Study. BMC Psychiatry 2020, 20, 335. [Google Scholar] [CrossRef]
- Krakauer, R.L.; Stelnicki, A.M.; Carleton, R.N. Examining Mental Health Knowledge, Stigma, and Service Use Intentions Among Public Safety Personnel. Front. Psychol. 2020, 11, 949. [Google Scholar] [CrossRef]
- Joyce, S.; Shand, F.; Bryant, R.A.; Lal, T.J.; Harvey, S.B. Mindfulness-Based Resilience Training in the Workplace: Pilot Study of the Internet-Based Resilience@Work (RAW) Mindfulness Program. J. Med. Internet Res. 2018, 20, e10326. [Google Scholar] [CrossRef]
- MacMillan, F.; Kolt, G.S.; Le, A.; George, E.S. Systematic Review of Randomised Control Trial Health Promotion Intervention Studies in the Fire Services: Study Characteristics, Intervention Design and Impacts on Health. Occup. Environ. Med. 2021, 78, 454–463. [Google Scholar] [CrossRef]
- Kyron, M.J.; Rees, C.S.; Lawrence, D.; Carleton, R.N.; McEvoy, P.M. Prospective Risk and Protective Factors for Psychopathology and Wellbeing in Civilian Emergency Services Personnel: A Systematic Review. J. Affect. Disord. 2021, 281, 517–532. [Google Scholar] [CrossRef]
- Kshtriya, S.; Kobezak, H.M.; Popok, P.; Lawrence, J.; Lowe, S.R. Social Support as a Mediator of Occupational Stressors and Mental Health Outcomes in First Responders. J. Community Psychol. 2020, 48, 2252–2263. [Google Scholar] [CrossRef]
- Bartlett, B.A.; Smith, L.J.; Tran, J.K.; Vujanovic, A.A. Understanding Mental Health among Military Veterans in the Fire Service. Psychiatry Res. 2018, 267, 394–399. [Google Scholar] [CrossRef]
- Carleton, R.N.; Afifi, T.O.; Turner, S.; Taillieu, T.; Vaughan, A.D.; Anderson, G.S.; Ricciardelli, R.; MacPhee, R.S.; Cramm, H.A.; Czarnuch, S.; et al. Mental Health Training, Attitudes toward Support, and Screening Positive for Mental Disorders. Cogn. Behav. Ther. 2020, 49, 55–73. [Google Scholar] [CrossRef]
- Deady, M.; Peters, D.; Lang, H.; Calvo, R.; Glozier, N.; Christensen, H.; Harvey, S.B. Designing Smartphone Mental Health Applications for Emergency Service Workers. Occup. Med. 2017, 67, 425–428. [Google Scholar] [CrossRef] [PubMed]
- Denkova, E.; Zanesco, A.P.; Rogers, S.L.; Jha, A.P. Is Resilience Trainable? An Initial Study Comparing Mindfulness and Relaxation Training in Firefighters. Psychiatry Res. 2020, 285, 112794. [Google Scholar] [CrossRef] [PubMed]
- Onyedire, N.G.; Ekoh, A.T.; Chukwuorji, J.B.C.; Ifeagwazi, C.M. Posttraumatic Stress Disorder (PTSD) Symptoms among Firefighters: Roles of Resilience and Locus of Control. J. Workplace Behav. Health 2017, 32, 227–248. [Google Scholar] [CrossRef]
- Mao, X.; Fung, O.W.M.; Hu, X.; Loke, A.Y. Psychological Impacts of Disaster on Rescue Workers: A Review of the Literature. Int. J. Disaster Risk Reduct. 2018, 27, 602–617. [Google Scholar] [CrossRef]
- Stanley, I.H.; Hom, M.A.; Chu, C.; Dougherty, S.P.; Gallyer, A.J.; Spencer-Thomas, S.; Shelef, L.; Fruchter, E.; Comtois, K.A.; Gutierrez, P.M.; et al. Perceptions of Belongingness and Social Support Attenuate PTSD Symptom Severity Among Firefighters: A Multistudy Investigation. Psychol. Serv. 2019, 16, 543–555. [Google Scholar] [CrossRef]
- Meyer, E.C.; Zimering, R.T.; Knight, J.; Morissette, S.B.; Kamholz, B.W.; Coe, E.; Carpenter, T.P.; Keane, T.M.; Kimbrel, N.A.; Gulliver, S.B. Negative Emotionality Interacts with Trauma Exposure to Prospectively Predict Posttraumatic Stress Disorder Symptoms During Firefighters’ First 3 Years of Service. J. Trauma. Stress 2021, 34, 333–344. [Google Scholar] [CrossRef]
- Miller, A.; Unruh, L.; Wharton, T.; Liu, X.; Zhang, N. Individual and Organizational Factors Associated with Professional Quality of Life in Florida Fire Personnel. J. Emerg. Manag. 2018, 16, 173–182. [Google Scholar] [CrossRef]
- Witt, M.; Stelcer, B.; Czarnecka-Iwańczuk, M. Stress Coping Styles in Firemen Exposed to Severe Stress. Psychiatr. Pol. 2018, 52, 543–555. [Google Scholar] [CrossRef]
- Counson, I.; Hosemans, D.; Lal, T.J.; Mott, B.; Harvey, S.B.; Joyce, S. Mental Health and Mindfulness amongst Australian Fire Fighters. BMC Psychol. 2019, 7, 34. [Google Scholar] [CrossRef] [PubMed]
- Hegberg, N.J.; Hayes, J.P.; Hayes, S.M. Exercise Intervention in PTSD: A Narrative Review and Rationale for Implementation. Front. Psychiatry 2019, 10, 133. [Google Scholar] [CrossRef] [PubMed]
- Whitworth, J.W.; Ciccolo, J.T. Exercise and Post-Traumatic Stress Disorder in Military Veterans: A Systematic Review. Mil. Med. 2016, 181, 953–960. [Google Scholar] [CrossRef]
- Robertson, I.T.; Cooper, C.L.; Sarkar, M.; Curran, T. Resilience Training in the Workplace from 2003 to 2014: A Systematic Review. J. Occup. Organ. Psychol. 2015, 88, 533–562. [Google Scholar] [CrossRef]
- Leppin, A.L.; Bora, P.R.; Tilburt, J.C.; Gionfriddo, M.R.; Zeballos-Palacios, C.; Dulohery, M.M.; Sood, A.; Erwin, P.J.; Brito, J.P.; Boehmer, K.R.; et al. The Efficacy of Resiliency Training Programs: A Systematic Review and Meta-Analysis of Randomized Trials. PLoS ONE 2014, 9, e111420. [Google Scholar] [CrossRef]
- Hollerbach, B.S.; Jahnke, S.A.; Poston, W.S.C.; Harms, C.A.; Heinrich, K.M. Examining a Novel Firefighter Exercise Training Program on Simulated Fire Ground Test Performance, Cardiorespiratory Endurance, and Strength: A Pilot Investigation. J. Occup. Med. Toxicol. 2019, 14, 12. [Google Scholar] [CrossRef]
- Day, R.S.; Jahnke, S.A.; Haddock, C.K.; Kaipust, C.M.; Jitnarin, N.; Poston, W.S.C. Occupationally Tailored, Web-Based, Nutrition and Physical Activity Program for Firefighters: Cluster Randomized Trial and Weight Outcome. J. Occup. Environ. Med. 2019, 61, 841–848. [Google Scholar] [CrossRef]
- The First Twenty. The First 20 Academy. Available online: https://www.thefirsttwenty.org/programming/ (accessed on 28 January 2021).
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)-A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap Consortium: Building an International Community of Software Platform Partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- International Association of Fire Fighters. The Fire Service Joint Labor Management Wellness-Fitness Initiative Candidate Physical Ability Test, 2nd ed.; Fire Service Joint Labor Management Wellness-Fitness Initiative: Washington, DC, USA, 2007. [Google Scholar]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W. Validation and Utility of a Self-Report Version of PRIME-MD: The PHQ Primary Care Study. Primary Care Evaluation of Mental Disorders. Patient Health Questionnaire. JAMA 1999, 282, 1737–1744. [Google Scholar] [CrossRef]
- Blanchard, E.B.; Jones-Alexander, J.; Buckley, T.C.; Forneris, C.A. Psychometric Properties of the PTSD Checklist (PCL). Behav. Res. Ther. 1996, 34, 669–673. [Google Scholar] [CrossRef]
- Campbell-Sills, L.; Stein, M.B. Psychometric Analysis and Refinement of the Connor–Davidson Resilience Scale (CD-RISC): Validation of a 10-Item Measure of Resilience. J. Trauma. Stress 2007, 20, 1019–1028. [Google Scholar] [CrossRef] [PubMed]
- Tennant, R.; Hiller, L.; Fishwick, R.; Platt, S.; Joseph, S.; Weich, S.; Parkinson, J.; Secker, J.; Stewart-Brown, S. The Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): Development and UK Validation. Health Qual. Life Outcomes 2007, 5, 63. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.W. The Patient Health Questionnaire PHQ-9: Validity of a Brief Depression Severity Measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef] [PubMed]
- Lang, A.J.; Laffaye, C.; Satz, L.E.; Dresselhaus, T.R.; Stein, M.B. Sensitivity and Specificity of the PTSD Checklist in Detecting PTSD in Female Veterans in Primary Care. J. Trauma. Stress 2003, 16, 257–264. [Google Scholar] [CrossRef]
- Moshier, S.J.; Lee, D.J.; Bovin, M.J.; Gauthier, G.; Zax, A.; Rosen, R.C.; Keane, T.M.; Marx, B.P. An Empirical Crosswalk for the PTSD Checklist: Translating DSM-IV to DSM-5 Using a Veteran Sample. J. Trauma. Stress 2019, 32, 799–805. [Google Scholar] [CrossRef]
- Salisu, I.; Hashim, N. A Critical Review of Scales Used in Resilience Research. IOSR J. Bus. Manag. 2017, 19, 23–33. [Google Scholar] [CrossRef]
- Davidson, J.R.T. Connor-Davidson Resilience Scale (CD-RISC) © Manual, San Diego, CA, USA, 2020; unpublished.
- Connor, K.M.; Davidson, J.R.T. Scoring and Interpretation of the Connor-Davidson Resilience Scale (CD-RISC©), San Diego, CA, USA, 2020; unpublished. Available online: https://www.connordavidson-resiliencescale.com/CD-RISC%20Manual%2008-19-18.pdf (accessed on 30 June 2021).
- Connor, K.M.; Davidson, J.R.T. The Connor-Davidson Resilience Scale. Available online: http://www.connordavidson-resiliencescale.com/about.php (accessed on 30 June 2021).
- Stewart-Brown, S.; Tennant, A.; Tennant, R.; Platt, S.; Parkinson, J.; Weich, S. Internal Construct Validity of the Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): A Rasch Analysis Using Data from the Scottish Health Education Population Survey. Health Qual. Life Outcomes 2009, 7, 15. [Google Scholar] [CrossRef]
- Maheswaran, H.; Weich, S.; Powell, J.; Stewart-Brown, S. Evaluating the Responsiveness of the Warwick Edinburgh Mental Well-Being Scale (WEMWBS): Group and Individual Level Analysis. Health Qual. Life Outcomes 2012, 10, 156. [Google Scholar] [CrossRef]
- Warwick-Edinburgh Mental Well-Being Scale (WEMWBS): User Guide—Version 2, 2nd ed.; NHS Health Scotland: Edinburgh, UK, 2015.
- Haff, G.G.; Triplett, N.T. (Eds.) Essentials of Strength Training and Conditioning, 4th ed.; Human Kinetics: Champaign, IL, USA, 2016. [Google Scholar]
- Microsoft Corporation. Microsoft Excel; Microsoft Corporation: Redmond, WA, USA, 2018. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows; IBM Corp.: Armonk, NY, USA, 2021. [Google Scholar]
- Glen, S. Hedges’ g: Definition, Formula. Statistics How To.com: Elementary Statistics for the Rest of Us! Available online: https://www.statisticshowto.com/hedges-g/ (accessed on 6 April 2025).
- Brydges, C.R. Effect Size Guidelines, Sample Size Calculations, and Statistical Power in Gerontology. Innov. Aging 2019, 3, igz036. [Google Scholar] [CrossRef]
- Quintana, D.S. Statistical Considerations for Reporting and Planning Heart Rate Variability Case-Control Studies. Psychophysiology 2017, 54, 344–349. [Google Scholar] [CrossRef]
- Lovakov, A.; Agadullina, E.R. Empirically Derived Guidelines for Effect Size Interpretation in Social Psychology. Eur. J. Soc. Psychol. 2021, 51, 485–504. [Google Scholar] [CrossRef]
- National Institute of Standards and Technology. Hedge’s g Statistic. Available online: https://www.itl.nist.gov/div898/software/dataplot/refman2/auxillar/hedgeg.htm (accessed on 6 July 2025).
- Fritz, C.O.; Morris, P.E.; Richler, J.J. Effect Size Estimates: Current Use, Calculations, and Interpretation. J. Exp. Psychol. Gen. 2012, 141, 2–18. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.-G.; Buchner, A. G*Power 3: A Flexible Statistical Power Analysis Program for the Social, Behavioral, and Biomedical Sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical Power Analyses Using G*Power 3.1: Tests for Correlation and Regression Analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [PubMed]
- Etymologia: Bonferroni Correction. Emerg. Infect. Dis. 2015, 21, 289. [CrossRef]
- SAS Institute Inc. SAS for Windows; SAS Institute Inc.: Cary, NC, USA, 2016. [Google Scholar]
- Singer, J.D.; Willett, J.B. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence; Oxford University Press, Inc.: New York, NY, USA, 2003. [Google Scholar]
- Hoffman, L. Longitudinal Analysis: Modeling Within-Person Fluctuation and Change; Taylor & Francis: New York, NY, USA, 2015. [Google Scholar]
- Borg, G. Borg’s Perceived Exertion and Pain Scales; Human Kinetics: Champaign, IL, USA, 1998. [Google Scholar]
- Lakens, D. Calculating and Reporting Effect Sizes to Facilitate Cumulative Science: A Practical Primer for t-Tests and ANOVAs. Front. Psychol. 2013, 4, 863. [Google Scholar] [CrossRef] [PubMed]
- Taylor, J.M.; Alanazi, S. Cohen’s and Hedges’ G. J. Nurs. Educ. 2023, 62, 316–317. [Google Scholar] [CrossRef]
- National Center for PTSD. Using the PTSD Checklist for DSM-IV (PCL); U.S. Department of Veterans Affairs: Washington, DC, USA; pp. 1–4. Available online: https://www.ptsd.va.gov/professional/assessment/documents/PCL_handoutDSM4.pdf (accessed on 30 June 2021).
- Prime-md. Patient Health Questionnaire (PHQ-9); Pfizer Inc.: New York, NY, USA, 2005. [Google Scholar]
- Corthésy-Blondin, L.; Genest, C.; Dargis, L.; Bardon, C.; Mishara, B.L. Reducing the Impacts of Exposure to Potentially Traumatic Events on the Mental Health of Public Safety Personnel: A Rapid Systematic Scoping Review. Psychol. Serv. 2022, 19, 80–94. [Google Scholar] [CrossRef]
- Jahnke, S.A.; Gist, R.; Poston, W.S.C.; Haddock, C.K. Behavioral Health Interventions in the Fire Service: Stories from the Firehouse. J. Workplace Behav. Health 2014, 29, 113–126. [Google Scholar] [CrossRef]
- Lentz, L.; Smith-Macdonald, L.; Malloy, D.C.; Anderson, G.S.; Beshai, S.; Ricciardelli, R.; Brémault-Phillips, S.; Carleton, R.N. A Qualitative Analysis of the Mental Health Training and Educational Needs of Firefighters, Paramedics, and Public Safety Communicators in Canada. Int. J. Environ. Res. Public Health 2022, 19, 6972. [Google Scholar] [CrossRef]
- Tabachnick, B.G.; Fidell, L.S. Using Multivariate Statistics, 6th ed.; Pearson Education, Inc.: Upper Saddle River, NJ, USA, 2013. [Google Scholar]
- Sempf, F.; Thienes, G. High-Intensity Functional Training for Firefighters. Strength Cond. J. 2022, 44, 97–105. [Google Scholar] [CrossRef]
- Stratton, E.; Lampit, A.; Choi, I.; Calvo, R.A.; Harvey, S.B.; Glozier, N. Effectiveness of EHealth Interventions for Reducing Mental Health Conditions in Employees: A Systematic Review and Meta-Analysis. PLoS ONE 2017, 12, e0189904. [Google Scholar] [CrossRef] [PubMed]
- Igboanugo, S.; Bigelow, P.L.; Mielke, J.G. Health Outcomes of Psychosocial Stress within Firefighters: A Systematic Review of the Research Landscape. J. Occup. Health 2021, 63, e12219. [Google Scholar] [CrossRef] [PubMed]
- Hobfoll, S.E.; Halbesleben, J.; Neveu, J.-P.; Westman, M. Conservation of Resources in the Organizational Context: The Reality of Resources and Their Consequences. Annu. Rev. Organ. Psychol. Organ. Behav. 2018, 5, 103–128. [Google Scholar] [CrossRef]
- Sattler, D.N.; Preston, A.J.; Kaiser, C.F.; Olivera, V.E.; Valdez, J.; Schlueter, S. Hurricane Georges: A Cross-National Study Examining Preparedness, Resource Loss, and Psychological Distress in the U.S. Virgin Islands, Puerto Rico, Dominican Republic, and the United States. J. Trauma. Stress 2002, 15, 339–350. [Google Scholar] [CrossRef]
- Sattler, D.N.; Boyd, B.; Kirsch, J. Trauma-Exposed Firefighters: Relationships among Posttraumatic Growth, Posttraumatic Stress, Resource Availability, Coping and Critical Incident Stress Debriefing Experience. Stress Health 2014, 30, 356–365. [Google Scholar] [CrossRef]
- Joyce, S.; Shand, F.; Lal, T.J.; Mott, B.; Bryant, R.A.; Harvey, S.B. Resilience@Work Mindfulness Program: Results from a Cluster Randomized Controlled Trial with First Responders. J. Med. Internet Res. 2019, 21, e12894. [Google Scholar] [CrossRef]
- Christopher, M.S.; Hunsinger, M.; Goerling, L.R.J.; Bowen, S.; Rogers, B.S.; Gross, C.R.; Dapolonia, E.; Pruessner, J.C. Mindfulness-Based Resilience Training to Reduce Health Risk, Stress Reactivity, and Aggression among Law Enforcement Officers: A Feasibility and Preliminary Efficacy Trial. Psychiatry Res. 2018, 264, 104–115. [Google Scholar] [CrossRef]
- Arnetz, B.B.; Arble, E.; Backman, L.; Lynch, A.; Lublin, A. Assessment of a Prevention Program for Work-Related Stress among Urban Police Officers. Int. Arch. Occup. Environ. Health 2013, 86, 79–88. [Google Scholar] [CrossRef]
- Pace, T.W.W.; Zeiders, K.H.; Cook, S.H.; Sarsar, E.D.; Hoyt, L.T.; Mirin, N.L.; Wood, E.P.; Tatar, R.; Davidson, R.J. Feasibility, Acceptability, and Preliminary Efficacy of an App-Based Meditation Intervention to Decrease Firefighter Psychological Distress and Burnout: A One-Group Pilot Study. JMIR Form. Res. 2022, 6, e34951. [Google Scholar] [CrossRef] [PubMed]
- Sharp, P.; Caperchione, C.M.; Brown, G.A.; Stadnyk, A.; Marin, E.; Hulin, B.; Wade, J.; Mott, B.; Gabriel, M.; Impellizzeri, F.; et al. A Pragmatic Strength and Conditioning Intervention for Firefighters: Feasibility of the Tactical Athlete Resilience Program (TARP). Health Promot. J. Aust. 2023, 34, 60–69. [Google Scholar] [CrossRef] [PubMed]
- Heydari, A.; Ostadtaghizadeh, A.; Khorasani-Zavareh, D.; Ardalan, A.; Ebadi, A.; Mohammadfam, I.; Shafaei, H. Building Resilience in Firefighters: A Systematic Review. Iran. J. Public Health 2022, 51, 1546–1558. [Google Scholar] [CrossRef] [PubMed]
- Alexander, L.; Cooper, K. Vocational Rehabilitation for Emergency Services Personnel: A Scoping Review. JBI Evid. Synth. 2019, 17, 1999–2019. [Google Scholar] [CrossRef]
- Elliot, D.L.; Goldberg, L.; Duncan, T.E.; Kuehl, K.S.; Moe, E.L.; Rosemary Breger, M.K.; DeFrancesco, C.L.; Denise Ernst, R.B.; Stevens, V.J. The PHLAME Firefighters’ Study: Feasibility and Findings. Am. J. Health Behav. 2004, 28, 13–23. [Google Scholar] [CrossRef]
- Norris, R.; Carroll, D.; Cochrane, R. The Effects of Aerobic and Anaerobic Training on Fitness, Blood Pressure, and Psychological Stress and Well-Being. J. Psychosom. Res. 1990, 34, 367–375. [Google Scholar] [CrossRef]
- Norvell, N.; Belles, D. Psychological and Physical Benefits of Circuit Weight Training in Law Enforcement Personnel. J. Consult. Clin. Psychol. 1993, 16, 520–527. [Google Scholar] [CrossRef]
- Lan, F.Y.; Scheibler, C.; Hershey, M.S.; Romero-Cabrera, J.L.; Gaviola, G.C.; Yiannakou, I.; Fernandez-Montero, A.; Christophi, C.A.; Christiani, D.C.; Sotos-Prieto, M.; et al. Effects of a Healthy Lifestyle Intervention and COVID-19-Adjusted Training Curriculum on Firefighter Recruits. Sci. Rep. 2022, 12, 10607. [Google Scholar] [CrossRef]
- Fraess-Phillips, A.; Wagner, S.; Harris, R.L. Firefighters and Traumatic Stress: A Review. Int. J. Emerg. Serv. 2017, 6, 67–80. [Google Scholar] [CrossRef]
- Sommerfeld, A.; Wagner, S.L.; Harder, H.G.; Schmidt, G. Behavioral Health and Firefighters: An Intervention and Interviews with Canadian Firefighters. J. Loss Trauma 2017, 22, 307–324. [Google Scholar] [CrossRef]
- Laureys, V.; Easton, M. Resilience of Firefighters Exposed to Potentially Traumatic Events: A Literature Review. Int. J. Emerg. Serv. 2020, 9, 217–232. [Google Scholar] [CrossRef]

| Characteristic | n | % | |
|---|---|---|---|
| Sex | Female | 3 | 10.00 |
| Male | 27 | 90.00 | |
| Rank | Firefighter | 8 | 26.66 |
| Engineer | 6 | 20.00 | |
| Captain | 10 | 33.33 | |
| Battalion Chief | 6 | 20.00 | |
| Relationship Status | Single | 3 | 10.00 |
| In a relationship | 2 | 6.66 | |
| Married or domestic partnership | 24 | 80.00 | |
| Divorced or separated | 1 | 3.33 | |
| Education Level | Some college but no degree | 2 | 6.66 |
| Associate degree | 13 | 43.33 | |
| Bachelor degree | 13 | 43.33 | |
| Graduate degree | 2 | 6.66 | |
| Race | White | 27 | 90.00 |
| Other | 1 | 3.33 | |
| Don’t know | 1 | 3.33 | |
| Prefer not to say | 1 | 3.33 | |
| Ethnicity | Not Hispanic | 26 | 86.66 |
| Hispanic | 3 | 10.00 | |
| Prefer not to say | 1 | 3.33 | |
| Characteristic | M (SD) | Range | |
| Age (years) | 39.70 (7.71) | 23.00–57.00 | |
| Years in fire service | 15.43 (8.37) | 1.00–35.00 | |
| Pre-Intervention, Full Sample (n = 30) | Pre-Intervention, Returning Sample (n = 20) | Post-Intervention, Returning Sample (n = 20) | ||||
|---|---|---|---|---|---|---|
| Variable | M (SD) | Range | M (SD) | Range | M (SD) | Range |
| Height (cm) | 179.41 (7.68) | 160.02–190.50 | 181.36 (6.61) | 170.18–190.50 | 181.36 (6.61) | 170.18–190.50 |
| Weight (kg) | 91.09 (12.65) | 64.33–120.95 | 93.33 (10.33) | 77.27–120.95 | 92.61 (9.61) | 78.41–115.77 |
| LBM (kg) | 71.99 (9.51) | 50.44–86.67 | 74.83 (7.23) | 63.15–86.67 | 74.34 (7.34) | 63.24–87.40 |
| BMI (kg·m−2) | 28.23 (2.96) | 22.48–35.25 | 28.36 (2.49) | 22.48–33.33 | 28.15 (2.32) | 22.81–31.90 |
| %BF | 20.76 (5.44) | 11.10–31.80 | 19.57 (5.26) | 11.10–31.80 | 19.56 (4.76) | 11.30–29.10 |
| T-CAC (stations) | 22.12 (3.83) | 15.00–30.00 | 22.91 (3.40) | 16.00–29.33 | 25.09 (3.94) | 17.00–32.47 |
| Occasion | PHQ-9 | PCL-C | ||||
|---|---|---|---|---|---|---|
| M (SD) | Range | Missing (%) | M (SD) | Range | Missing (%) | |
| Baseline (Week 0) | 3.43 (3.22) | 0–10 | 0 (0.00) | 32.11 (13.20) | 17–66 | 2 (6.66) |
| Pre-Intervention (Week 4) | 3.77 (3.61) | 0–12 | 0 (0.00) | 32.33 (14.28) | 17–69 | 0 (0.00) |
| Midpoint (Week 11) | 2.83 (2.71) | 0–11 | 1 (3.33) | 29.31 (13.88) | 17–73 | 1 (3.33) |
| Post-Intervention (Week 17) | 2.93 (4.32) | 0–20 | 3 (10.00) | 28.33 (13.47) | 17–68 | 3 (10.00) |
| Occasion | CD-RISC10 | WEMWBS | ||||
| M (SD) | Range | Missing (%) | M (SD) | Range | Missing (%) | |
| Baseline (Week 0) | 31.31 (5.97) | 16–40 | 1 (3.33) | 50.25 (7.93) | 31–61 | 2 (6.66) |
| Pre-Intervention (Week 4) | 30.27 (5.60) | 16–39 | 0 (0.00) | 50.37 (9.20) | 30–68 | 0 (0.00) |
| Midpoint (Week 11) | 31.00 (5.25) | 23–40 | 1 (3.33) | 50.48 (7.61) | 33–70 | 1 (3.33) |
| Post-Intervention (Week 17) | 32.04 (5.73) | 19–40 | 3 (10.00) | 52.81 (9.74) | 33–70 | 4 (13.33) |
| Hedges’ g | |||||||
|---|---|---|---|---|---|---|---|
| Outcome | M Diff. (SD) | 95% CI | t | p a | Missing (%) | Point Estimate | 95% CI |
| PHQ-9 | 0.33 (2.48) | [−0.59, 1.26] | 0.74 | 0.47 | 0 (0.00) | 0.13 | [−0.22, 0.49] |
| PCL-C | 0.89 (5.51) | [−1.24, 3.03] | 0.86 | 0.40 | 2 (6.66) | 0.16 | [−0.21, 0.53] |
| CD-RISC10 | −1.00 (3.32) | [−2.26, 0.26] | −1.62 | 0.12 | 1 (3.33) | −0.30 | [−0.66, 0.07] |
| WEMWBS | −0.46 (4.54) | [−2.23, 1.30] | −0.54 | 0.59 | 2 (6.66) | −0.10 | [−0.47, 0.27] |
| Hedges’ g | |||||||
|---|---|---|---|---|---|---|---|
| Variable | M Diff. (SD) | 95% CI | t | p a | Missing (%) | Point Estimate | 95% CI |
| BW (kg) | −0.72 (2.14) | [−1.72, 0.29] | −1.50 | 0.15 | 10 (33.33) | −0.32 | [−0.75, 0.12] |
| LBM (kg) | −0.48 (2.05) | [−1.44, 0.48] | −1.06 | 0.30 | 10 (33.33) | −0.23 | [−0.65, 0.20] |
| BMI (kg·m−2) | −0.21 (0.63) | [−0.51, 0.08] | −1.51 | 0.15 | 10 (33.33) | −0.32 | [−0.75, 0.11] |
| %BF | −0.02 (1.50) | [−0.72, 0.69] | −0.05 | 0.97 | 10 (33.33) | −0.01 | [−0.43, 0.41] |
| T-CAC (stations) | 2.18 (1.51) | [1.47, 2.88] | 6.46 | <0.001 | 10 (33.33) | 1.42 | [0.79, 2.03] |
| Hedges’ g | |||||||
|---|---|---|---|---|---|---|---|
| Variable | M Diff. (SD) | 95% CI | t | p a | Missing (%) | Point Estimate | 95% CI |
| PHQ-9 | −0.93 (2.90) | [−2.07, 0.22] | −1.66 | 0.11 | 3 (10.00) | −0.32 | [−0.69, 0.07] |
| PCL-C | −5.00 (7.40) | [−7.93, −2.07] | −3.51 | 0.002 | 3 (10.00) | −0.67 | [−1.07, −0.25] |
| CD-RISC10 | 2.19 (4.52) | [0.40, 3.97] | 2.51 | 0.02 | 3 (10.00) | 0.48 | [0.08, 0.87] |
| WEMWBS | 2.39 (7.10) | [−0.48, 5.25] | 1.71 | 0.10 | 4 (13.33) | 0.33 | [−0.06, 0.72] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Santos, A.C.; Long, S.; Moreno, C.P.; Bycura, D. Effectiveness of a Mind–Body Intervention at Improving Mental Health and Performance Among Career Firefighters. Int. J. Environ. Res. Public Health 2025, 22, 1227. https://doi.org/10.3390/ijerph22081227
Santos AC, Long S, Moreno CP, Bycura D. Effectiveness of a Mind–Body Intervention at Improving Mental Health and Performance Among Career Firefighters. International Journal of Environmental Research and Public Health. 2025; 22(8):1227. https://doi.org/10.3390/ijerph22081227
Chicago/Turabian StyleSantos, Anthony C., Seth Long, Christopher P. Moreno, and Dierdra Bycura. 2025. "Effectiveness of a Mind–Body Intervention at Improving Mental Health and Performance Among Career Firefighters" International Journal of Environmental Research and Public Health 22, no. 8: 1227. https://doi.org/10.3390/ijerph22081227
APA StyleSantos, A. C., Long, S., Moreno, C. P., & Bycura, D. (2025). Effectiveness of a Mind–Body Intervention at Improving Mental Health and Performance Among Career Firefighters. International Journal of Environmental Research and Public Health, 22(8), 1227. https://doi.org/10.3390/ijerph22081227





