Post-Traumatic Stress Disorder (PTSD) Resulting from Road Traffic Accidents (RTA): A Systematic Literature Review
Abstract
1. Introduction
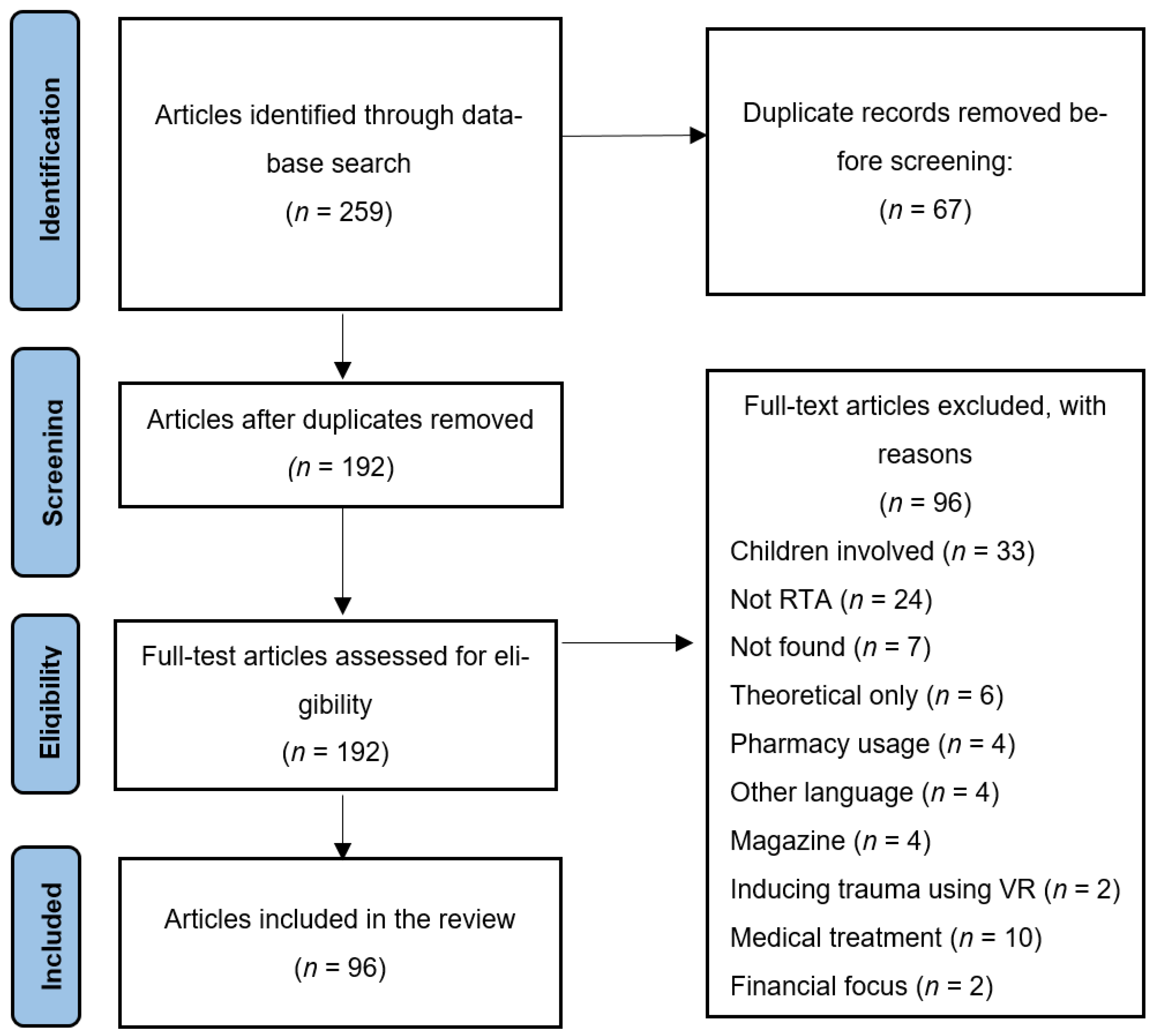
2. Materials and Methods
2.1. Information Sources
2.2. Eligibility Criteria
2.3. Data Screening and Extraction
2.4. Data Synthesis
3. Results and Discussion
Study and Sample Characteristics
4. Overview of Findings
4.1. PTSD Symptom Prevalence and Persistence
4.1.1. Prevalence of Symptoms of PTSD
4.1.2. Persistence of Symptoms of PTSD
4.2. Risk Factors for Developing PTSD Post-RTA
4.2.1. Biological and Injury-Related Factors
4.2.2. Psychological Factors
4.2.3. Social and Demographic Factors
4.3. Sociodemographic Factors Do Not Impact PTSD Post-RDA
4.4. Cognitive Mechanisms Associated with PTSD After an RTA
4.4.1. Rumination and Thought Suppression
4.4.2. Working Memory and Cognitive Interference
4.4.3. Metacognitive Beliefs
4.4.4. Symptom Pattern and Timing
4.4.5. Coping Style and Interpersonal Functioning
4.5. Quality of Life and PTSD
4.6. Post-Traumatic Growth After a RTA
4.7. Comorbid Psychological and Cognitive Factors Associated with PTSD Post-RTA
4.7.1. Acute Stress and Mood Disorders
4.7.2. Traumatic Brain Injury and PTSD Symptom Profiles
4.7.3. Comorbidity with Other Psychological and Cognitive Factors
4.8. Treatments for PTSD
4.8.1. Cognitive Behavioural Therapy for PTSD Post-RTA
4.8.2. Virtual Reality Treatment for PTSD Post-RTA
4.8.3. Other Treatments of PTSD Post-RTA
4.9. The Consequence of the PTSD
4.9.1. Impact of PTSD Post-RTA on Heart Rate
4.9.2. Impact of PTSD Post-RTA on Brain Function
4.9.3. Impact of PTSD Post-RTA on Employment
4.10. Scales Used to Measure PTSD
5. Implications for Mental Health Services and Public Health Policy
6. Limitations of the Extant Literature
7. Conclusions
8. Recommendations for Research
9. Recommendations for Policy
9.1. Routine Psychological Screening Post-RTA
9.2. Integration of Brief CBT into Early Intervention Pathways
9.3. Public Awareness Campaigns Targeting Minor RTA Survivors
9.4. Development and Regulation of PTSD Assessment Tools
9.5. Cross-Sector Data Sharing and Support Coordination
9.6. Investment in Innovative Treatments, Including VR
9.7. Support for Families and Social Networks
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Washington, DC, USA, 2013. [Google Scholar]
- World Health Organisation. Global Status Report on Prehospital and Emergency Care 2018. 2018. Available online: https://www.who.int/publications/i/item/9789241565684 (accessed on 10 November 2023).
- Bryant, R.A. Post-traumatic stress disorder: A state-of-the-art review of evidence and challenges. World Psychiatry 2019, 18, 259–269. [Google Scholar] [CrossRef] [PubMed]
- Brewin, C.R.; Atwoli, L.; Bisson, J.I.; Galea, S.; Koenen, K.; Lewis-Fernández, R. Post-traumatic stress disorder: Evolving conceptualization and evidence, and future research directions. World Psychiatry 2025, 24, 52–80. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.J. Psychiatric Morbidity Following Road Traffic Accidents. Ph.D. Thesis, University College London, London, UK, 1997. Available online: https://discovery.ucl.ac.uk/id/eprint/10098971 (accessed on 10 November 2023).
- Leroy, A.; Cottencin, O.; Labreuche, J.; Mascarel, P.; De Pourtales, M.A.; Molenda, S.; Paget, V.; Lemogne, C.; Bougerol, T.; Gregory, T.; et al. Four Questions Nurses Can Ask to Predict PTSD 1 Year after a Motor Vehicle Crash. J. Trauma Nurs. 2022, 29, 70–79. [Google Scholar] [CrossRef] [PubMed]
- Koren, D.; Arnon, I.; Klein, E. Long term course of chronic post-traumatic stress disorder in traffic accident victims: A three-year prospective follow-up study. Behav. Res. Ther. 2001, 39, 1449–1458. [Google Scholar] [CrossRef]
- Koenen, K.C.; Ratanatharathorn, A.; Ng, L.; McLaughlin, K.A.; Bromet, E.J.; Stein, D.J.; Karam, E.G.; Ruscio, A.M.; Benjet, C.; Scott, K.; et al. Posttraumatic stress disorder in the World Mental Health Surveys. Psychol. Med. 2017, 47, 2260–2274. [Google Scholar] [CrossRef]
- Lin, W.; Gong, L.; Xia, M.; Dai, W. Prevalence of post-traumatic stress disorder among road traffic accident survivors: A PRISMA-compliant meta-analysis. Medicine 2018, 97, e9693. [Google Scholar] [CrossRef]
- Ponniah, K.; Hollon, S.D. Empirically supported psychological treatments for adult acute stress disorder and post-traumatic stress disorder: A review. Depress. Anxiety 2009, 26, 1086–1109. [Google Scholar] [CrossRef]
- Boccia, M.; Piccardi, L.; Cordellieri, P.; Guariglia, C.; Giannini, A.M. EMDR therapy for PTSD after motor vehicle accidents: Meta-analytic evidence for specific treatment. Front. Hum. Neurosci. 2015, 9, 213. [Google Scholar] [CrossRef]
- Daddah, D.; Glele Ahanhanzo, Y.; Kpozehouen, A.; Hounkpe Dos Santos, B.; Ouendo, E.M.; Leveque, A. Prevalence and Risk Factors of Post-Traumatic Stress Disorder in Survivors of a Cohort of Road Accident Victims in Benin: Results of a 12-Month Cross-Sectional Study. J. Multidiscip. Healthc. 2022, 15, 719–731. [Google Scholar] [CrossRef]
- Yimer, G.M.; Adem, Y.F.; Haile, Y. Determinants of post-traumatic stress disorder among survivors of road traffic accidents in dessie comprehensive specialized hospital North-East Ethiopia. BMC Psychiatry 2023, 23, 218. [Google Scholar] [CrossRef]
- Transport Community. Road Safety Statistics: Western Balkans 2023. Available online: https://www.transport-community.org/wp-content/uploads/2024/10/Road-Safety-Statistics_Western-Balkans_2023.pdf (accessed on 22 October 2023).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.; Colquhoun, H.; Kastner, M.; Levac, D.; Ng, C.; Sharpe, J.P.; Wilson, K.; et al. A scoping review on the conduct and reporting of scoping reviews. BMC Med. Res. Methodol. 2016, 16, 15. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Adawi, M.; Zerbetto, R.; Re, T.S.; Bisharat, B.; Mahamid, M.; Amital, H.; Del Puente, G.; Bragazzi, N.L. Psychometric properties of the Brief Symptom Inventory in nomophobic subjects: Insights from preliminary confirmatory factor, exploratory factor, and clustering analyses in a sample of healthy Italian volunteers. Psychol. Res. Behav. Manag. 2019, 12, 145–154. [Google Scholar] [CrossRef]
- Angerpointner, K.; Weber, S.; Tschech, K.; Schubert, H.; Herbst, T.; Ernstberger, A.; Kerschbaum, M. Post-traumatic stress disorder after minor trauma—A prospective cohort study. Med. Hypotheses 2020, 135, 109465. [Google Scholar] [CrossRef]
- Asmundson, G.J.G.; Cox, B.J.; Larsen, D.K.; Frombach, I.K.; Norton, G.R. Psychometric properties of the Accident Fear Questionnaire: An analysis based on motor vehicle accident survivors in a rehabilitation setting. Rehabil. Psychol. 1999, 44, 373–387. [Google Scholar] [CrossRef]
- Asuquo, J.E.; Edet, B.E.; Abang, I.E.; Essien, E.A.; Osakwe, O.G.; Aigbomain, E.J.; Chigbundu, K.C. Depression and post-traumatic stress disorder among road traffic accident victims managed in a Tertiary hospital in Southern Nigeria. Niger. J. Clin. Pract. 2017, 20, 170–175. [Google Scholar] [CrossRef]
- Aykaç, C.; Direk, N.; Kemik, K.; Alkın, T. Examination of post-traumatic growth, post-traumatic stress symptoms, and neurocognitive flexibility levels in individuals who have experienced a traffic accident. Turk. J. Clin. Psychiatry 2024, 27, 65–73. [Google Scholar] [CrossRef]
- Bae, S.M.; Hyun, M.H.; Lee, S.H. Comparison of Memory Function and MMPI-2 Profile between Post-traumatic Stress Disorder and Adjustment Disorder after a Traffic Accident. Clin. Psychopharmacol. Neurosci. 2014, 12, 41–47. [Google Scholar] [CrossRef]
- Bae, S.M.; Hyun, M.H.; Ra, Y.S. Mediating effects of forgiveness and emotion-focused coping on post-traumatic stress disorder symptoms caused by physical injury and perceived threat. Asia Pac. Psychiatry 2015, 7, 164–172. [Google Scholar] [CrossRef]
- Baptie, G.; Andrade, J.; Bacon, A.M.; Norman, A. Virtually renovating the Trauma Film Paradigm: Comparing virtual reality with on-screen presentation of an analogue trauma. Cyberpsychol. J. Psychosoc. Res. Cyberspace 2021, 15. [Google Scholar] [CrossRef]
- Barth, J.; Kopfmann, S.; Nyberg, E.; Angenendt, J.; Frommberger, U. Post-traumatic stress disorders and extent of psychosocial impairments five years after a traffic accident. Psychosoc. Med. 2005, 2, Doc09. [Google Scholar] [PubMed]
- Beck, J.G.; Gudmundsdottir, B.; Palyo, S.A.; Miller, L.M.; Grant, D.M. Rebound effects following deliberate thought suppression: Does PTSD make a difference? Behav. Ther. 2006, 37, 170–180. [Google Scholar] [CrossRef]
- Beck, J.G.; Palyo, S.A.; Winer, E.H.; Schwagler, B.E.; Ang, E.J. Virtual Reality Exposure Therapy for PTSD symptoms after a road accident: An uncontrolled case series. Behav. Ther. 2007, 38, 39–48. [Google Scholar] [CrossRef] [PubMed]
- Bedaso, A.; Kediro, G.; Ebrahim, J.; Tadesse, F.; Mekonnen, S.; Gobena, N.; Gebrehana, E. Prevalence and determinants of post-traumatic stress disorder among road traffic accident survivors: A prospective survey at selected hospitals in southern Ethiopia. BMC Emerg. Med. 2020, 20, 52. [Google Scholar] [CrossRef]
- Benjamin, C.L.; O’Neil, K.A.; Crawley, S.A.; Beidas, R.S.; Coles, M.; Kendall, P.C. Patterns and predictors of subjective units of distress in anxious youth. Behav. Cogn. Psychother. 2010, 38, 497–504. [Google Scholar] [CrossRef]
- Berntsen, D.; Rubin, D.C. The centrality of event scale: A measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behav. Res. Ther. 2006, 44, 219–231. [Google Scholar] [CrossRef]
- Blanchard, E.B.; Hickling, E.J.; Buckley, T.C.; Taylor, A.E.; Vollmer, A.; Loos, W.R. Psychophysiology of post-traumatic stress disorder related to motor vehicle accidents: Replication and extension. J. Consult. Clin. Psychol. 1996, 64, 742. [Google Scholar] [CrossRef]
- Blanchard, E.B.; Hickling, E.J.; Malta, L.S.; Jaccard, J.; Devineni, T.; Veazey, C.H.; Galovski, T.E. Prediction of response to psychological treatment among motor vehicle accident survivors with PTSD. Behav. Ther. 2003, 34, 351–363. [Google Scholar] [CrossRef]
- Blanchard, E.B.; Buckley, T.C. Psychophysiological assessment of post-traumatic stress disorder. In Post-Traumatic Stress Disorder: A Comprehensive Text; Saigh, P.A., Bremner, J.D., Eds.; Allyn and Bacon: Boston, MA, USA, 1938. [Google Scholar]
- Blanchard, E.B.; Hickling, E.J. After the Crash: Psychological Assessment and Treatment of Survivors of Motor Vehicle Accidents; American Psychological Association: Washington, DC, USA, 2004. [Google Scholar]
- Boelen, P.A.; Eisma, M.C.; de Keijser, J.; Lenferink, L.I.M. Treatment Gap in Mental Health Care for Victims of Road Traffic Accidents. Clin. Psychol. Psychother. 2024, 31, e2970. [Google Scholar] [CrossRef]
- Brand, S.; Otte, D.; Petri, M.; Decker, S.; Stübig, T.; Krettek, C.; Müller, C.W. Incidence of post-traumatic stress disorder after traffic accidents in Germany. Int. J. Emerg. Ment. Health 2014, 16, 233–236. [Google Scholar] [CrossRef] [PubMed]
- Briere, J.; Elliot, D.M.; Harris, K.; Cotman, A. Trauma Symptom Inventory:Psychometrics and Association With Childhood and Adult Victimization in Clinical Samples. J. Interpers. Violence 1995, 10, 387–401. [Google Scholar] [CrossRef]
- Brom, D.; Kleber, R.J.; Hofman, M.C. Victims of traffic accidents: Incidence and prevention of post-traumatic stress disorder. J. Clin. Psychol. 1993, 49, 131–140. [Google Scholar] [CrossRef]
- Bryant, R.A.; Harvey, A.G.; Guthrie, R.M.; Moulds, M.L. A prospective study of psychophysiological arousal, acute stress disorder, and post-traumatic stress disorder. J. Abnorm. Psychol. 2000, 109, 341–344. [Google Scholar] [CrossRef]
- Bryant, R.A.; Kenny, L.; Rawson, N.; Cahill, C.; Joscelyne, A.; Garber, B.; Tockar, J.; Tran, J.; Dawson, K. Two-year follow-up of trauma-focused cognitive behavior therapy for post-traumatic stress disorder in emergency service personnel: A randomized clinical trial. Depress. Anxiety 2021, 38, 1131–1137. [Google Scholar] [CrossRef]
- Buckby, J.A.; Yung, A.R.; Cosgrave, E.M.; Killackey, E.J. Clinical utility of the Mood and Anxiety Symptom Questionnaire (MASQ) in a sample of young help-seekers. BMC Psychiatry 2007, 7, 50. [Google Scholar] [CrossRef]
- Carroll, C.P.; Cochran, J.A.; Price, J.P.; Guse, C.E.; Wang, M.C. The AIS-2005 Revision in Severe Traumatic Brain Injury: Mission Accomplished or Problems for Future Research? Ann. Adv. Automot. Med. 2010, 54, 233–238. [Google Scholar]
- Choi, Y.; Moon, E.; Park, J.M.; Lee, B.D.; Lee, Y.M.; Jeong, H.J.; Chung, Y.I. Psychometric Properties of the Coping Inventory for Stressful Situations in Korean Adults. Psychiatry Investig. 2017, 14, 427–433. [Google Scholar] [CrossRef]
- Chossegros, L.; Hours, M.; Charnay, P.; Bernard, M.; Fort, E.; Boisson, D.; Sancho, P.O.; Yao, S.N.; Laumon, B. Predictive factors of chronic post-traumatic stress disorder 6 months after a road traffic accident. Accid. Anal. Prev. 2011, 43, 471–477. [Google Scholar] [CrossRef]
- Clapp, J.D.; Beck, J.G. An Examination of the Glover Numbing Scale: Expanding the Content Validity of Post-traumatic Numbing. J. Psychopathol. Behav. Assess. 2009, 31, 256–263. [Google Scholar] [CrossRef]
- Coles, T.; Coon, C.; DeMuro, C.; McLeod, L.; Gnanasakthy, A. Psychometric evaluation of the Sheehan Disability Scale in adult patients with attention-deficit/hyperactivity disorder. Neuropsychiatr. Dis. Treat. 2014, 10, 887–895. [Google Scholar] [CrossRef] [PubMed]
- Coronas, R.; Garcia-Pares, G.; Viladrich, C.; Santos, J.M.; Menchon, J.M. Clinical and sociodemographic variables associated with the onset of post-traumatic stress disorder in road traffic accidents. Depress. Anxiety 2008, 25, E16–E23. [Google Scholar] [CrossRef] [PubMed]
- Mirabolfathi, V.; Moradi, A.R.; Jobson, L. Influence of affective distractors on working memory capacity in relation to symptoms of post-traumatic stress disorder. Appl. Cogn. Psychol. 2019, 33, 904–910. [Google Scholar] [CrossRef]
- Davidson, J.R.T.; Tharwani, H.M.; Connor, K.M. Davidson Trauma Scale (DTS): Normative scores in the general population and effect sizes in placebo-controlled SSRI trials. Depress. Anxiety 2002, 15, 75–78. [Google Scholar] [CrossRef]
- Ehring, T.; Ehlers, A.; Glucksman, E. Do cognitive models help in predicting the severity of post-traumatic stress disorder, phobia, and depression after motor vehicle accidents? A prospective longitudinal study. J. Consult. Clin. Psychol. 2008, 76, 219. [Google Scholar] [CrossRef]
- Diagnostic and Statistical Manual of Mental Disorders, 4th ed.; American Psychiatric Publishing, Inc.: Washington, DC, USA, 1995.
- Fecteau, G.; Nicki, R. Cognitive Behavioural Treatment of Post Traumatic Stress Disorder after Motor Vehicle Accident. Behav. Cogn. Psychother. 1999, 27, 201–214. [Google Scholar] [CrossRef]
- Fedroff, I.; Taylor, S.; Asmundson, G.; Koch, W. Cognitive factors in traumatic stress reactions: Predicting PTSD symptoms from anxiety sensitivity and beliefs about harmful events. Behav. Cogn. Psychother. 2000, 28, 5–15. [Google Scholar] [CrossRef]
- Fekadu, W.; Mekonen, T.; Belete, H.; Belete, A.; Yohannes, K. Incidence of Post-Traumatic Stress Disorder After Road Traffic Accident. Front. Psychiatry 2019, 10, 519. [Google Scholar] [CrossRef]
- Feki, R.; Zouari, L.; Majdoub, Y.; Omri, S.; Gassara, I.; Smaoui, N.; Bouali, M.M.; Ben Thabet, J.; Charfi, N.; Maalej, M. Prevalence and predictors of post-traumatic stress disorder in road traffic accidents. Pan Afr. Med. J. 2024, 47, 89. [Google Scholar] [CrossRef]
- Figlerski, L.J. Perceived Control in Automobile Accidents and the Development of Symptoms Related to Post-Traumatic Stress Disorder. Ph.D. Thesis, Hofstra University, Hempstead, NY, USA, 1989. Available online: https://www.proquest.com/openview/fa817b6bd1b915ea66ed605b68b854a3 (accessed on 18 November 2023).
- Fort, E.; Pelissier, C.; Fanjas, A.; Charnay, P.; Charbotel, B.; Bergeret, A.; Fontana, L.; Hours, M. Road casualties in work-related and private contexts: Occupational medical impact. Results from the ESPARR cohort. Work 2018, 60, 117–128. [Google Scholar] [CrossRef]
- Ghanizadeh, A.; Tavassoli, M. Gender comparison of exposed trauma and post-traumatic stress disorder in a community sample of adolescents. J. Trauma Nurs. JTN 2007, 14, 165–169. [Google Scholar] [CrossRef] [PubMed]
- Gidron, Y.; Gal, R.; Freedman, S.; Twiser, I.; Lauden, A.; Snir, Y.; Benjamin, J. Translating research findings to PTSD prevention: Results of a randomized-controlled pilot study. J. Trauma. Stress. 2001, 14, 773–780. [Google Scholar] [CrossRef] [PubMed]
- Gittins, C.B.; Paterson, H.M.; Sharpe, L. How does immediate recall of a stressful event affect psychological response to it? J. Behav. Ther. Exp. Psychiatry 2015, 46, 19–26. [Google Scholar] [CrossRef] [PubMed]
- Hekimoğlu, Y.; Sari, M.; Taştekin, B.; Asirdizer, M. Late psychiatric consequences in disability patients injured in traffic accidents. East. J. Med. 2022, 27, 281–288. [Google Scholar] [CrossRef]
- Holeva, V.; Tarrier, N.; Wells, A. Prevalence and predictors of acute stress disorder and PTSD following road traffic accidents: Thought control strategies and social support. Behav. Ther. 2001, 32, 65–83. [Google Scholar] [CrossRef]
- Hours, M.; Chossegros, L.; Charnay, P.; Tardy, H.; Nhac-Vu, H.T.; Boisson, D.; Luaute, J.; Laumon, B. Outcomes one year after a road accident: Results from the ESPARR cohort. Accid. Anal. Prev. 2013, 50, 92–102. [Google Scholar] [CrossRef]
- Hovens, J.E.; van de Weerd, M. Post-traumatic stress disorder in debriefed survivors of a bus accident. Psychol. Rep. 1998, 82, 1075–1081. [Google Scholar] [CrossRef]
- Iyadurai, L.; Blackwell, S.E.; Meiser-Stedman, R.; Watson, P.; Bonsall, M.B.; Geddes, J.R.; Holmes, E.A. Preventing intrusive memories after trauma via a brief intervention involving Tetris gameplay in the emergency department: A proof-of-concept randomized controlled trial. Mol. Psychiatry 2018, 23, 674–682. [Google Scholar] [CrossRef]
- Jeavons, S. Predicting who suffers psychological trauma in the first year after a road accident. Behav. Res. Ther. 2000, 38, 499–508. [Google Scholar] [CrossRef]
- Jones, C.; Harvey, A.G.; Brewin, C.R. Traumatic brain injury, dissociation, and post-traumatic stress disorder in road traffic accident survivors. J. Trauma Stress. 2005, 18, 181–191. [Google Scholar] [CrossRef]
- Jones, C.; Harvey, A.G.; Brewin, C.R. The organization and content of trauma memories in survivors of road traffic accidents. Behav. Res. Ther. 2007, 45, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Keshet, H.; Foa, E.B.; Gilboa-Schechtman, E. Women’s self-perceptions in the aftermath of trauma: The role of trauma-centrality and trauma-type. Psychol. Trauma 2019, 11, 542–550. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Ressler, K.J.; House, S.L.; Beaudoin, F.L.; An, X.; Stevens, J.S.; Zeng, D.; Neylan, T.C.; Linnstaedt, S.D.; Germine, L.T.; et al. Sociodemographic and trauma-related predictors of PTSD within 8 weeks of a motor vehicle collision in the AURORA study. Mol. Psychiatry 2021, 26, 3108–3121. [Google Scholar] [CrossRef] [PubMed]
- Khati, I.; Hours, M.; Charnay, P.; Chossegros, L.; Tardy, H.; Nhac-Vu, H.T.; Boisson, D.; Laumon, B. Quality of life one year after a road accident: Results from the adult ESPARR cohort. J. Trauma Acute Care Surg. 2013, 74, 301–311. [Google Scholar] [CrossRef]
- Khodadadi-Hassankiadeh, N.; Dehghan-Nayeri, N.; Shahsavari, H.; Yousefzadeh-Chabok, S.; Haghani, H. Psychosocial and Mental Variables and Post-Traumatic Stress Disorder in Traffic Accident Survivors in Northern Iran. Bull. Emerg. Trauma 2017, 5, 197–220. [Google Scholar]
- Kim, W.H.; Cho, S.E.; Hong, J.P.; Kim, H.; Maeng, S.; Kang, J.M.; Na, K.S.; Oh, S.H.; Park, J.W.; Bae, J.N.; et al. Effectiveness of virtual reality exposure treatment for post-traumatic stress disorder due to motor vehicle or industrial accidents. Virtual Real. 2022, 26, 1539–1549. [Google Scholar] [CrossRef]
- Kovacevic, J.; Miskulin, M.; Degmecic, D.; Vcev, A.; Leovic, D.; Sisljagic, V.; Simic, I.; Palenkic, H.; Vcev, I.; Miskulin, I. Predictors of Mental Health Outcomes in Road Traffic Accident Survivors. J. Clin. Med. 2020, 9, 309. [Google Scholar] [CrossRef]
- Kramer, U.; Ceschi, G.; Van der Linden, M.; Bodenmann, G. Individual and Dyadic Coping Strategies in the Aftermath of a Traumatic Experience. Swiss J. Psychol. 2005, 64, 241–248. [Google Scholar] [CrossRef]
- Krzemieniecki, A.; Gabriel, K.I. Stigmatization of post-traumatic stress disorder is altered by PTSD Knowledge and the precipitating trauma of the sufferer. J. Ment. Health 2021, 30, 447–453. [Google Scholar] [CrossRef]
- Li, X.; Sun, L.; Li, Q.; Wang, L. Prediction of post-traumatic stress disorder by acute stress disorder in traffic accident survivors. Turk. J. Med. Sci. 2021, 51, 2502–2509. [Google Scholar] [CrossRef]
- Lowinger, T.; Solomon, Z. Ptsd, Guilt, and Shame among Reckless Drivers. J. Loss Trauma 2004, 9, 327–344. [Google Scholar] [CrossRef]
- Mairean, C. Driving cognitions, rumination, and post-traumatic stress disorder in road traffic accidents survivors. Clin. Psychol. Psychother. 2019, 26, 47–54. [Google Scholar] [CrossRef]
- Matthews, L.R. Work potential of road accident survivors with post-traumatic stress disorder. Behav. Res. Ther. 2005, 43, 483. [Google Scholar] [CrossRef] [PubMed]
- Mayou, R.A.; Black, J.; Bryant, B. Unconsciousness, amnesia and psychiatric symptoms following road traffic accident injury. Br. J. Psychiatry 2000, 177, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Medhaffar, K.; Feki, I.; Baati, I.; Sellami, R.; Trigui, D.; Moalla, S.; Keskes, H.; Masmoudi, J. Post-traumatic stress disorder, anxiety and depression in victims of road traffic accidents. Eur. Psychiatry 2016, 33, S640. [Google Scholar]
- Miller, H.R.; Goldberg, J.O.; Streiner, D.L. What’s in a name? The MMPI-2 PTSD scales. J. Clin. Psychol. 1995, 51, 626–631. [Google Scholar] [CrossRef]
- Murray, J.; Ehlers, A.; Mayou, R.A. Dissociation and post-traumatic stress disorder: Two prospective studies of road traffic accident survivors. Br. J. Psychiatry 2002, 180, 363–368. [Google Scholar] [CrossRef]
- Nightingale, J.; Williams, R.M. Attitudes to emotional expression and personality in predicting post-traumatic stress disorder. Br. J. Clin. Psychol. 2000, 39, 243–254. [Google Scholar] [CrossRef]
- Nilsen, A.S.; Blix, I.; Leknes, S.; Ekeberg, O.; Skogstad, L.; Endestad, T.; Ostberg, B.C.; Heir, T. Brain Activity in Response to Trauma-specific, Negative, and Neutral Stimuli. A fMRI Study of Recent Road Traffic Accident Survivors. Front. Psychol. 2016, 7, 1173. [Google Scholar] [CrossRef]
- Olaya, B.; Alonso, J.; Atwoli, L.; Kessler, R.C.; Vilagut, G.; Haro, J.M. Association between traumatic events and post-traumatic stress disorder: Results from the ESEMeD-Spain study. Epidemiol. Psychiatr. Sci. 2015, 24, 172–183. [Google Scholar] [CrossRef]
- Piltan, M.; Moradi, A.R.; Choobin, M.H.; Azadfallah, P.; Eskandari, S.; Hitchcock, C. Impaired autobiographical memory flexibility in Iranian trauma survivors with post-traumatic stress disorder. Clin. Psychol. Sci. 2021, 9, 294–301. [Google Scholar] [CrossRef] [PubMed]
- Rabe, S.; Dorfel, D.; Zollner, T.; Maercker, A.; Karl, A. Cardiovascular correlates of motor vehicle accident related post-traumatic stress disorder and its successful treatment. Appl. Psychophysiol. Biofeedback 2006, 31, 315–330. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, S.M.; Glover, H.; Ohlde, C.; Mercer, R.; Hamlin, C.; Goodnick, P.; Perez-Rivera, M.I. Relationship of Numbing to Alexithymia, Apathy, and Depression. Psychol. Rep. 2001, 88, 189–200. [Google Scholar] [CrossRef]
- Ratnani, D. Study of post traumatic stress disorder among survivors of road traffic accident. Int. J. Health Sci. 2022, 6, 3762–3767. [Google Scholar] [CrossRef]
- Roitman, P.; Gilad, M.; Ankri, Y.L.; Shalev, A.Y. Head injury and loss of consciousness raise the likelihood of developing and maintaining PTSD symptoms. J. Trauma Stress. 2013, 26, 727–734. [Google Scholar] [CrossRef]
- Roussis, P. Metacognitive Factors in Post-Traumatic Stress Disorder (PTSD); The University of Manchester: Manchester, UK, 2007; Available online: https://www.proquest.com/openview/6c103bb6e9c481d6ff637927b3520961/1?pq-origsite=gscholar&cbl=2026366 (accessed on 2 November 2023).
- Sadeghi-Bazargani, H.; Shahedifar, N.; Somi, M.H.; Poustchi, H.; Bazargan-Hejazi, S.; Jafarabadi, M.A.; Sadeghi, V.; Golestani, M.; Pourasghar, F.; Mohebbi, I. PERSIAN Traffic Safety and Health Cohort: A study protocol on postcrash mental and physical health consequences. Inj. Prev. 2022, 28, 269–279. [Google Scholar] [CrossRef]
- Sescosse, M.G.; Blázquez, F.P.; Arocena, F.L.; Campos, T.G. A pilot study of post-traumatic growth training for patients with post-traumatic stress disorder. Int. J. Psychol. Psychol. Ther. 2018, 18, 235–246. [Google Scholar]
- Sun, Y.-W.; Hu, H.; Wang, Y.; Ding, W.-N.; Chen, X.; Wan, J.-Q.; Zhou, Y.; Wang, Z.; Xu, J.-R. Inter-hemispheric functional and anatomical connectivity abnormalities in traffic accident-induced PTSD: A study combining fMRI and DTI. J. Affect. Disord. 2015, 188, 80–88. [Google Scholar] [CrossRef]
- Veazey, C.H.; Blanchard, E.B.; Hickling, E.J.; Buckley, T.C. Physiological Responsiveness of Motor Vehicle Accident Survivors with Chronic Post-traumatic Stress Disorder. Appl. Psychophysiol. Biofeedback 2004, 29, 51–62. [Google Scholar] [CrossRef]
- Walshe, D.G.; Lewis, E.J.; Kim, S.I.; O’Sullivan, K.; Wiederhold, B.K. Exploring the use of computer games and virtual reality in exposure therapy for fear of driving following a motor vehicle accident. CyberPsychol. Behav. 2003, 6, 329–334. [Google Scholar] [CrossRef]
- Wan, X.; Lan, C.; Chen, J.; Wang, W.; Zhang, H.; Li, L. Creative arts program as an intervention for PTSD: A randomized clinical trial with motor vehicle accident survivors. Int. J. Clin. Exp. Med. 2015, 8, 13585–13591. [Google Scholar]
- Wu, K.; Chan, S.; Yiu, V.F. Psychometric properties and confirmatory factor analysis of the post-traumatic stress disorder checklist for Chinese survivors of road traffic accidents. East Asian Arch. Psychiatry 2008, 18, 144. [Google Scholar]
- Yasan, A.; Guzel, A.; Tamam, Y.; Ozkan, M. Predictive factors for acute stress disorder and post-traumatic stress disorder after motor vehicle accidents. Psychopathology 2009, 42, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Zoellner, T.; Rabe, S.; Karl, A.; Maercker, A. Post-traumatic growth in accident survivors: Openness and optimism as predictors of its constructive or illusory sides. J. Clin. Psychol. 2008, 64, 245–263. [Google Scholar] [CrossRef]
- Clark, E.; Burkett, K.; Stanko-Lopp, D. Let Evidence Guide Every New Decision (LEGEND): An evidence evaluation system for point-of-care clinicians and guideline development teams. J. Eval. Clin. Pract. 2009, 15, 1054–1060. [Google Scholar] [CrossRef]
- Booth, A.; Sutton, A.; Papaioannou, D. Systematic Approaches to a Successful Literature Review, 2nd ed.; SAGE Publications: Thousand Oaks, CA, USA, 2016. [Google Scholar]
- World Health Organisation. 2022. Available online: https://www.who.int/health-topics/road-safety (accessed on 22 October 2023).
- Yohannes, K.; Gebeyehu, A.; Adera, T.; Ayano, G.; Fekadu, W. Prevalence and correlates of post-traumatic stress disorder among survivors of road traffic accidents in Ethiopia. Int. J. Ment. Health Syst. 2018, 12, 50. [Google Scholar] [CrossRef]
- Wetzel, R.D.; Murphy, G.E.; Simons, A.; Lustman, P.; North, C.; Yutzy, S. What does the Keane PTSD scale of the MMPI measure? Repeated measurements in a group of patients with major depression. Psychol. Rep. 2003, 92, 781–786. [Google Scholar] [CrossRef]
- Weathers, F.W.; Keane, T.M.; Davidson, J.R. Clinician-Administered PTSD Scale: A review of the first ten years of research. Depress. Anxiety 2001, 13, 132–156. [Google Scholar] [CrossRef]
- Kobak, K.A. The Hamilton Depression Rating Scale (HAMD). In Comprehensive Handbook of Psychological Assessment, Vol. 2: Personality Assessment; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2004; pp. 87–98. [Google Scholar]
- Foa, E.B.; McLean, C.P.; Zang, Y.; Zhong, J.; Rauch, S.; Porter, K.; Knowles, K.; Powers, M.B.; Kauffman, B.Y. Psychometric properties of the Post-traumatic Stress Disorder Symptom Scale Interview for DSM–5 (PSSI–5). Psychol. Assess. 2016, 28, 1159. [Google Scholar] [CrossRef]
- Wu, K.K.; Leung, P.W.; Cho, V.W.; Law, L.S. Post-traumatic Growth After Motor Vehicle Crashes. J. Clin. Psychol. Med. Settings 2016, 23, 181–191. [Google Scholar] [CrossRef]
- Wu, K.K.; Li, F.W.; Cho, V.W. A randomized controlled trial of the effectiveness of brief-CBT for patients with symptoms of post-traumatic stress following a motor vehicle crash. Behav. Cogn. Psychother. 2014, 42, 31–47. [Google Scholar] [CrossRef] [PubMed]
- Weathers, F.W.; Blake, D.D.; Schnurr, P.P.; Kaloupek, D.G.; Marx, B.P.; Keane, T.M. The Life Events Checklist for DSM-5 (LEC-5). 2013. Available online: https://www.ptsd.va.gov/professional/assessment/te-measures/life_events_checklist.asp (accessed on 19 November 2023).
- World Health Organisation. Composite International Diagnostic Interview (CIDI), Version 2.1; World Health Organisation: Geneva, Switzerland, 1994. [Google Scholar]
- van Bruggen, V.; Ten Klooster, P.M.; van der Aa, N.; Smith, A.J.M.; Westerhof, G.J.; Glas, G. Structural Validity of the World Assumption Scale. J. Trauma Stress. 2018, 31, 816–825. [Google Scholar] [CrossRef] [PubMed]
- Foa, E.B.; Ehlers, A.; Clark, D.M.; Tolin, D.F.; Orsillo, S.M. The Post-traumatic Cognitions Inventory (PTCI): Development and validation. Psychol. Assess. 1999, 11, 303–314. [Google Scholar] [CrossRef]
- Kocalevent, R.D.; Berg, L.; Beutel, M.E.; Hinz, A.; Zenger, M.; Härter, M.; Nater, U.; Brähler, E. Social support in the general population: Standardization of the Oslo social support scale (OSSS-3). BMC Psychol. 2018, 6, 31. [Google Scholar] [CrossRef]
- Mayou, R.A.; Ehlers, A.; Hobbs, M. Psychological debriefing for road traffic accident victims: Three-year follow-up of a randomized controlled trial. Br. J. Psychiatry 2002, 180, 287–293. [Google Scholar] [CrossRef]
- Daneshvar, S.; Taghavi, M.R.; Jobson, L. Proactive Interference in Post-traumatic Stress Disorder. J. Trauma Stress. 2021, 34, 641–653. [Google Scholar] [CrossRef]
- Beck, J.G.; Grant, D.M.; Read, J.P.; Clapp, J.D.; Coffey, S.F.; Miller, L.M.; Palyo, S.A. The impact of event scale-revised: Psychometric properties in a sample of motor vehicle accident survivors. J. Anxiety Disord. 2008, 22, 187–198. [Google Scholar] [CrossRef]
- Ehring, T.; Ehlers, A. Does rumination mediate the relationship between emotion regulation ability and post-traumatic stress disorder? Eur. J. Psychotraumatol. 2014, 5, 23547. [Google Scholar] [CrossRef]
- Ehlers, A.; Taylor, J.E.; Ehring, T.; Hofmann, S.G.; Deane, F.P.; Roth, W.T.; Podd, J.V. The Driving Cognitions Questionnaire: Development and preliminary psychometric properties. J. Anxiety Disord. 2007, 21, 493–509. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, H.; Wang, J.; Wu, J.; Liu, X. Prevalence and predictors of post-traumatic growth in accidentally injured patients. J. Clin. Psychol. Med. Settings 2013, 20, 3–12. [Google Scholar] [CrossRef]
- World Health Organisation. The World Health Organization Quality of Life (WHOQOL)–BREF. 2004. Available online: https://apps.who.int/iris/handle/10665/77773 (accessed on 28 October 2023).
- Brewin, C.R.; Rose, S.; Andrews, B.; Green, J.; Tata, P.; McEvedy, C.; Turner, S.; Foa, E.B. Brief screening instrument for post-traumatic stress disorder. Br. J. Psychiatry 2002, 181, 158–162. [Google Scholar] [CrossRef] [PubMed]
- Guest, R.; Tran, Y.; Gopinath, B.; Cameron, I.D.; Craig, A. Prevalence and psychometric screening for the detection of major depressive disorder and post-traumatic stress disorder in adults injured in a motor vehicle crash who are engaged in compensation. BMC Psychol. 2018, 6, 4. [Google Scholar] [CrossRef] [PubMed]
- Taylor, S.; Cox, B.J. An expanded Anxiety Sensitivity Index: Evidence for a hierarchic structure in a clinical sample. J. Anxiety Disord. 1998, 12, 463–483. [Google Scholar] [CrossRef] [PubMed]
- Brackett, M.A.; Salovey, P. Measuring emotional intelligence with the Mayer-Salovery-Caruso Emotional Intelligence Test (MSCEIT). Psicothema 2006, 18, 34–41. [Google Scholar]
- Butcher, J.N.; Atlis, M.M.; Hahn, J. The Minnesota Multiphasic Personality Inventory-2 (MMPI-2). In Comprehensive Handbook of Psychological Assessment, Vol. 2: Personality Assessment; John Wiley & Sons, Inc.: Hoboken, NJ, USA, 2004; pp. 30–38. [Google Scholar]
- Zimet, G.D.; Dahlem, N.W.; Zimet, S.G.; Farley, G.K. The Multidimensional Scale of Perceived Social Support. J. Personal. Assess. 1988, 52, 30–41. [Google Scholar] [CrossRef]
- Osman, A.; Wong, J.L.; Bagge, C.L.; Freedenthal, S.; Gutierrez, P.M.; Lozano, G. The Depression Anxiety Stress Scales—21 (DASS-21): Further examination of dimensions, scale reliability, and correlates. J. Clin. Psychol. 2012, 68, 1322–1338. [Google Scholar] [CrossRef]
- London, K.; Bruck, M.; Melnyk, L. Post-event information affects children’s autobiographical memory after one year. Law Hum. Behav. 2009, 33, 344–355. [Google Scholar] [CrossRef]
- Shmueli, A. The Visual Analog rating Scale of health-related quality of life: An examination of end-digit preferences. Health Qual. Life Outcomes 2005, 3, 71. [Google Scholar] [CrossRef]
- Zhu, W.; Wei, Y.; Meng, X.; Li, J. The mediation effects of coping style on the relationship between social support and anxiety in Chinese medical staff during COVID-19. BMC Health Serv. Res. 2020, 20, 1007. [Google Scholar] [CrossRef]
- Javali, R.H.; Krishnamoorthy Patil, A.; Srinivasarangan, M.; Suraj; Sriharsha. Comparison of Injury Severity Score, New Injury Severity Score, Revised Trauma Score and Trauma and Injury Severity Score for Mortality Prediction in Elderly Trauma Patients. Indian J. Crit. Care Med. 2019, 23, 73–77. [Google Scholar] [CrossRef]
- Keller, M.B.; Lavori, P.W.; Friedman, B.; Nielsen, E.; Endicott, J.; McDonald-Scott, P.; Andreasen, N.C. The Longitudinal Interval Follow-up Evaluation. A comprehensive method for assessing outcome in prospective longitudinal studies. Arch. Gen. Psychiatry 1987, 44, 540–548. [Google Scholar] [CrossRef] [PubMed]
- Sarason, I.G.; Levine, H.M.; Basham, R.B.; Sarason, B.R. Assessing social support: The Social Support Questionnaire. J. Personal. Soc. Psychol. 1983, 44, 127–139. [Google Scholar] [CrossRef]
- Wells, A.; Davies, M.I. The Thought Control Questionnaire: A measure of individual differences in the control of unwanted thoughts. Behav. Res. Ther. 1994, 32, 871–878. [Google Scholar] [CrossRef] [PubMed]
- Hinz, A.; Singer, S.; Brähler, E. European reference values for the quality of life questionnaire EORTC QLQ-C30: Results of a German investigation and a summarizing analysis of six European general population normative studies. Acta Oncol. 2014, 53, 958–965. [Google Scholar] [CrossRef]
- Abbott, R.A.; Ploubidis, G.B.; Huppert, F.A.; Kuh, D.; Croudace, T.J. An Evaluation of the Precision of Measurement of Ryff’s Psychological Well-Being Scales in a Population Sample. Soc. Indic. Res. 2010, 97, 357–373. [Google Scholar] [CrossRef]
- Smith, B.; Mackenzie-Ross, S.; Scragg, P. Prevalence of poor psychological morbidity following a minor road traffic accident (RTA): The clinical implications of a prospective longitudinal study. Couns. Psychol. Q. 2007, 20, 149–155. [Google Scholar] [CrossRef]
- Mayou, R.; Bryant, B.; Duthie, R. Psychiatric consequences of road traffic accidents. Br. Med. J. 1993, 307, 647–651. [Google Scholar] [CrossRef]
- Brunet, A.; Weiss, D.S.; Metzler, T.J.; Best, S.R.; Neylan, T.C.; Rogers, C.; Fagan, J.; Marmar, C.R. The Peritraumatic Distress Inventory: A proposed measure of PTSD criterion A2. Am. J. Psychiatry 2001, 158, 1480–1485. [Google Scholar] [CrossRef]
- Weathers, F.W.; Bovin, M.J.; Lee, D.J.; Sloan, D.M.; Schnurr, P.P.; Kaloupek, D.G.; Keane, T.M.; Marx, B.P. The Clinician-Administered PTSD Scale for DSM-5 (CAPS-5): Development and initial psychometric evaluation in military veterans. Psychol. Assess. 2018, 30, 383–395. [Google Scholar] [CrossRef]
- Galatzer-Levy, I.R.; Huang, S.H.; Bonanno, G.A. Trajectories of resilience and dysfunction following potential trauma: A review and statistical evaluation. Clin. Psychol. Rev. 2018, 63, 41–55. [Google Scholar] [CrossRef]
- Weathers, F.W.; Litz, B.T.; Keane, T.M.; Palmieri, P.A.; Marx, B.P.; Schnurr, P.P. The PTSD Checklist for DSM-5 (PCL-5). 2013. Available online: https://www.ptsd.va.gov (accessed on 15 September 2023).
| Study | Year | Country/Region | LEGEND | Study Design | Primary Methodology | Notes |
|---|---|---|---|---|---|---|
| Adawi et al. [18] | 2019 | Italy | 3B | Psychometric | Quantitative | Brief Symptom Inventory in nomophobic subjects |
| Angerpointner et al. [19] | 2020 | Germany | 3B | Prospective | Quantitative | PTSD after minor trauma |
| Asmundson et al. [20] | 1999 | Canada | 3B | Psychometric Study | Quantitative | Accident Fear Questionnaire validation |
| Asuquo et al. [21] | 2017 | Nigeria | 4B | Case-control | Quantitative | PTSD vs. controls post-RTA |
| Aykaç et al. [22] | 2024 | Turkey | 4A | Cross-sectional | Quantitative | Post-traumatic growth after RTA |
| Bae et al. [23] | 2014 | Korea | 3B | Cross-sectional | Quantitative | Memory function and PTSD |
| Bae et al. [24] | 2015 | Korea | 4B | Cross-sectional | Quantitative | Forgiveness as PTSD mediator |
| Baptie et al. [25] | 2021 | UK | 2B | RCT | Mixed Methods | VR intervention for trauma recovery |
| Barth et al. [26] | 2005 | Germany | 3B | Longitudinal | Quantitative | PTSD and psychosocial impairments |
| Beck et al. [27] | 2006 | USA | 3B | Experimental | Quantitative | Thought suppression post-RTA |
| Beck et al. [28] | 2007 | USA | 4B | Case Series | Mixed Methods | Virtual Reality Exposure Therapy |
| Bedaso et al. [29] | 2020 | Ethiopia | 3B | Prospective | Quantitative | PTSD prevalence among survivors |
| Benjamin et al. [30] | 2010 | USA | 3B | Experimental | Quantitative | Subjective distress in anxious youth |
| Berntsen & Rubin [31] | 2006 | USA | 3A | Psychometric | Quantitative | Centrality of event scale for trauma |
| Blanchard et al. [32] | 1996 | USA | 3B | Prospective | Quantitative | PTSD remission after 1 year |
| Blanchard et al. [33] | 2003 | USA | 3B | Experimental | Quantitative | Prediction of response to therapy |
| Blanchard & Buckley [34] | 1998 | USA | 3B | Prospective | Quantitative | Psychophysiological changes after RTA |
| Blanchard & Hickling [35] | 2004 | USA | 3B | Book | Qualitative | Assessment and treatment post-MVA |
| Boccia et al. [11] | 2015 | Italy | 1B | Meta-analysis | Quantitative | EMDR treatment efficacy for RTA survivors |
| Boelen et al. [36] | 2024 | Netherlands | 3B | Survey | Mixed Methods | Preferences for PTSD treatment modes |
| Brand et al. [37] | 2014 | Germany | 3A | Cross-sectional | Quantitative | PTSD incidence after RTAs |
| Briere et al. [38] | 1995 | USA | 4A | Psychometric | Quantitative | Trauma Symptom Inventory validation |
| Brom et al. [39] | 1993 | Netherlands | 3B | Cross-sectional | Mixed Methods | Counselling outcomes post-RTA |
| Bryant et al. [40] | 2000 | Australia | 4A | Prospective | Quantitative | Acute stress predicting PTSD |
| Bryant et al. [41] | 2021 | Australia | 2A | RCT | Mixed Methods | Brief vs. long CBT exposure therapies |
| Buckby et al. [42] | 2007 | Australia | 3B | Psychometric | Quantitative | MASQ validation in youth |
| Carroll et al. [43] | 2010 | USA | 3B | Review | Quantitative | AIS revision for brain injury research |
| Choi et al. [44] | 2017 | South Korea | 3B | Psychometric | Quantitative | Coping Inventory validation |
| Chossegros et al. [45] | 2011 | France | 3A | Cohort | Quantitative | PTSD at 6 months post-RTA |
| Clapp & Beck [46] | 2009 | USA | 3B | Psychometric | Quantitative | Glover Numbing Scale examination |
| Coles et al. [47] | 2014 | USA | 4A | Psychometric | Quantitative | Evaluation of Sheehan Disability Scale |
| Coronas et al. [48] | 2008 | Spain | 4B | Cross-sectional | Quantitative | PTSD onset in RTA survivors |
| Daddah et al. [12] | 2022 | Benin | 3B | Cross-sectional | Quantitative | PTSD risk factors post-RTA |
| Daneshvar et al. [49] | 2021 | Iran | 3B | Experimental | Quantitative | Positive emotion intervention on memory |
| Davidson et al. [50] | 2002 | USA | 4A | Psychometric | Quantitative | Norms for Davidson Trauma Scale |
| Ehring et al. [51] | 2008 | UK | 3B | Experimental | Quantitative | Memory updating in PTSD |
| Ehring & Ehlers [52] | 2014 | UK | 4A | Experimental | Quantitative | Rumination and PTSD symptoms |
| Fecteau & Nicki [53] | 1999 | Canada | 2B | RCT | Quantitative | CBT for PTSD post-MVA |
| Fedroff et al. [54] | 2000 | Canada | 4A | Experimental | Quantitative | CBT impact on anxiety sensitivity |
| Fekadu et al. [55] | 2019 | Ethiopia | 3B | Cross-sectional | Quantitative | PTSD impacts on work and life |
| Feki et al. [56] | 2024 | Tunisia | 4B | Cross-sectional | Quantitative | Gender differences in PTSD risk |
| Figlerski et al. [57] | 1989 | USA | 3B | Survey | Quantitative | Anxiety after minor RTAs |
| Fort et al. [58] | 2018 | France | 4A | Prospective | Quantitative | Return to work predictors post-RTA |
| Ghanizadeh & Tavassoli [59] | 2007 | Iran | 3B | Community Study | Quantitative | Adolescents’ PTSD symptoms |
| Gidron et al. [60] | 2001 | Israel | 3B | RCT (pilot) | Mixed Methods | Memory intervention (Mem-Flex) |
| Gittins et al. [61] | 2015 | UK | 3B | RCT | Quantitative | Writing about trauma vs. non-recall task |
| Guest et al. [26] | 2018 | Australia | 4B | Psychometric | Quantitative | DASS-21 and IES-R post-RTA |
| Hekimoglu et al. [62] | 2022 | Turkey | 3B | Longitudinal | Quantitative | PTSD prevalence at 7 years post-RTA |
| Holeva et al. [63] | 2001 | UK | 3A | Cross-sectional | Quantitative | Acute stress and social support |
| Hours et al. [64] | 2013 | France | 3A | Longitudinal | Quantitative | Severe injury and relational impact |
| Hovens & van de Weerd [65] | 1998 | Netherlands | 3B | Prospective | Quantitative | Hyperarousal predicting PTSD |
| Iyadurai [66] | 2015 | UK | 2B | RCT | Quantitative | Cognitive task to reduce intrusive memories |
| Jeavons [67] | 2000 | UK | 3B | Prospective | Quantitative | PTSD and subsyndromal PTSD at 1 year |
| Jones et al. [68] | 2005 | UK | 3A | Prospective | Quantitative | TBI and PTSD prediction |
| Jones et al. [69] | 2007 | UK | 2B | Qualitative | Mixed Methods | Trauma memory organization post-RTA |
| Keshet et al. [70] | 2019 | Israel | 4B | Cross-sectional | Quantitative | Self-perceptions post-RTA trauma |
| Kessler et al. [71] | 2021 | USA | 4A | Prospective | Quantitative | Trauma predictors of PTSD post-MVA |
| Khati et al. [72] | 2013 | France | 2B | Cohort | Quantitative | Quality of life post-RTA |
| Khodadadi-Hassankiadeh et al. [73] | 2017 | Iran | 3A | Cross-sectional | Quantitative | Depression, amnesia, PTSD |
| Kim et al. [74] | 2022 | Korea | 3A | Cohort | Mixed Methods | VR Exposure Therapy vs. control group |
| Koren et al. [7] | 2001 | Israel | 4A | Longitudinal | Quantitative | Chronic PTSD over 3 years |
| Kovacevic et al. [75] | 2020 | Croatia | 3A | Cross-sectional | Quantitative | Predictors of PTSD and mental health |
| Kramer et al. [76] | 2005 | Switzerland | 4B | Cross-sectional | Quantitative | Dyadic coping post-trauma |
| Krzemieniecki & Gabriel [77] | 2021 | USA | 3A | Survey | Quantitative | Stigma and trauma type comparison |
| Leroy et al. [6] | 2022 | France | 2B | Cohort | Quantitative | PTSD prevalence after 1 year |
| Li et al. [78] | 2021 | China | 4A | Prospective | Quantitative | Acute Stress Disorder predicting PTSD |
| Lin et al. [9] | 2018 | China | 3B | Meta-analysis | Quantitative | PTSD prevalence meta-analysis |
| Lowinger & Solomon [79] | 2004 | Israel | 3B | Cross-sectional | Quantitative | Self-blame in reckless drivers |
| Mairean [80] | 2019 | Romania | 3A | Survey | Quantitative | Driving cognitions and rumination |
| Matthews [81] | 2005 | Australia | 3B | Cross-sectional | Quantitative | Work limitations with PTSD post-RTA |
| Mayou et al. [82] | 2000 | UK | 3B | Longitudinal | Quantitative | Unconsciousness and PTSD symptoms |
| Medhaffar et al. [83] | 2016 | Tunisia | 4A | Cross-sectional | Quantitative | Injury type and PTSD development |
| Miller et al. [84] | 1995 | USA | 3B | Psychometric | Quantitative | MMPI-2 PTSD scale assessment |
| Mirabolfathi et al. [49] | 2019 | Iran | 4A | Experimental | Quantitative | Affective distractors and memory |
| Murray et al. [85] | 2002 | UK | 3A | Prospective | Quantitative | Injury severity predicting PTSD |
| Nightingale & Williams [86] | 2000 | UK | 4A | Cross-sectional | Quantitative | PTSD and emotional expression |
| Nilsen et al. [87] | 2016 | Norway | 3B | fMRI Study | Quantitative | Brain activation in PTSD post-RTA |
| Olaya et al. [88] | 2015 | Spain | 3B | Survey | Quantitative | Sociodemographic predictors of PTSD |
| Piltan et al. [89] | 2021 | Iran | 2A | Experimental | Quantitative | Memory flexibility and PTSD |
| Ponniah & Hollon [10] | 2009 | USA | 2A | Review (of RCTs) | Quantitative | Treatment efficacy for PTSD |
| Rabe et al. [90] | 2006 | Germany | 2A | Physiological Study | Quantitative | Heart rate reactivity and PTSD |
| Ramirez et al. [91] | 2001 | USA | 4A | Survey | Quantitative | Numbing, apathy, and depression |
| Ratnani [92] | 2022 | India | 3A | Cross-sectional | Quantitative | PTSD prevalence within 1 year |
| Roitman et al. [93] | 2013 | Israel | 3B | Cross-sectional | Quantitative | Unconsciousness and PTSD risk |
| Roussis [94] | 2007 | UK | 3B | Thesis | Quantitative | Metacognitive factors in PTSD |
| Sadeghi-Bazargani et al. [95] | 2022 | Iran | 4A | Cohort | Quantitative | PTSD prevalence at 1 month post-RTA |
| Sescosse et al. [96] | 2018 | USA | 2B | RCT | Quantitative | Post-traumatic growth and recovery |
| Smith et al. [5] | 1997 | UK | 3A | Prospective | Quantitative | PTSD prevalence at 6 weeks post-RTA |
| Sun et al. [97] | 2015 | China | 4B | Neuroimaging Study | Quantitative | Corpus callosum changes in PTSD |
| Veazey et al. [98] | 2004 | USA | 5A | Psychophysiological | Quantitative | Heart rate in PTSD survivors |
| Walshe et al. [99] | 2015 | China | 3B | Cohort | Quantitative | Art therapy for PTSD post-RTA |
| Wan et al. [100] | 2015 | China | 3B | RCT | Mixed Methods | Art therapy for PTSD post-RTA |
| Wu et al. [101] | 2014 | China | 2A | RCT | Mixed Methods | CBT vs. self-help booklet intervention |
| Yasan et al. [102] | 2019 | Turkey | 3A | Longitudinal | Quantitative | PTSD trajectory over a year |
| Yimer et al. [13] | 2023 | Ethiopia | 3B | Cross-sectional | Quantitative | PTSD comorbidity rates |
| Zoellner et al. [103] | 2008 | Switzerland | 4A | Cross-sectional | Quantitative | Post-traumatic growth and PTSD |
| Country of Publication (n = 96) | |
|---|---|
| Country of publication | Number of studies |
| USA | 22 |
| UK | 13 |
| Iran | 6 |
| China | 6 |
| France | 5 |
| Australia | 5 |
| Israel | 5 |
| Germany | 5 |
| Netherlands | 3 |
| Korea | 3 |
| Ethiopia | 3 |
| Turkey | 3 |
| Canada | 3 |
| Switzerland | 2 |
| Tunisia | 2 |
| Italy | 2 |
| Spain | 2 |
| Benin | 1 |
| Croatia | 1 |
| South Korea | 1 |
| Nigeria | 1 |
| Romania | 1 |
| Norway | 1 |
| India | 1 |
| Year of publication | Number of studies (%) (n = 96) |
| −1999 | 10 (10.4%) |
| 2000–2010 | 34 (35.4%) |
| 2011–2024 | 54 (56.2%) |
| Sample Characteristics | |
|---|---|
| Number of participants included in all studies | 50,275 |
| Information about psychological treatments | Number of studies (%) (n = 96) |
| No information about participants having any kind of psychological treatment after the accident | 77 (80.2%) |
| Studies that report that participants have some psychological treatment after the accident | 21 (21.9%) |
| Patient type | Number of studies (%) (n = 96) |
| Hospitalized after a Road Traffic Accident | 31 (32.3%) |
| Not hospitalized after the Road Traffic Accident | 67 (69.8%) |
| Used Scales for PTSD (Original Author) | Number (%) of Studies (n = 96) | Studies Using the Scale |
|---|---|---|
| PTSD Checklist-(PCL-5) [107] | 26 studies (27.1%) | [4,5,6,12,13,29,30,34,45,56,64,75,77,78,80,81,84,89,90,93,95,96,107,108,109,110] |
| Clinician-Administered PTSD Scale (CAPS) [111] | 24 studies (25%) | [4,5,6,12,18,21,44,49,58,63,71,74,78,82,105,106,107,112,113,114,115,116,117,118] |
| PTSD Symptom Scale—Interview, PSS-I-5 scale [119] | 15 studies (15.6%) | [27,36,56,67,68,69,71,73,76,81,82,93,96,108,120] |
| PTSD Symptom Scale Self-Report Version (PSS-SR) [121] | 4 studies (4.2%) | [7,54,65,86] |
| Post-traumatic Diagnostic Scale [5] | 3 studies (3.1%) | [70,85,122] |
| Mississippi PTSD Scale for Civilians [112] | 2 studies (2.1%) | [50,60] |
| Davidson Trauma Scale (DTS) [123] | 1 study (1%) | [120] |
| Used Scales (Original Author) | Number (%) of Studies (n = 96) | Studies Using the Scale |
|---|---|---|
| The Impact of Event Scale (Revised IES-R) [124] | 17 studies (17.7%) | [7,23,31,34,36,55,71,75,92,97,103,108,111,119,124,125,126] |
| Beck depression and anxiety inventories [124] | 9 studies (9.4%) | [7,19,23,27,39,49,53,57,61,67,74,94,97,100,101,124,127] |
| Motor Vehicle Accident Interview (MVA) Interview [36] | 4 studies (4.2%) | [33,46,54,63] |
| Post Traumatic Growth Inventory [128] | 4 studies (4.2%) | [19,22,34,96] |
| The State-Trait Anxiety Inventory (STAI) [129] | 3 studies (3.1%) | [25,33,98] |
| The Peritraumatic Dissociative Experiences Questionnaire [130] | 2 studies (2.1%) | [102,124] |
| Anxiety Sensitivity Index [131] | 1 study (1%) | [61] |
| Mayer-Salovery-Caruso Emotional Intelligence Test (MSCEIT) [115] | 1 study (1%) | [46] |
| The Minnesota Multiphasic Personality Inventory-2 (MMPI-2) [132] | 1 study (1%) | [64] |
| The Multidimensional Scale of Perceived Social Support [133] | 1 study (1%) | [23] |
| Composite International Diagnostic Interview (CIDI) [116] | 1 study (1%) | [41] |
| The Depression Anxiety Stress Scales—21 (DASS-21) [117] | 1 study (1%) | [61] |
| Post event information (PEI) [134] | 1 study (1%) | [61] |
| Coping Inventory for Stressful Situations [45] | 1 study (1%) | [68] |
| World Assumption Scale [135] | 1 study (1%) | [67] |
| The Centrality of Event Scale [32] | 1 study (1%) | [70] |
| The Post-traumatic Cognitions Inventory (PTCI) [136] | 1 study (1%) | [70] |
| The Driving Cognitions Questionnaire [114] | 1 study (1%) | [80] |
| The visual analog rating scale of health-related quality of life [137] | 1 study (1%) | [107] |
| Mood and Anxiety Symptom Questionnaire (MASQ) [43] | 1 study (1%) | [107] |
| Trait Coping Style Scale [138] | 1 study (1%) | [119] |
| The Abbreviated Injury Scale (AIS) [44] | 1 study (1%) | [119] |
| Glover Numbing Scale [92] | 1 study (1%) | [46] |
| Injury Severity Score [139] | 1 study (1%) | [103] |
| The Longitudinal Interval Follow-up Evaluation (LIFE) [140] | 1 study (1%) | [33] |
| Brief Symptom Inventory [19] | 1 study (1%) | [33] |
| The Social Support Questionnaire [118] | 1 study (1%) | [63] |
| The Thought Control Questionnaire [141] | 1 study (1%) | [63] |
| The Accident Fear Questionnaire [21] | 1 study (1%) | [53] |
| Trauma Symptom Inventory [39] | 1 study (1%) | [39] |
| The quality of life questionnaire [142] | 1 study (1%) | [95] |
| Oslo social support scale (OSSS-3) [125] | 1 study (1%) | [13] |
| Sheehan Disability Scale [48] | 1 study (1%) | [13] |
| Scale of Psychological Well-being [113] | 1 study (1%) | [96] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Trajchevska, M.; Jones, C.M. Post-Traumatic Stress Disorder (PTSD) Resulting from Road Traffic Accidents (RTA): A Systematic Literature Review. Int. J. Environ. Res. Public Health 2025, 22, 985. https://doi.org/10.3390/ijerph22070985
Trajchevska M, Jones CM. Post-Traumatic Stress Disorder (PTSD) Resulting from Road Traffic Accidents (RTA): A Systematic Literature Review. International Journal of Environmental Research and Public Health. 2025; 22(7):985. https://doi.org/10.3390/ijerph22070985
Chicago/Turabian StyleTrajchevska, Marija, and Christian Martyn Jones. 2025. "Post-Traumatic Stress Disorder (PTSD) Resulting from Road Traffic Accidents (RTA): A Systematic Literature Review" International Journal of Environmental Research and Public Health 22, no. 7: 985. https://doi.org/10.3390/ijerph22070985
APA StyleTrajchevska, M., & Jones, C. M. (2025). Post-Traumatic Stress Disorder (PTSD) Resulting from Road Traffic Accidents (RTA): A Systematic Literature Review. International Journal of Environmental Research and Public Health, 22(7), 985. https://doi.org/10.3390/ijerph22070985





