The Role of Testing and Vaccination in Mediating Social Vulnerability and COVID-19 Prevalence in Southern Nevada
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Area
2.2. Data Sources
2.3. Statistical Analyses
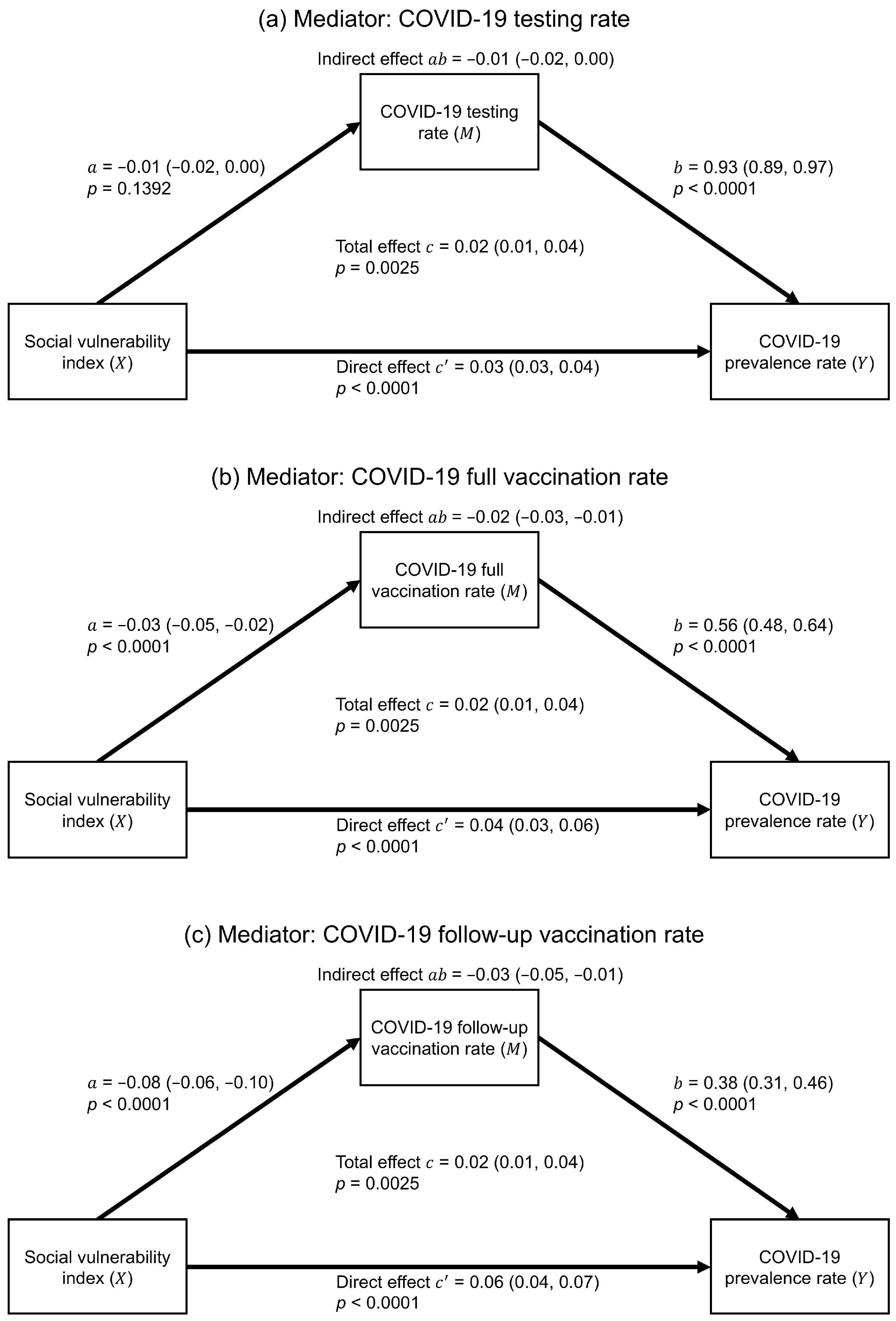
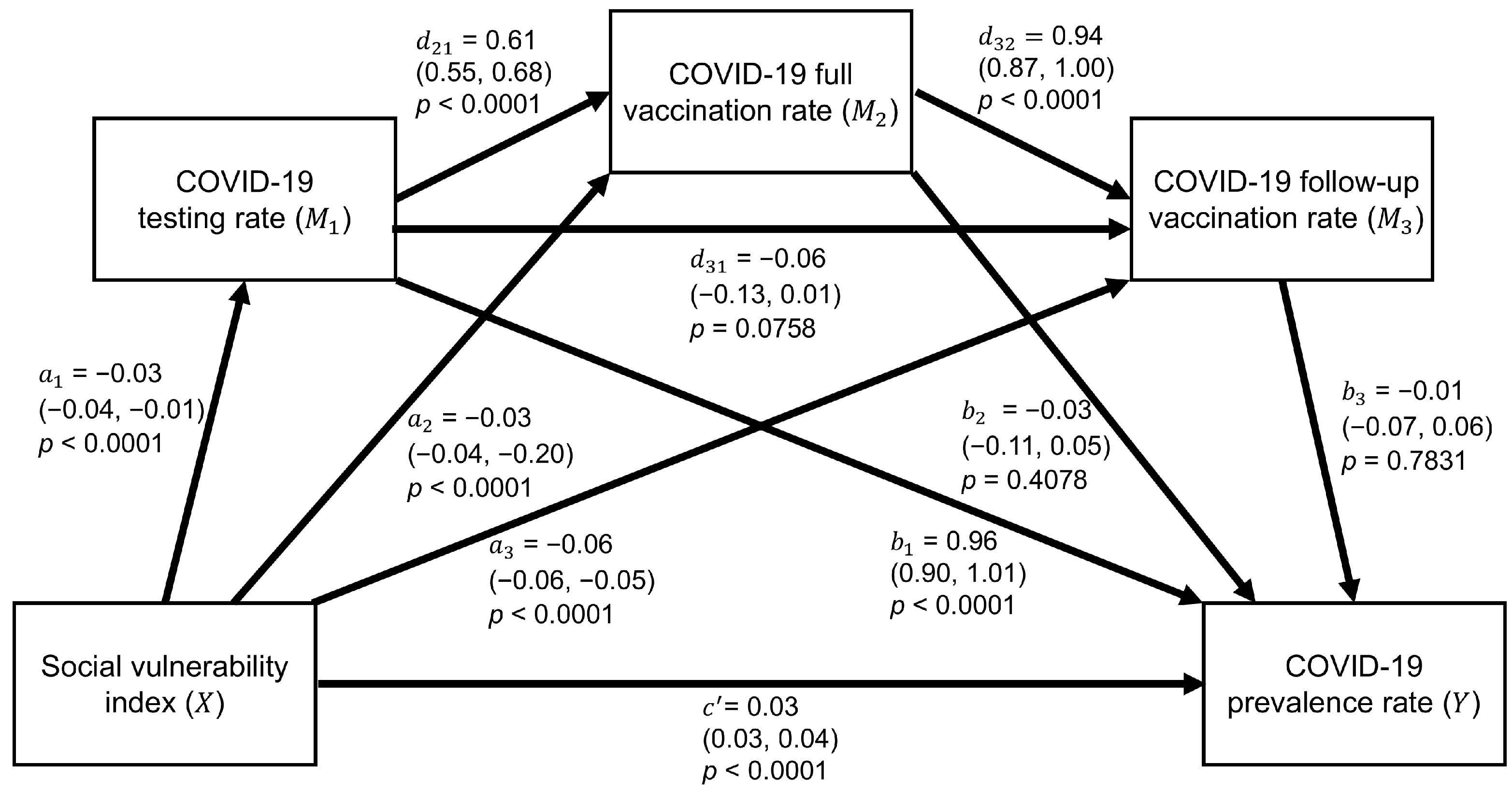
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Stokes, E.K.; Zambrano, L.D.; Anderson, K.N.; Marder, E.P.; Raz, K.M.; El Burai Felix, S.; Tie, Y.; Fullerton, K.E. Coronavirus Disease 2019 Case Surveillance—United States, January 22–May 30, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 759–765. [Google Scholar] [CrossRef] [PubMed]
- Sawyer, C.; Marshall, J. Income Inequality Linked to Social Vulnerability to Disasters. PreventionWeb 2024. Available online: https://www.preventionweb.net/news/income-inequality-linked-social-vulnerability-disasters (accessed on 29 July 2024).
- Wolkin, A.; Collier, S.; House, J.S.; Reif, D.; Motsinger-Reif, A.; Duca, L.; Sharpe, J.D. Comparison of National Vulnerability Indices Used by the Centers for Disease Control and Prevention for the COVID-19 Response. Public Health Rep. 2022, 137, 803–812. [Google Scholar] [CrossRef] [PubMed]
- Flanagan, B.E.; Gregory, E.W.; Hallisey, E.J.; Heitgerd, J.L.; Lewis, B. A Social Vulnerability Index for Disaster Management. J. Homel. Secur. Emerg. 2011, 8, 0000102202154773551792. [Google Scholar] [CrossRef]
- Schmidt, H.; Weintraub, R.; Williams, M.A.; Miller, K.; Buttenheim, A.; Sadecki, E.; Wu, H.; Doiphode, A.; Nagpal, N.; Gostin, L.O.; et al. Equitable Allocation of COVID-19 Vaccines in the United States. Nat. Med. 2021, 27, 1298–1307. [Google Scholar] [CrossRef]
- Al Rifai, M.; Jain, V.; Khan, S.U.; Nasir, K.; Zhu, D.; Vasudeva, R.; Lavie, C.J.; Dodani, S.; Petersen, L.A.; Virani, S.S. Social Vulnerability and COVID-19: An Analysis of CDC Data. Prog. Cardiovasc. Dis. 2022, 73, 91–93. [Google Scholar] [CrossRef]
- Bilal, U.; Tabb, L.P.; Barber, S.; Roux, A.V.D. Spatial Inequities in COVID-19 Testing, Positivity, Confirmed Cases, and Mortality in 3 U.S. Cities: An Ecological Study. Ann. Intern. Med. 2021, 174, 936–944. [Google Scholar] [CrossRef]
- Ali, S.; Asaria, M.; Stranges, S. COVID-19 and Inequality: Are We All in This Together? Can. J. Public Health 2020, 111, 415–416. [Google Scholar] [CrossRef]
- DuPre, N.C.; Karimi, S.; Zhang, C.H.; Blair, L.; Gupta, A.; Alharbi, L.M.A.; Alluhibi, M.; Mitra, R.; McKinney, W.P.; Little, B. County-Level Demographic, Social, Economic, and Lifestyle Correlates of COVID-19 Infection and Death Trajectories During the First Wave of the Pandemic in the United States. Sci. Total Environ. 2021, 786, 147495. [Google Scholar] [CrossRef]
- Paul, A.; Englert, P.; Varga, M. Socio-Economic Disparities and COVID-19 in the USA. J. Phys. Complex. 2021, 2, 035017. [Google Scholar] [CrossRef]
- Bhowmik, T.; Tirtha, S.D.; Iraganaboina, N.C.; Eluru, N.A. Comprehensive Analysis of COVID-19 Transmission and Mortality Rates at the County Level in the United States Considering Socio-Demographics, Health Indicators, Mobility Trends, and Health Care Infrastructure Attributes. PLoS ONE 2021, 16, e0249133. [Google Scholar] [CrossRef]
- Sung, B. A Spatial Analysis of the Association Between Social Vulnerability and the Cumulative Number of Confirmed Deaths from COVID-19 in United States Counties Through November 14, 2020. Osong Public Health Res. Perspect. 2021, 12, 149–157. [Google Scholar] [CrossRef] [PubMed]
- Dasgupta, S.; Bowen, V.B.; Leidner, A.; Fletcher, K.; Musial, T.; Rose, C.; Cha, A.; Kang, G.; Dirlikov, E.; Pevzner, E.; et al. Association Between Social Vulnerability and a County’s Risk for Becoming a COVID-19 Hotspot—United States, June 1-July 25, 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 1535–1541. [Google Scholar] [CrossRef] [PubMed]
- Hughes, M.M.; Wang, A.; Grossman, M.K.; Pun, E.; Whiteman, A.; Deng, L.; Hallisey, E.; Sharpe, J.D.; Ussery, E.N.; Stokley, S.; et al. County-Level COVID-19 Vaccination Coverage and Social Vulnerability—United States, December 14, 2020-March 1, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 431–436. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.S.; Brown, A.F.; Washington, D.L. Inclusion of Race and Ethnicity with Neighborhood Socioeconomic Deprivation When Assessing COVID-19 Hospitalization Risk Among California Veterans Health Administration Users. JAMA Netw. Open 2023, 6, e231471. [Google Scholar] [CrossRef]
- Megahed, F.M.; Jones-Farmer, L.A.; Ma, Y.; Rigdon, S.E. Explaining the Varying Patterns of COVID-19 Deaths Across the United States: 2-Stage Time Series Clustering Framework. JMIR Public Health Surveill. 2022, 8, e32164. [Google Scholar] [CrossRef]
- van Ingen, T.; Brown, K.A.; Buchan, S.A.; Akingbola, S.; Daneman, N.; Warren, C.M.; Smith, B.T.; Varga, C. Neighbourhood-Level Socio-Demographic Characteristics and Risk of COVID-19 Incidence and Mortality in Ontario, Canada: A Population-Based Study. PLoS ONE 2022, 17, e0276507. [Google Scholar] [CrossRef]
- Zegarra Zamalloa, C.O.; Contreras, P.J.; Orellana, L.R.; Riega Lopez, P.A.; Prasad, S.; Cuba Fuentes, M.S. Social Vulnerability During the COVID-19 Pandemic in Peru. PLoS Glob. Public Health 2022, 2, e0001330. [Google Scholar] [CrossRef]
- Oates, G.R.; Juarez, L.D.; Horswell, R.; Chu, S.; Miele, L.; Fouad, M.N.; Curry, W.A.; Fort, D.; Hillegass, W.B.; Danos, D.M. The Association Between Neighborhood Social Vulnerability and COVID-19 Testing, Positivity, and Incidence in Alabama and Louisiana. J. Community Health 2021, 46, 1115–1123. [Google Scholar] [CrossRef]
- Troppy, S.; Wilt, G.E.; Whiteman, A.; Hallisey, E.; Crockett, M.; Sharpe, J.D.; Haney, G.; Cranston, K.; Klevens, R.M. Geographic Associations Between Social Factors and SARS-CoV-2 Testing Early in the COVID-19 Pandemic, February–June 2020, Massachusetts. Public Health Rep. 2021, 136, 765–773. [Google Scholar] [CrossRef]
- Donadio, G.; Choudhary, M.; Lindemer, E.; Pawlowski, C.; Soundararajan, V. Counties with Lower Insurance Coverage and Housing Problems Are Associated with Both Slower Vaccine Rollout and Higher COVID-19 Incidence. Vaccines 2021, 9, 973. [Google Scholar] [CrossRef]
- Khairat, S.; Zou, B.; Adler-Milstein, J. Factors and Reasons Associated with Low COVID-19 Vaccine Uptake Among Highly Hesitant Communities in the US. Am. J. Infect. Control 2022, 50, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Thakore, N.; Khazanchi, R.; Orav, E.J.; Ganguli, I. Association of Social Vulnerability, COVID-19 Vaccine Site Density, and Vaccination Rates in the United States. Healthcare 2021, 9, 100583. [Google Scholar] [CrossRef]
- Ali, R.; Samin, P. Higher COVID-19 Vaccination Rates among Unemployed in the United States: State-Level Study in the First 100 Days of Vaccine Initiation. medRxiv 2021, medRxiv:2021.04.17.21255668. [Google Scholar] [CrossRef]
- King, W.C.; Rubinstein, M.; Reinhart, A.; Mejia, R. COVID-19 Vaccine Hesitancy January-May 2021 Among 18–64 Year Old US Adults by Employment and Occupation. Prev. Med. Rep. 2021, 24, 101569. [Google Scholar] [CrossRef] [PubMed]
- Diesel, J.; Sterrett, N.; Dasgupta, S.; Kriss, J.L.; Barry, V.; Esschert, K.V.; Whiteman, A.; Cadwell, B.L.; Weller, D.; Qualters, J.R.; et al. COVID-19 Vaccination Coverage Among Adults—United States, December 14, 2020-May 22, 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 922–927. [Google Scholar] [CrossRef]
- Kriss, J.L.; Hung, M.C.; Srivastav, A.; Black, C.L.; Lindley, M.C.; Lee, J.T.; Koppaka, R.; Tsai, Y.; Lu, P.-J.; Yankey, D.; et al. COVID-19 Vaccination Coverage, by Race and Ethnicity—National Immunization Survey Adult COVID Module, United States, December 2020-November 2021. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 757–763. [Google Scholar] [CrossRef]
- Mody, A.; Bradley, C.; Redkar, S.; Fox, B.; Eshun-Wilson, I.; Hlatshwayo, M.G.; Trolard, A.; Tram, K.H.; Filiatreau, L.M.; Thomas, F.; et al. Quantifying Inequities in COVID-19 Vaccine Distribution Over Time by Social Vulnerability, Race and Ethnicity, and Location: A Population-Level Analysis in St. Louis and Kansas City, Missouri. PLoS Med. 2022, 19, e1004048. [Google Scholar] [CrossRef]
- Baack, B.N.; Abad, N.; Yankey, D.; Kahn, K.E.; Razzaghi, H.; Brookmeyer, K.; Kolis, J.; Wilhelm, E.; Nguyen, K.H.; Singleton, J.A. COVID-19 Vaccination Coverage and Intent Among Adults Aged 18-39 Years—United States, March-May 2021. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 928–933. [Google Scholar] [CrossRef]
- Assefa, Y.; Gilks, C.F.; Reid, S.; van de Pas, R.; Gete, D.G.; Van Damme, W. Analysis of the COVID-19 Pandemic: Lessons Towards a More Effective Response to Public Health Emergencies. Glob. Health 2022, 18, 10. [Google Scholar] [CrossRef]
- Rosenberg, E.S.; Dufort, E.M.; Blog, D.S.; Hall, E.W.; Hoefer, D.; Backenson, B.P.; Muse, A.T.; Kirkwood, J.N.; George, K.S.; Holtgrave, D.R.; et al. COVID-19 Testing, Epidemic Features, Hospital Outcomes, and Household Prevalence, New York State—March 2020. Clin. Infect. Dis. 2020, 71, 1953–1959. [Google Scholar] [CrossRef]
- Rentsch, C.T.; Kidwai-Khan, F.; Tate, J.P.; Park, L.S.; King, J.T., Jr.; Skanderson, M.; Hauser, R.G.; Schultze, A.; Jarvis, C.I.; Holodniy, M.; et al. Patterns of COVID-19 Testing and Mortality by Race and Ethnicity Among United States Veterans: A Nationwide Cohort Study. PLoS Med. 2020, 17, e1003379. [Google Scholar] [CrossRef] [PubMed]
- Gaffney, A.; Woolhandler, S.; Himmelstein, D.U. COVID-19 Testing and Incidence Among Uninsured and Insured Individuals in 2020: A National Study. J. Gen. Intern. Med. 2022, 37, 1344–1347. [Google Scholar] [CrossRef] [PubMed]
- Kirby, R.P.; Maimaran, M.; Palamountain, K.M. Is There a “Price That’s Right” for At-Home COVID Tests? PLoS ONE 2023, 18, e0282043. [Google Scholar] [CrossRef] [PubMed]
- Rader, B.; Gertz, A.; Iuliano, A.D.; Gilmer, M.; Wronski, L.; Astley, C.M.; Sewalk, K.; Varrelman, T.J.; Cohen, J.; Parikh, R.; et al. Use of At-Home COVID-19 Tests—United States, August 23, 2021–March 12, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 489–494. [Google Scholar] [CrossRef]
- Ferdinands, J.M.; Rao, S.; Dixon, B.E.; Mitchell, P.K.; DeSilva, M.B.; Irving, S.A.; Lewis, N.; Natarajan, K.; Stenehjem, E.; Grannis, S.J.; et al. Waning 2-Dose and 3-Dose Effectiveness of mRNA Vaccines Against COVID-19-Associated Emergency Department and Urgent Care Encounters and Hospitalizations Among Adults During Periods of Delta and Omicron Variant Predominance—VISION Network, 10 States, August 2021-January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 255–263. [Google Scholar] [CrossRef]
- Kuitunen, I.; Uimonen, M.; Seppälä, S.J.; Ponkilainen, V.T. COVID-19 Vaccination Status and Testing Rates in Finland—A Potential Cause for Bias in Observational Vaccine Effectiveness Analysis. Influenza Other Respir. Viruses 2022, 16, 842–845. [Google Scholar] [CrossRef]
- Hayes, A.F. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach; Guilford Publications: New York, NY, USA, 2017. [Google Scholar]
- Bhuiyan, M.A.N.; Davis, T.C.; Arnold, C.L.; Motayar, N.; Bhuiyan, S.; Smith, D.G.; Murnane, K.S.; Densmore, K.; van Diest, M.; Bailey, S.R.; et al. Using the Social Vulnerability Index to Assess COVID-19 Vaccine Uptake in Louisiana. GeoJournal 2023, 88, 3239–3248. [Google Scholar] [CrossRef]
- McPhearson, T.; Grabowski, Z.; Herreros-Cantis, P.; Mustafa, A.; Ortiz, L.; Kennedy, C.; Tomateo, C.; Lopez, B.; Olivotto, V.; Vantu, A. Pandemic Injustice: Spatial and Social Distributions of COVID-19 in the US Epicenter. J. Extreme Events 2020, 7, 2150007. [Google Scholar] [CrossRef]
- Ransome, Y.; Ojikutu, B.O.; Buchanan, M.; Johnston, D.; Kawachi, I. Neighborhood Social Cohesion and Inequalities in COVID-19 Diagnosis Rates by Area-Level Black/African American Racial Composition. J. Urban Health 2021, 98, 222–232. [Google Scholar] [CrossRef]
- Tan, A.X.; Hinman, J.A.; Abdel Magid, H.S.; Nelson, L.M.; Odden, M.C. Association Between Income Inequality and County-Level COVID-19 Cases and Deaths in the US. JAMA Netw. Open. 2021, 4, e218799. [Google Scholar] [CrossRef]
- Backer, S.; Rezene, A.; Kahar, P.; Khanna, D. Socioeconomic Determinants of COVID-19 Incidence and Mortality in Florida. Cureus 2022, 14, e22491. [Google Scholar] [CrossRef] [PubMed]
- Tortolero, G.A.; Otto, M.O.; Ramphul, R.; Yamal, J.M.; Rector, A.; Brown, M.; Peskin, M.F.; Mofleh, D.; Boerwinkle, E. Examining Social Vulnerability and the Association with COVID-19 Incidence in Harris County, Texas. Front. Public Health 2021, 9, 798085. [Google Scholar] [CrossRef]
- Biggs, E.N.; Maloney, P.M.; Rung, A.L.; Peters, E.S.; Robinson, W.T. The Relationship Between Social Vulnerability and COVID-19 Incidence Among Louisiana Census Tracts. Front. Public Health 2020, 8, 617976. [Google Scholar] [CrossRef] [PubMed]
- Ivanov, A.; Mukherjee, U.K.; Bose, S.; Seshadri, S.; Watkins, R.; England, A.C.; Suriano, J.; Ahsen, M.E.; Souyris, S. COVID-19 Test-to-Stay Program for K-12 Schools: Opt-in Versus Opt-out Consent Model. IScience 2024, 27, 108770. [Google Scholar] [CrossRef] [PubMed]
- Dryden-Peterson, S.; Velásquez, G.E.; Stopka, T.J.; Davey, S.; Lockman, S.; Ojikutu, B.O. Disparities in SARS-CoV-2 Testing in Massachusetts During the COVID-19 Pandemic. JAMA Netw. Open 2021, 4, e2037067. [Google Scholar] [CrossRef]
- Mullachery, P.H.; Li, R.; Melly, S.; Kolker, J.; Barber, S.; Roux, A.V.D.; Bilal, U. Inequities in Spatial Accessibility to COVID-19 Testing in 30 Large US Cities. Soc. Sci. Med. 2022, 310, 115307. [Google Scholar] [CrossRef]
- Ferguson, J.M.; Abdel Magid, H.S.; Purnell, A.L.; Kiang, M.V.; Osborne, T.F. Differences in COVID-19 Testing and Test Positivity Among Veterans, United States, 2020. Public Health Rep. 2021, 136, 483–492. [Google Scholar] [CrossRef]
- Iwata, K.; Miyakoshi, C. Is COVID-19 Mortality Associated with Test Number? J. Family Med. Prim. Care 2022, 11, 1842–1844. [Google Scholar] [CrossRef]
- Lieberman-Cribbin, W.; Alpert, N.; Flores, R.; Taioli, E. Analyzing Disparities in COVID-19 Testing Trends According to Risk for COVID-19 Severity Across New York City. BMC Public Health 2021, 21, 1717. [Google Scholar] [CrossRef]
- Khan, M.M.; Odoi, A.; Odoi, E.W. Geographic Disparities in COVID-19 Testing and Outcomes in Florida. BMC Public Health 2023, 23, 79. [Google Scholar] [CrossRef]
- Alphonso, S.R.; Andrews, M.R.; Regan, S.D.; Shishkov, A.; Cantor, J.H.; Powell-Wiley, T.M.; Tamura, K. Geospatially Clustered Low COVID-19 Vaccine Rates among Adolescents in Socially Vulnerable US Counties. Prev. Med. Rep. 2024, 37, 102545. [Google Scholar] [CrossRef]
- Xu, Z.; Jiang, B. Effects of Social Vulnerability and Spatial Accessibility on COVID-19 Vaccination Coverage: A Census-Tract Level Study in Milwaukee County, USA. Int. J. Environ. Res. Public Health 2022, 19, 12304. [Google Scholar] [CrossRef] [PubMed]
- Brown, C.C.; Young, S.G.; Pro, G.C. COVID-19 Vaccination Rates Vary by Community Vulnerability: A County-Level Analysis. Vaccine 2021, 39, 4245–4249. [Google Scholar] [CrossRef] [PubMed]
- Hongru, D.; Samee, S.; Lauren, M.G. Association Between Vaccination Rates and COVID-19 Health Outcomes in the United States: A Population-Level Statistical Analysis. medRxiv 2023. [Google Scholar] [CrossRef]
- Samson, L.W.; Tarazi, W.; Orav, E.J.; Sheingold, S.; De Lew, N.; Sommers, B.D. Associations Between County-Level Vaccination Rates and COVID-19 Outcomes Among Medicare Beneficiaries; ASPE: Office of the Assistant Secretary for Planning and Evaluation: Washington, DC, USA, 2021.
- Walters, G.D. Why Are Mediation Effects So Small? Int. J. Soc. Res. Methodol. 2019, 22, 219–232. [Google Scholar] [CrossRef]
- Satici, B.; Saricali, M.; Satici, S.A.; Griffiths, M.D. Intolerance of Uncertainty and Mental Well-Being: Serial Mediation by Rumination and Fear of COVID-19. Int. J. Ment. Health Addict. 2022, 20, 2731–2742. [Google Scholar] [CrossRef]
- Yang, Y.; Cuffee, Y.L.; Aumiller, B.B.; Schmitz, K.; Almeida, D.M.; Chinchilli, V.M. Serial Mediation Roles of Perceived Stress and Depressive Symptoms in the Association Between Sleep Quality and Life Satisfaction Among Middle-Aged American Adults. Front. Psychol. 2022, 13, 822564. [Google Scholar] [CrossRef]
- Zhao, H.; Xiong, J.; Zhang, Z.; Qi, C. Growth Mindset and College Students’ Learning Engagement During the COVID-19 Pandemic: A Serial Mediation Model. Front. Psychol. 2021, 12, 621094. [Google Scholar] [CrossRef]
- Alfons, A.; Ateş, N.Y.; Groenen, P.J.F. A Robust Bootstrap Test for Mediation Analysis. Organ. Res. Methods 2021, 25, 591–617. [Google Scholar] [CrossRef]
| Variable | Mean | SD | Min. | Q1 | Median | Q3 | Max. |
|---|---|---|---|---|---|---|---|
| Social vulnerability index | 7.79 | 2.55 | 1.45 | 5.74 | 7.64 | 9.90 | 13.33 |
| COVID-19 prevalence rate | 233.45 | 78.58 | 4.40 | 193.29 | 224.66 | 260.02 | 989.26 |
| COVID-19 testing rate | 1851.30 | 757.59 | 49.86 | 1558.21 | 1756.14 | 1995.45 | 12,476.19 |
| COVID-19 full vaccination rate | 611.49 | 808.93 | 45.70 | 492.57 | 546.36 | 616.19 | 17,371.41 |
| COVID-19 follow-up vaccination rate | 281.26 | 124.75 | 0.00 | 213.89 | 260.92 | 323.84 | 1270.61 |
| Variable | COVID-19 Prevalence Rate | COVID-19 Testing Rate | COVID-19 Full Vaccination Rate | COVID-19 Follow-Up Vaccination Rate |
|---|---|---|---|---|
| Social vulnerability index | −0.07 (−0.15, 0.02) | −0.26 (−0.33, −0.18) | −0.13 (−0.21, −0.04) | −0.58 (−0.63, −0.52) |
| COVID-19 prevalence rate | 0.78 (0.75, 0.81) | 0.31 (0.24, 0.39) | 0.55 (0.48, 0.60) | |
| COVID-19 testing rate | 0.71 (0.66, 0.75) | 0.72 (0.67, 0.75) | ||
| COVID-19 full vaccination rate | 0.52 (0.46, 0.58) |
| Path § | Effect §§ | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Total effect () | 0.01 | (0.001, 0.02) | 0.0354 |
| Direct effect () | 0.03 | (0.03, 0.04) | <0.0001 |
| Total indirect effect | −0.02 | (−0.03, −0.002) | - |
| Individual indirect effect 1 | −0.02 | (−0.04, −0.01) | - |
| Individual indirect effect 2 | 0.001 | (−0.01, 0.007) | - |
| Individual indirect effect 3 | 0.001 | (−0.01, 0.02) | - |
| Individual indirect effect 4 | 0.001 | (−0.01, 0.004) | - |
| Individual indirect effect 5 | −0.00 | (−0.002, 0.004) | − |
| Individual indirect effect 6 | 0.0003 | (−0.003, 0.01) | − |
| Individual indirect effect 7 | 0.0001 | (−0.002, 0.01) | − |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lopez, A.; Chien, L.-C.; Chen, L.-W.A.; Coughenour, C.; Marquez, E.; Lee, S.-P. The Role of Testing and Vaccination in Mediating Social Vulnerability and COVID-19 Prevalence in Southern Nevada. Int. J. Environ. Res. Public Health 2025, 22, 980. https://doi.org/10.3390/ijerph22070980
Lopez A, Chien L-C, Chen L-WA, Coughenour C, Marquez E, Lee S-P. The Role of Testing and Vaccination in Mediating Social Vulnerability and COVID-19 Prevalence in Southern Nevada. International Journal of Environmental Research and Public Health. 2025; 22(7):980. https://doi.org/10.3390/ijerph22070980
Chicago/Turabian StyleLopez, Andrea, Lung-Chang Chien, L.-W. Antony Chen, Courtney Coughenour, Erika Marquez, and Szu-Ping Lee. 2025. "The Role of Testing and Vaccination in Mediating Social Vulnerability and COVID-19 Prevalence in Southern Nevada" International Journal of Environmental Research and Public Health 22, no. 7: 980. https://doi.org/10.3390/ijerph22070980
APA StyleLopez, A., Chien, L.-C., Chen, L.-W. A., Coughenour, C., Marquez, E., & Lee, S.-P. (2025). The Role of Testing and Vaccination in Mediating Social Vulnerability and COVID-19 Prevalence in Southern Nevada. International Journal of Environmental Research and Public Health, 22(7), 980. https://doi.org/10.3390/ijerph22070980







